 Facebook
Facebook
 X
X
 Instagram
Instagram
 TikTok
TikTok
 Youtube
Youtube

If you’ve ever had a bad toothache in your upper jaw, you know the general area where the human animal experiences life in its greatest intensity. You can’t get away from the pain because it’s right where you live. Similarly, sufferers of a medical condition called empty-nose syndrome, say they found out the hard way that the area inside of your nose and above the roof of your mouth can provide a baseline sense of well-being — or a complete lack thereof.
“It’s pure, unremitting hell,” says Robert Gerlach, 34, of Lemon Grove, who was diagnosed with empty-nose syndrome following a nasal surgery in 2011. Gerlach, who relocated to the San Diego area from Rochester, New York, two years ago, is like many others who move to the region hoping this is where they will find relief from the rare, but increasingly recognized condition.
It turns out, a common procedure called a turbinectomy or turbinate-reduction surgery in rare cases can cause empty-nose syndrome. Turbinate reductions are frequently performed to treat sleep apnea. That was the reason for Gerlach’s operation.
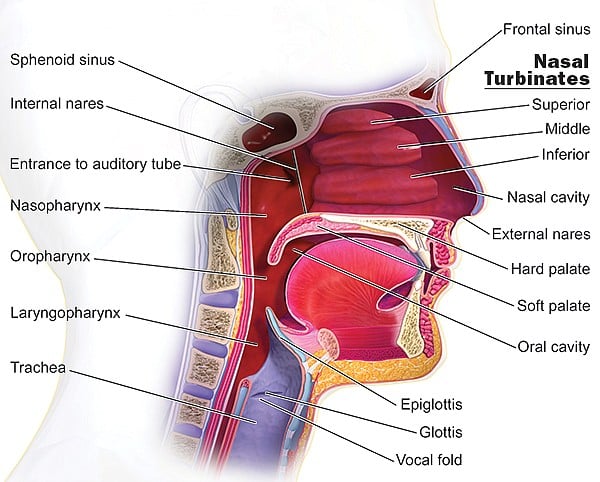
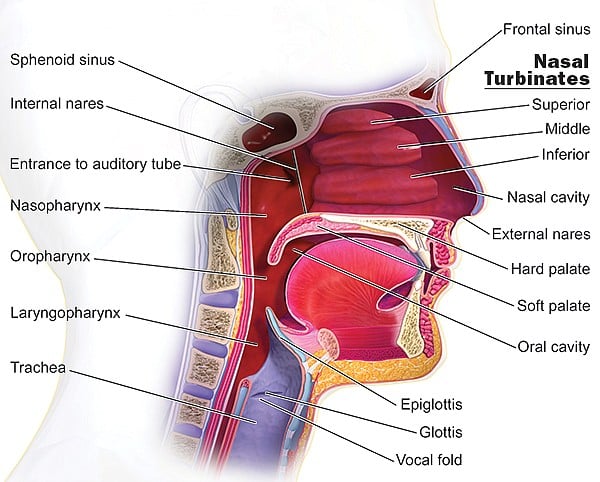
Just above the roof of your mouth and behind the exterior of your nose are a set of three tiers of flesh-covered bones. Each of those tiers is decked out with a pair of structures called nasal turbinates. These are bony, knoblike features inside the “nasal vault.” They are covered with soft tissue made up of epithelium and mucosa that exchange and humidify air, while also warming air to ready it for maximum oxygenation and distribution by the lungs.
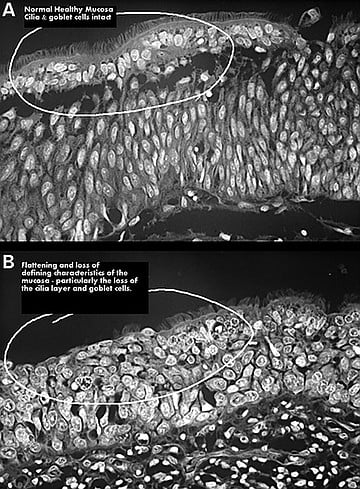
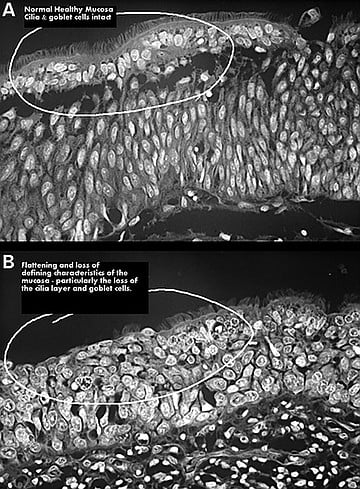
The system of turbinates is a stroke of evolutionary genius, which the American Rhinologic Society says has been key to mammals’ and birds’ ability to adapt to hostile climates. The epithelium, which look like microscopic hairs on the turbinates, allow you to smell and to efficiently breathe through your nose.
Ear, nose, and throat specialists often surgically reduce the size of nasal turbinates on people with chronic breathing problems. Although most turbinate reductions are successful, empty-nose is a rare post-surgery syndrome that leaves its victims feeling permanently “hollowed out” or “zombie-like,” as more than one sufferer described their symptoms to the San Diego Reader.
“This is worse than death,” says Gerlach, who has undergone nearly a dozen subsequent procedures in search of relief following the turbinate operation he says gave him empty-nose syndrome.
Gerlach’s first surgery did nothing to alleviate his obstructive sleep apnea. He says his sleep troubles are worse than ever. Sleep clinics across San Diego, where he frequently undergoes studies, have become his homes away from home.
Put in lay terms, obstructive sleep apnea happens when tissue blocks the respiratory system, encumbering normal sleep. Nasal turbinates are often blamed for such obstructions; so it’s only natural that doctors have, for years, been surgically reducing turbinate tissue.
Most researchers cite a 1993 study published in the New England Journal of Medicine that found 24 percent of men and 9 percent of women in America suffer from obstructive sleep apnea. It’s a condition that can lead to depression, stroke, heart disease — even death. However, there’s little agreement about the success rate of turbinate reduction as a treatment for sleep apnea. Figures range from a 30–90 percent success rate, varying by technique.
Another local empty-nose patient says the fact that he was told he needed nasal surgery to help him breathe better couldn’t have come from further out of left field than it did.
“I didn’t even have a problem breathing or sleeping or anything — not even a deviated septum,” says Nathan Schmidt, 36. He underwent “an overly aggressive” turbinate reduction in 2004 in Boston. “I was young, in a band and thought I’d listen to my friends’ and family’s warnings that loud music was bad for my hearing,” Schmidt says, recalling his decision to get checked out by an ear, nose, and throat specialist as a precautionary measure to protect his hearing.

“I thought I was being proactive,” he says, adding that he now wishes that instead of an ear, nose, and throat doctor he would have seen an audiologist, who would have just tested his hearing.
“Instead, he looked in my nose and said I’d breathe a lot better if I had turbinate-reduction surgery. I told him I didn’t think I had any trouble breathing, to which he replied, ‘You don’t know what normal breathing is because you don’t have any other point of reference.’”
His insurance paid for the turbinectomy to the tune of about $12,000. Starting with losing the ability to play in a band, Schmidt’s life would never be the same. He now lives in Tijuana, where he owns a small business.
He receives care for empty-nose syndrome in San Diego from Deborah Watson, M.D. Watson is an otolaryngology (ear, nose, and throat) surgeon and professor of surgery at UCSD. She is considered one of the nation’s foremost experts on empty-nose syndrome. He praises Watson for diagnosing his post-surgery travails as empty-nose syndrome and for helping him find modest relief.
How many people suffer from empty-nose syndrome? No one knows because there’s never been an effort to find out.
“It’s not in their interest to bring this up,” says Gerlach, referring to the otolaryngology profession. “Turbinate reductions are the most common surgery they do; they don’t even tell you it can cause empty-nose.”
Compared to Gerlach’s, Schmidt’s condition is mild. In fact, Schmidt says his is among the mildest he’s heard of among a growing community of sufferers who seek solutions, advice, and share news of potential new treatments with one another via social media. Yet, even for Schmidt, having empty-nose is a rough way to live.
“It’s tough, but some days are better than others,” Schmidt says. “I’m a naturally outgoing, well-adjusted person. I went to Juilliard and had a very active social life before empty-nose syndrome. But when my nose is bad, which is well over half the time, I feel miserable, tired, and anxious, and don’t want to go out. It’s difficult making plans; like if I’m invited to something, I’ll instantly think, If my nose is bad that day, I’ll not want to go, and if I do go and look miserable people will think it’s because I don’t like them. Having said that, I try to see it as just a disability and keep in mind all the other aspects of myself, like my intellect and health otherwise, that it doesn’t affect.”
Serious respiratory issues are part of what defines empty-nose. But Schmidt is the recipient of a highly prized rarity among sufferers: a medical procedure that restored a modicum of feeling like he “can breathe right.”
“I had two separate cartilage implants performed by Deborah Watson at UCSD Medical Center,” he says. “They were both beneficial, but by no means a cure. I had the first implant about 11 years ago.”
But many sufferers believe there is an effort by the ear, nose, and throat medical establishment to stifle awareness of their condition. They say turbinate-reduction surgeries are quick, easy ways to generate revenue with little risk. One sufferer says there’s a “turbinectomy industrial complex.”
“Most people come out of turbinate-reduction surgery fine,” says Gerlach. “The problem is you aren’t told what the risk is.”
Ear, nose, and throat doctors deny being cavalier about turbinate reductions or that there is a tacit conspiracy to ratchet up revenue by overprescribing the procedures.
Meanwhile, Gerlach’s sojourn for relief from symptoms that range from a constant feeling of suffocation and exhaustion to anxiety and memory loss has taken him from coast to coast and back again. He says even sympathetic ear, nose, and throat doctors are loath to talk about empty-nose syndrome.
“I’d be very surprised if you could get any of these doctors to talk to you about empty-nose syndrome in the media,” Gerlach says.
Indeed, physicians in the local otolaryngology community contacted by the San Diego Reader were mostly unwilling to discuss empty-nose syndrome.
As well as being home to a top-notch, albeit sometimes media-shy, medical community with expertise on empty-nose syndrome, there’s another reason sufferers settle in San Diego.
“The salt in the air is better for my nose, and the climate is more consistent, which makes it somewhat easier to breathe than artificially heated air,” Gerlach says, adding that he had hoped San Diego’s vibrant biotech and stem-cell industries might offer a new solution.
He dreams that one day he’ll wake up to a headline announcing that one of San Diego’s famous life science companies has developed a therapy to regenerate nasal tissue. Until then, there’s our mild climate.
“I feel worse in hot and humid weather,” says Nathan Schmidt. “I always sleep with an air conditioner. Cool, dry air helps stimulate mucous production. San Diego and Tijuana weather for me isn’t so bad. I used to live in Boston, where the summers were intolerable.”
Schmidt and Gerlach feel there’s a crucial difference between sufficient respiration, which they and most empty-nose sufferers technically have, versus the satisfaction and sense of well-being that comes with the sensation of breathing normally.
“I would put the nonrespiratory symptoms of empty-nose syndrome into two categories,” Schmidt explains. “The first is missing everyday sensations of the nose. Most people take it for granted, but nasal sensitivity is a consistent source of pleasure. Even though it’s associated with being sick and congested, when you sneeze you get a shot of pleasure, or like when you breathe deeply through the nose or meditate, it’s relaxing.”
Schmidt says he never knew how key to being happy the feeling of having a functioning nose was until it was gone. He thinks he’d do almost anything to feel “nice, normal nasal congestion again.”
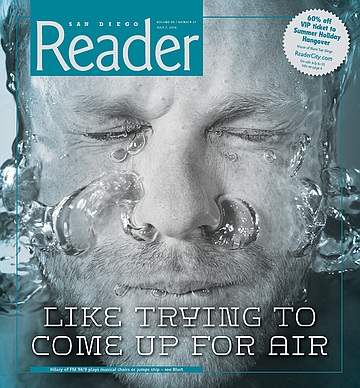
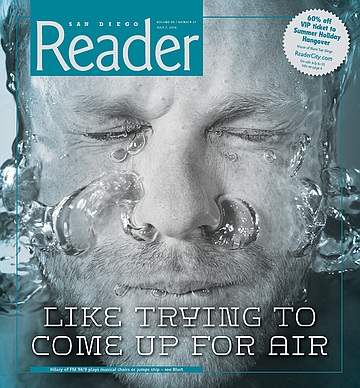
Asked to describe the sensation of the syndrome, Schmidt askes me to imagine “the panic that sets in when you hold your breath for too long, like trying to come up for air in the water, but you’ve way underestimated how deep in the pool you are.”
He continues, “I’m convinced that part of the patient’s brain literally thinks that he is not breathing, due to the nose not sensing airflow even if air is going in,” he continues. “[Your] nose goes from being a source of pleasure to a source of anxiety. For a lot of patients, including myself before my first corrective surgery was done by Dr. Watson, it’s so unbearable that they resort to plugging their noses, wishing they didn’t have a nose at all.”
Noting that empty-nose patients have committed suicide because of the condition, a recent Buzzfeed article with the headline, “Is Empty Nose Syndrome Real, and if not, Why are People Killing Themselves Over It?” cited an academic paper by Dr. Spencer Payne of the University of Virginia. “The problem with empty-nose syndrome is probably not that it does not exist,” Dr. Spencer says. “It is that we cannot adequately explain its existence by what we currently understand about the nose. Many otolaryngologists are unwilling to make a ‘leap of faith’ and, instead of acknowledging the existence of something they do not understand, are left skeptical of it in its entirety.”
Back in San Diego, a landmark paper explaining a means of implanting tissue to fill some of surgery-related nasal vacancy (co-authored by Dr. Watson and fellow otolaryngologist Dr. Angela Chang of Scripps Health San Diego) has no problem acknowledging the existence of empty-nose syndrome. The specialists describe the same pioneering procedure that Nathan Schmidt underwent twice as Watson’s patient.
“Empty nose syndrome (ENS) is a potential complication of excessive resection of turbinate tissue,” reads an abstract. “Patients with ENS complain of nasal obstruction despite a widely patent nasal cavity.”
The San Diego otolaryngologists’ work on a treatment notwithstanding, no mention of empty-nose syndrome is mentioned as a risk of turbinate-reduction surgery on a National Institutes of Health website called MedicinePlus. The governmental site, billed as a trusted source of pre-surgery medical information for patients as well as families and friends of patients, lists only the following risks associated with turbinectomies: “a hole in the tissue that divides the sides of the nose (septum), loss of feeling in the skin on the nose, change in the sense of smell, fluid buildup in the nose, and return of the nasal blockage after surgery.”
Scripps otolaryngologist Dr. Chang says physicians sometimes scratch their heads when empty-nose sufferers say they can’t breath.
“One patient described it as feeling like someone were suffocating him with a pillow,” Dr. Chang says. “But then doctors look into their nasal passages and see that air is definitely getting through. I think some patients feel that their doctors think they’re crazy.”
But Chang doesn’t think they’re crazy. She acknowledges that there is a difference between someone who actually thinks they’re not breathing when indeed they are, versus someone who understands that they are respirating, yet nevertheless feels as if they’re suffocating.
“Empty-nose is not widely understood,” she says, “It’s extremely rare, but for patients who have it, it’s a really, really hard condition for them to live with.”
She doesn’t know why there has not been much if any replication of the turbinate-implant procedure she helped pioneer, but she’s inclined to chalk it up to a dearth of sufferers.
“There just aren’t that many,” says Chang. “But a patient I did implant surgery on in 2008 still says his condition continues to be improved compared to how he felt before the procedure.”
As it happens, this year’s annual meeting of the American Academy of Otolaryngology–Head and Neck Surgery Foundation will convene at the San Diego Convention Center in September.
In light of recent news coverage about empty-nose syndrome and the fact that Drs. Watson’s and Chang’s research publication (titled “Inferior turbinate augmentation with auricular cartilage for the treatment of empty nose syndrome”) appeared late last year in the Ear, Nose and Throat Journal, you’d think the two San Diego doctors’ procedures will be a hot topic at the otolaryngology specialty’s annual pilgrimage. But none of the nearly 300 workshops, symposiums, mini-symposiums, and other classes on tap at the international conference refer to empty-nose syndrome in their titles. Neither Watson’s nor Chang’s name appears among the hundreds of speakers.
It’s not clear whether two workshops — under whose titles empty-nose syndrome could conceivably fall as a subtopic — will address the condition. Those include a session called, “Surgery of the Inferior, Middle, and Superior Turbinates” and another with a title that invokes a particularly vulnerable group of patients: “Controversies in the Evaluation and Treatment of Pediatric Sleep Apnea.”
Looking at the agenda at this year’s conference, one can see why empty-nose syndrome sufferers feel invisible to the profession that gave them the condition.
“ENS absolutely exists,” University of Virginia’s Dr. Payne said in an interview about the disorder. “It’s just not necessarily certain what that means for every specific patient.”
Payne adds that patients who suffer from empty-nose syndrome are a paradox because they say they can’t breathe yet clearly they can.
Both Nathan Schmidt and Robert Gerlach find that characterization offensive.

“‘No one with this condition says, ‘Hey, I can’t breathe,’” Gerlach points out. “We say, ‘It feels like I can’t breathe’ — all the fucking time. There’s a big difference. We’re not crazy. We understand that we’d be dead if air wasn’t going into our lungs.”
A few weeks after the ear, nose, and throat doctors’ convention leaves San Diego, another gathering will hit town. With roots firmly planted up north in Silicon Valley, the Exponential Medicine Expo kicks off at the Hotel Del Coronado in October. When it does, a handful of empty-nose sufferers and others interested in the condition will attend a workshop where the possibility of using 3D-printer technology to create material that could replace lost turbinate tissue will be discussed.
Gerlach has traveled to see otolaryngologists at Stanford, UCSD, UCLA, the Mayo Clinic, and numerous other institutions in search of relief. For reasons ranging from medical to financial, no one has been willing to take his case on.
Gerlach was also seen by UCSD’s Dr. Watson but was not offered the implant Schmidt got.
“She was a very nice lady, well-intentioned, but she was just like every other otolaryngology specialist who’s seen me since I was given the life-crushing gift that is empty-nose syndrome,” Gerlach says. “Ultimately she had nothing to offer me to help me feel like I can breathe correctly again.”


If you’ve ever had a bad toothache in your upper jaw, you know the general area where the human animal experiences life in its greatest intensity. You can’t get away from the pain because it’s right where you live. Similarly, sufferers of a medical condition called empty-nose syndrome, say they found out the hard way that the area inside of your nose and above the roof of your mouth can provide a baseline sense of well-being — or a complete lack thereof.
“It’s pure, unremitting hell,” says Robert Gerlach, 34, of Lemon Grove, who was diagnosed with empty-nose syndrome following a nasal surgery in 2011. Gerlach, who relocated to the San Diego area from Rochester, New York, two years ago, is like many others who move to the region hoping this is where they will find relief from the rare, but increasingly recognized condition.
It turns out, a common procedure called a turbinectomy or turbinate-reduction surgery in rare cases can cause empty-nose syndrome. Turbinate reductions are frequently performed to treat sleep apnea. That was the reason for Gerlach’s operation.
Just above the roof of your mouth and behind the exterior of your nose are a set of three tiers of flesh-covered bones. Each of those tiers is decked out with a pair of structures called nasal turbinates. These are bony, knoblike features inside the “nasal vault.” They are covered with soft tissue made up of epithelium and mucosa that exchange and humidify air, while also warming air to ready it for maximum oxygenation and distribution by the lungs.
The system of turbinates is a stroke of evolutionary genius, which the American Rhinologic Society says has been key to mammals’ and birds’ ability to adapt to hostile climates. The epithelium, which look like microscopic hairs on the turbinates, allow you to smell and to efficiently breathe through your nose.
Ear, nose, and throat specialists often surgically reduce the size of nasal turbinates on people with chronic breathing problems. Although most turbinate reductions are successful, empty-nose is a rare post-surgery syndrome that leaves its victims feeling permanently “hollowed out” or “zombie-like,” as more than one sufferer described their symptoms to the San Diego Reader.
“This is worse than death,” says Gerlach, who has undergone nearly a dozen subsequent procedures in search of relief following the turbinate operation he says gave him empty-nose syndrome.
Gerlach’s first surgery did nothing to alleviate his obstructive sleep apnea. He says his sleep troubles are worse than ever. Sleep clinics across San Diego, where he frequently undergoes studies, have become his homes away from home.
Put in lay terms, obstructive sleep apnea happens when tissue blocks the respiratory system, encumbering normal sleep. Nasal turbinates are often blamed for such obstructions; so it’s only natural that doctors have, for years, been surgically reducing turbinate tissue.
Most researchers cite a 1993 study published in the New England Journal of Medicine that found 24 percent of men and 9 percent of women in America suffer from obstructive sleep apnea. It’s a condition that can lead to depression, stroke, heart disease — even death. However, there’s little agreement about the success rate of turbinate reduction as a treatment for sleep apnea. Figures range from a 30–90 percent success rate, varying by technique.
Another local empty-nose patient says the fact that he was told he needed nasal surgery to help him breathe better couldn’t have come from further out of left field than it did.
“I didn’t even have a problem breathing or sleeping or anything — not even a deviated septum,” says Nathan Schmidt, 36. He underwent “an overly aggressive” turbinate reduction in 2004 in Boston. “I was young, in a band and thought I’d listen to my friends’ and family’s warnings that loud music was bad for my hearing,” Schmidt says, recalling his decision to get checked out by an ear, nose, and throat specialist as a precautionary measure to protect his hearing.

“I thought I was being proactive,” he says, adding that he now wishes that instead of an ear, nose, and throat doctor he would have seen an audiologist, who would have just tested his hearing.
“Instead, he looked in my nose and said I’d breathe a lot better if I had turbinate-reduction surgery. I told him I didn’t think I had any trouble breathing, to which he replied, ‘You don’t know what normal breathing is because you don’t have any other point of reference.’”
His insurance paid for the turbinectomy to the tune of about $12,000. Starting with losing the ability to play in a band, Schmidt’s life would never be the same. He now lives in Tijuana, where he owns a small business.
He receives care for empty-nose syndrome in San Diego from Deborah Watson, M.D. Watson is an otolaryngology (ear, nose, and throat) surgeon and professor of surgery at UCSD. She is considered one of the nation’s foremost experts on empty-nose syndrome. He praises Watson for diagnosing his post-surgery travails as empty-nose syndrome and for helping him find modest relief.
How many people suffer from empty-nose syndrome? No one knows because there’s never been an effort to find out.
“It’s not in their interest to bring this up,” says Gerlach, referring to the otolaryngology profession. “Turbinate reductions are the most common surgery they do; they don’t even tell you it can cause empty-nose.”
Compared to Gerlach’s, Schmidt’s condition is mild. In fact, Schmidt says his is among the mildest he’s heard of among a growing community of sufferers who seek solutions, advice, and share news of potential new treatments with one another via social media. Yet, even for Schmidt, having empty-nose is a rough way to live.
“It’s tough, but some days are better than others,” Schmidt says. “I’m a naturally outgoing, well-adjusted person. I went to Juilliard and had a very active social life before empty-nose syndrome. But when my nose is bad, which is well over half the time, I feel miserable, tired, and anxious, and don’t want to go out. It’s difficult making plans; like if I’m invited to something, I’ll instantly think, If my nose is bad that day, I’ll not want to go, and if I do go and look miserable people will think it’s because I don’t like them. Having said that, I try to see it as just a disability and keep in mind all the other aspects of myself, like my intellect and health otherwise, that it doesn’t affect.”
Serious respiratory issues are part of what defines empty-nose. But Schmidt is the recipient of a highly prized rarity among sufferers: a medical procedure that restored a modicum of feeling like he “can breathe right.”
“I had two separate cartilage implants performed by Deborah Watson at UCSD Medical Center,” he says. “They were both beneficial, but by no means a cure. I had the first implant about 11 years ago.”
But many sufferers believe there is an effort by the ear, nose, and throat medical establishment to stifle awareness of their condition. They say turbinate-reduction surgeries are quick, easy ways to generate revenue with little risk. One sufferer says there’s a “turbinectomy industrial complex.”
“Most people come out of turbinate-reduction surgery fine,” says Gerlach. “The problem is you aren’t told what the risk is.”
Ear, nose, and throat doctors deny being cavalier about turbinate reductions or that there is a tacit conspiracy to ratchet up revenue by overprescribing the procedures.
Meanwhile, Gerlach’s sojourn for relief from symptoms that range from a constant feeling of suffocation and exhaustion to anxiety and memory loss has taken him from coast to coast and back again. He says even sympathetic ear, nose, and throat doctors are loath to talk about empty-nose syndrome.
“I’d be very surprised if you could get any of these doctors to talk to you about empty-nose syndrome in the media,” Gerlach says.
Indeed, physicians in the local otolaryngology community contacted by the San Diego Reader were mostly unwilling to discuss empty-nose syndrome.
As well as being home to a top-notch, albeit sometimes media-shy, medical community with expertise on empty-nose syndrome, there’s another reason sufferers settle in San Diego.
“The salt in the air is better for my nose, and the climate is more consistent, which makes it somewhat easier to breathe than artificially heated air,” Gerlach says, adding that he had hoped San Diego’s vibrant biotech and stem-cell industries might offer a new solution.
He dreams that one day he’ll wake up to a headline announcing that one of San Diego’s famous life science companies has developed a therapy to regenerate nasal tissue. Until then, there’s our mild climate.
“I feel worse in hot and humid weather,” says Nathan Schmidt. “I always sleep with an air conditioner. Cool, dry air helps stimulate mucous production. San Diego and Tijuana weather for me isn’t so bad. I used to live in Boston, where the summers were intolerable.”
Schmidt and Gerlach feel there’s a crucial difference between sufficient respiration, which they and most empty-nose sufferers technically have, versus the satisfaction and sense of well-being that comes with the sensation of breathing normally.
“I would put the nonrespiratory symptoms of empty-nose syndrome into two categories,” Schmidt explains. “The first is missing everyday sensations of the nose. Most people take it for granted, but nasal sensitivity is a consistent source of pleasure. Even though it’s associated with being sick and congested, when you sneeze you get a shot of pleasure, or like when you breathe deeply through the nose or meditate, it’s relaxing.”
Schmidt says he never knew how key to being happy the feeling of having a functioning nose was until it was gone. He thinks he’d do almost anything to feel “nice, normal nasal congestion again.”
Asked to describe the sensation of the syndrome, Schmidt askes me to imagine “the panic that sets in when you hold your breath for too long, like trying to come up for air in the water, but you’ve way underestimated how deep in the pool you are.”
He continues, “I’m convinced that part of the patient’s brain literally thinks that he is not breathing, due to the nose not sensing airflow even if air is going in,” he continues. “[Your] nose goes from being a source of pleasure to a source of anxiety. For a lot of patients, including myself before my first corrective surgery was done by Dr. Watson, it’s so unbearable that they resort to plugging their noses, wishing they didn’t have a nose at all.”
Noting that empty-nose patients have committed suicide because of the condition, a recent Buzzfeed article with the headline, “Is Empty Nose Syndrome Real, and if not, Why are People Killing Themselves Over It?” cited an academic paper by Dr. Spencer Payne of the University of Virginia. “The problem with empty-nose syndrome is probably not that it does not exist,” Dr. Spencer says. “It is that we cannot adequately explain its existence by what we currently understand about the nose. Many otolaryngologists are unwilling to make a ‘leap of faith’ and, instead of acknowledging the existence of something they do not understand, are left skeptical of it in its entirety.”
Back in San Diego, a landmark paper explaining a means of implanting tissue to fill some of surgery-related nasal vacancy (co-authored by Dr. Watson and fellow otolaryngologist Dr. Angela Chang of Scripps Health San Diego) has no problem acknowledging the existence of empty-nose syndrome. The specialists describe the same pioneering procedure that Nathan Schmidt underwent twice as Watson’s patient.
“Empty nose syndrome (ENS) is a potential complication of excessive resection of turbinate tissue,” reads an abstract. “Patients with ENS complain of nasal obstruction despite a widely patent nasal cavity.”
The San Diego otolaryngologists’ work on a treatment notwithstanding, no mention of empty-nose syndrome is mentioned as a risk of turbinate-reduction surgery on a National Institutes of Health website called MedicinePlus. The governmental site, billed as a trusted source of pre-surgery medical information for patients as well as families and friends of patients, lists only the following risks associated with turbinectomies: “a hole in the tissue that divides the sides of the nose (septum), loss of feeling in the skin on the nose, change in the sense of smell, fluid buildup in the nose, and return of the nasal blockage after surgery.”
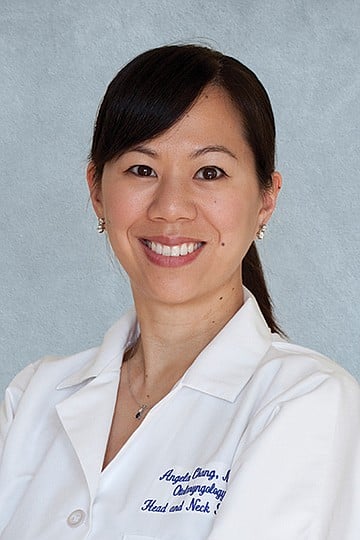
Scripps otolaryngologist Dr. Chang says physicians sometimes scratch their heads when empty-nose sufferers say they can’t breath.
“One patient described it as feeling like someone were suffocating him with a pillow,” Dr. Chang says. “But then doctors look into their nasal passages and see that air is definitely getting through. I think some patients feel that their doctors think they’re crazy.”
But Chang doesn’t think they’re crazy. She acknowledges that there is a difference between someone who actually thinks they’re not breathing when indeed they are, versus someone who understands that they are respirating, yet nevertheless feels as if they’re suffocating.
“Empty-nose is not widely understood,” she says, “It’s extremely rare, but for patients who have it, it’s a really, really hard condition for them to live with.”
She doesn’t know why there has not been much if any replication of the turbinate-implant procedure she helped pioneer, but she’s inclined to chalk it up to a dearth of sufferers.
“There just aren’t that many,” says Chang. “But a patient I did implant surgery on in 2008 still says his condition continues to be improved compared to how he felt before the procedure.”
As it happens, this year’s annual meeting of the American Academy of Otolaryngology–Head and Neck Surgery Foundation will convene at the San Diego Convention Center in September.
In light of recent news coverage about empty-nose syndrome and the fact that Drs. Watson’s and Chang’s research publication (titled “Inferior turbinate augmentation with auricular cartilage for the treatment of empty nose syndrome”) appeared late last year in the Ear, Nose and Throat Journal, you’d think the two San Diego doctors’ procedures will be a hot topic at the otolaryngology specialty’s annual pilgrimage. But none of the nearly 300 workshops, symposiums, mini-symposiums, and other classes on tap at the international conference refer to empty-nose syndrome in their titles. Neither Watson’s nor Chang’s name appears among the hundreds of speakers.
It’s not clear whether two workshops — under whose titles empty-nose syndrome could conceivably fall as a subtopic — will address the condition. Those include a session called, “Surgery of the Inferior, Middle, and Superior Turbinates” and another with a title that invokes a particularly vulnerable group of patients: “Controversies in the Evaluation and Treatment of Pediatric Sleep Apnea.”
Looking at the agenda at this year’s conference, one can see why empty-nose syndrome sufferers feel invisible to the profession that gave them the condition.
“ENS absolutely exists,” University of Virginia’s Dr. Payne said in an interview about the disorder. “It’s just not necessarily certain what that means for every specific patient.”
Payne adds that patients who suffer from empty-nose syndrome are a paradox because they say they can’t breathe yet clearly they can.
Both Nathan Schmidt and Robert Gerlach find that characterization offensive.

“‘No one with this condition says, ‘Hey, I can’t breathe,’” Gerlach points out. “We say, ‘It feels like I can’t breathe’ — all the fucking time. There’s a big difference. We’re not crazy. We understand that we’d be dead if air wasn’t going into our lungs.”
A few weeks after the ear, nose, and throat doctors’ convention leaves San Diego, another gathering will hit town. With roots firmly planted up north in Silicon Valley, the Exponential Medicine Expo kicks off at the Hotel Del Coronado in October. When it does, a handful of empty-nose sufferers and others interested in the condition will attend a workshop where the possibility of using 3D-printer technology to create material that could replace lost turbinate tissue will be discussed.
Gerlach has traveled to see otolaryngologists at Stanford, UCSD, UCLA, the Mayo Clinic, and numerous other institutions in search of relief. For reasons ranging from medical to financial, no one has been willing to take his case on.
Gerlach was also seen by UCSD’s Dr. Watson but was not offered the implant Schmidt got.
“She was a very nice lady, well-intentioned, but she was just like every other otolaryngology specialist who’s seen me since I was given the life-crushing gift that is empty-nose syndrome,” Gerlach says. “Ultimately she had nothing to offer me to help me feel like I can breathe correctly again.”
Comments