 Facebook
Facebook
 X
X
 Instagram
Instagram
 TikTok
TikTok
 Youtube
Youtube
OUR INDEPENDENT PROVIDER ASSOCIATION (IPA) MEETING THURSDAY NIGHT ADDRESSED NEARLY EVERY NIGHTMARISH ASPECT OF PRACTICING MEDICINE IN THE 1990S. MEETINGS SUCH AS THIS ARE RUINING MY HEALTH.
Three months ago, our IPA announced it had tumbled into deep financial trouble, with about $3 million of debts, minimal cash reserves, and a negative monthly balance sheet. The IPA — which I’ll call Quality Services Medical Group (QSMG) to protect its corporate secrets — pays me for the health care of about 20 percent of my patients, so I would like to see it do well. The medical group called this meeting to tell all of us shareholders what it was doing to manage the crisis.
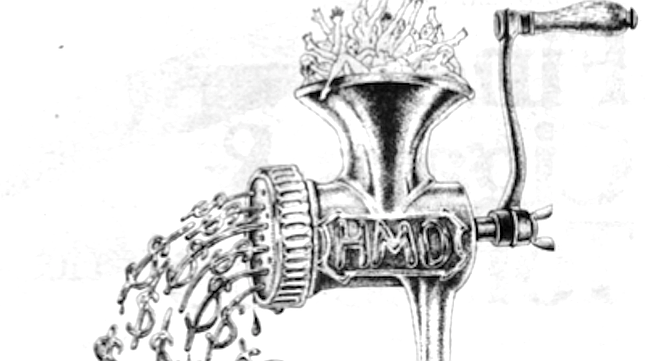
IPAs are like stockbrokers; in an ideal world, they wouldn't exist. In the big picture, they have no purpose; they are middlemen. Aetna, Blue Cross, Foundation Health, Health Net, and other insurance companies design health insurance plans and sell them to employers, who then sign up their employees. But the insurance companies don’t have any doctors, hospitals, labs, x-ray facilities, or other personnel and equipment to provide health care to their enrollees in HMO (Health Maintenance Organization) plans. IPAs are regional collections of health care providers, which exist so that HMOs can contract with them for these services in a given geographical area. Kaiser is the exception; they have their own providers who work only for Kaiser and therefore see only Kaiser patients. Kaiser doesn’t use IPAs, which helps them control costs. We can hope that our IPA will someday be able to contract directly with employers and replace the greedy HMOs that are draining all the resources out of medicine and into their huge bank accounts.
Meanwhile, QSMG is in trouble. Two corporate financial consultants stood before us and told us why we got into trouble and how we were going to get out. They told us that the medical group had overpaid its doctors, sacrificing its long-term financial viability to keep us happy. To correct this, they cut payments to primary care physicians by 20 percent beginning July 1.
That move had repercussions. Primary care physicians (family physicians, internists, and pediatricians) have much higher overhead costs than specialists, usually about 60 percent of our gross receipts, which leaves the other 40 percent as our profit margin. When the group cut our payments by 20 percent, they halved our earnings. For those among us who had as many as 80 percent of our patients belonging to QSMG , this was devastating. One of my favorite colleagues abandoned her solo practice to join Kaiser. Several others now have practices on the edge of financial insolvency.
Specialists have not fared well either. QSMG has cut their payments 45 percent over the past several years. Fortunately for the specialists, this came on the heels of a decade of unprecedented prosperity, where they were raking in fortunes that one could easily label excessive — $250,0(X) to $1 million annually. Even as the market corrects itself, those specialists who have managed their money well are not hurting the way the primary care doctors are.
Let’s assume you are a teacher and you live in my area. The school district gives you a choice among different health plans, including Kaiser. Suppose you select a Health Net HMO plan. In our region, the HMOs contract with two competing IPAs, QSMG and BPMG (Best Physicians Medical Group, not their real name). You choose the group you want to use, often based on which hospital the IPA uses or which physicians belong to the group. I am unusual in that I belong to both groups. QSMG hates the fact that I am not exclusive to their group because it allows patients to select BPMG and still see me, so QSMG cannot use me as a means to attract patients away from the competition. BPMG tolerates my infidelity because they are based in the next town, not mine. My presence gives them access to more patients through greater geographical coverage. I’m not willing to drop BPMG because if I did, the 20 percent of my patients who are in BPMG would have to switch to QSMG or see another doctor. QSMG’s current financial straits illustrate how stupid I would be to become exclusive to their group.
You then decide on a primary care physician, and since I am inventing this scenario, you will pick me. Because you live in my town, you pick the local IPA, QSMG, so that if you ever end up in the hospital, you will go to First Quality Hospital. Your school district begins paying monthly premiums to Health Net.
Health Net pockets 15 to 20 percent of your premium to pay its CEO and administrators for the great job they do designing and selling their health plans; it gives the rest to QSMG to cover all of your health care costs for the month. Whether you never see the doctor or you need S15,000 worth of care for a hernia operation this month, Health Net pays the same amount to QSMG.
This is a great arrangement for insurance companies. They leave it to the IPA to administer the benefits of their plans, so when a subscriber wants a service that is not covered, cannot see an out-of-plan specialist, or cannot have a medicine he wants because it’s too expensive, he finds out from his primary care physician or from the I PA. So who’s on the front lines getting the complaints? The primary care physicians and the IPA. The insurance companies just sit back and count their profits. How much profit? The CEOs of the top ten insurance companies in 1995 split $7 billion.
That’s right: ten guys, $7 billion in one year.
I could gross $700 million if I examined ten million women or delivered 500,000 babies in a year; I guess CEOs think their great logos and TV ads are worth netting that much. So they tell us that the reason our IPA is insolvent is because it pays doctors too much. Draw your own conclusions. The insurance companies control the money because consumers’ employers pay them, and as long as they have the money, they can make the rules.
Some of the more ridiculous rules they make involve medications. Suppose you suffer from hay fever, including watery eyes, sneezing, runny nose, and scratchy throat. Benadryl clears you up, but your snoring through office meetings is taxing your boss’s patience.
I prescribe a medicine for your nose that works great, but you’re tired of showing up for dates looking like you just read Anna Karenina, so we decide to prescribe you a nonsedating antihistamine. If you watch TV, you have seen the ads for these, with children and parents in hot air balloons soaring over golden meadows, their hearts filled with glee and their air passages free from mucus.
We have a choice between Allegra, Claritin, Hismanal, and Zyrtec (I want to meet the marketing wizard who came up with that name). When deciding between nearly identical drugs, the patient and I opt for the cheapest and/or the one with the most convenient dosing schedule. But the choice is not ours to make anymore. Each insurance company has its own formulary, and we doctors must prescribe drugs on the formulary, or the insurance company won’t pay for it. Why? Because insurance and pharmaceutical companies make deals. So if Health Net made a deal with Schering this month, I have to know this and prescribe Claritin, even though Allegra is usually less expensive. If Schering and Health Net have a spat, and next month Janssen gets the deal, I have to switch the patient to Hismanal.
Then there is the whole issue of generic drugs. When a new medicine becomes available, the pharmaceutical company that patented it gets exclusive rights to sell it until its patent expires, at which time other companies can make the same medicine and sell it cheaper as a generic. Now, when a given drug’s patent expires, the company with the patent almost always makes a generic version that is identical to its brand-name product except it does not display the original logo on the pills or the label. So most generic drugs are exactly the same as the original, and they sell for less.
IPAs, in their efforts to control costs, are trying to get their physicians to prescribe generic medications. The pharmaceutical industry, to protect its huge profit margins, is trying to maximize the use of brand-name medications.
You go to the pharmacy with a prescription that specifies “Presslow pills” (not an actual drug name) for high blood pressure. Your pharmacist reads the prescription, knowing that Ruxarus Pharmaceuticals (fictitious name) makes a generic version of this drug that costs 40 percent less than the brand name. He also knows that Buxarus will give him a $20 rebate every time he dispenses the brand-name version, so he searches the prescription for the words “Dispense generic unless otherwise specified.” He doesn’t find them, because we have yet to educate most doctors to include those words on our preprinted prescription pads. Pharmacists, especially those running small private businesses, are caught in the vise of dwindling reimbursements and shrinking profits as much as the rest of us health care service providers, so he dispenses the brand-name product and pockets the $20, knowing he has helped increase the cost of health insurance in order to pay his rent.
Insurance companies can’t resist such temptation either. Most HMOs in California’s major cities are in the process of shifting or have already shifted the financial risk for their clients’ pharmacy costs to the IPAs by paying the IPAs a fixed, small amount of money per month for each patient to cover pharmacy costs. Having unloaded this responsibility, many HMOs have landed contracts with pharmaceutical companies that give them a rebate when the pharmacist dispenses the brand-name medication. Now the HMOs can encourage their patients to demand brand-name products; the rebates increase the HMOs’ profits, and the IPA pays for the more expensive medications.
Because of this, QSMG announced at the meeting that it is issuing us preprinted pads that include the phrase “Dispense generic unless otherwise specified." They also told us that the group will include pharmacy costs per patient in our quarterly “report cards,” which inform each primary care physician how much the care of his patients is costing the IPA. If we are “efficient” and spend less than a certain target amount in providing care, including the costs specialists incur while caring for our patients, the group will reward us. That is what the group tells us. The reality is that they will dock us less when the next round of reimbursement cuts comes, as they have never had money to give us bonuses in the past, and I do not see any reason to believe they will have any in the future. Those PCPs (primary-care physicians) who are above the targets will not get the “bonus” of a smaller pay cut.
If you have noticed that your doctor seems to have less time for you, to look more stressed than before, and to have less competent staff at the office, you are probably right. It will get worse before it gets better.
One might wonder why the IPAs cannot negotiate better contracts with the HMOs to get more money. The answer to an economist is simple: there are too many doctors and too many IPAs.
In our region, we have the two IPAs: QSMG and BPMG. When the HMOs come around every year to renew the contracts, the negotiations go something like the following.
The HMO’s CEO gives QSMG’s president an envelope with an offer, always for less money per patient than the previous year. With the envelope comes a clear message: “If you don’t accept this offer, we’ll take all of your patients down the road to BPMG." The CEO does the same thing when he meets with BPMG. The existence of the two IPAs allows the HMO to ratchet down its offer every year until one of the medical groups goes out of business. Both of our groups have powerhouse financial institutions backing them as capital partners. Both are running lean; BPMG has been particularly aggressive in cutting excess specialists and other surplus providers out of its plan to keep costs down. QSMG has been more loyal to its specialists, and that is the biggest reason its financial troubles are much worse.
The other major player in our region is Kaiser. Kaiser is now making a big push to drive down its premiums so low that the rest of us will go out of business, and they may succeed. The model that Kaiser and the other HMOs are moving toward to keep costs down is to restrict access to providers as much as possible. Each PCP in the plan will be responsible for about 4000 patients, twice as many as now. When a patient wants to talk to his PCP, he will use either his phone or computer to access a triage system that will take him through a series of decision trees and either recommend a treatment or allow him access to a health care provider.
That initial provider probably will not be your primary care provider (physician, nurse practitioner, or physician’s assistant), but someone with less training who works for less money. If your problem is too complex for that person, then maybe you will get to see or talk to your PCP. This system will also make much more use of mid-level practitioners (nurse practitioners and physician’s assistants) because they will work for less money than physicians. Physicians will see only those people with complex medical problems and will not get the opportunity to know their patients in times of good health, when we can emphasize the processes of building trust and preventing disease. We will supervise the care of scores of others whom we may never meet.
Systems such as these work for two types of people; those who almost never have to use it and those who are intelligent and assertive enough to work through it. A disproportionate number of people who will read this article fall into one or both categories, but for most people, this type of system will not maintain health, which will render the term Health Maintenance Organization ironic. Fond as I am of examples of true irony, I do not want my profession to be one of them.

OUR INDEPENDENT PROVIDER ASSOCIATION (IPA) MEETING THURSDAY NIGHT ADDRESSED NEARLY EVERY NIGHTMARISH ASPECT OF PRACTICING MEDICINE IN THE 1990S. MEETINGS SUCH AS THIS ARE RUINING MY HEALTH.
Three months ago, our IPA announced it had tumbled into deep financial trouble, with about $3 million of debts, minimal cash reserves, and a negative monthly balance sheet. The IPA — which I’ll call Quality Services Medical Group (QSMG) to protect its corporate secrets — pays me for the health care of about 20 percent of my patients, so I would like to see it do well. The medical group called this meeting to tell all of us shareholders what it was doing to manage the crisis.
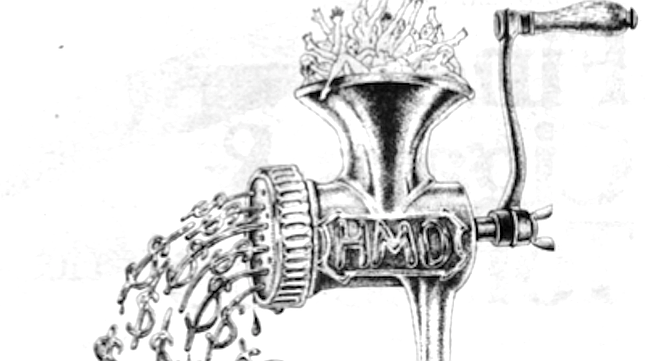
IPAs are like stockbrokers; in an ideal world, they wouldn't exist. In the big picture, they have no purpose; they are middlemen. Aetna, Blue Cross, Foundation Health, Health Net, and other insurance companies design health insurance plans and sell them to employers, who then sign up their employees. But the insurance companies don’t have any doctors, hospitals, labs, x-ray facilities, or other personnel and equipment to provide health care to their enrollees in HMO (Health Maintenance Organization) plans. IPAs are regional collections of health care providers, which exist so that HMOs can contract with them for these services in a given geographical area. Kaiser is the exception; they have their own providers who work only for Kaiser and therefore see only Kaiser patients. Kaiser doesn’t use IPAs, which helps them control costs. We can hope that our IPA will someday be able to contract directly with employers and replace the greedy HMOs that are draining all the resources out of medicine and into their huge bank accounts.
Meanwhile, QSMG is in trouble. Two corporate financial consultants stood before us and told us why we got into trouble and how we were going to get out. They told us that the medical group had overpaid its doctors, sacrificing its long-term financial viability to keep us happy. To correct this, they cut payments to primary care physicians by 20 percent beginning July 1.
That move had repercussions. Primary care physicians (family physicians, internists, and pediatricians) have much higher overhead costs than specialists, usually about 60 percent of our gross receipts, which leaves the other 40 percent as our profit margin. When the group cut our payments by 20 percent, they halved our earnings. For those among us who had as many as 80 percent of our patients belonging to QSMG , this was devastating. One of my favorite colleagues abandoned her solo practice to join Kaiser. Several others now have practices on the edge of financial insolvency.
Specialists have not fared well either. QSMG has cut their payments 45 percent over the past several years. Fortunately for the specialists, this came on the heels of a decade of unprecedented prosperity, where they were raking in fortunes that one could easily label excessive — $250,0(X) to $1 million annually. Even as the market corrects itself, those specialists who have managed their money well are not hurting the way the primary care doctors are.
Let’s assume you are a teacher and you live in my area. The school district gives you a choice among different health plans, including Kaiser. Suppose you select a Health Net HMO plan. In our region, the HMOs contract with two competing IPAs, QSMG and BPMG (Best Physicians Medical Group, not their real name). You choose the group you want to use, often based on which hospital the IPA uses or which physicians belong to the group. I am unusual in that I belong to both groups. QSMG hates the fact that I am not exclusive to their group because it allows patients to select BPMG and still see me, so QSMG cannot use me as a means to attract patients away from the competition. BPMG tolerates my infidelity because they are based in the next town, not mine. My presence gives them access to more patients through greater geographical coverage. I’m not willing to drop BPMG because if I did, the 20 percent of my patients who are in BPMG would have to switch to QSMG or see another doctor. QSMG’s current financial straits illustrate how stupid I would be to become exclusive to their group.
You then decide on a primary care physician, and since I am inventing this scenario, you will pick me. Because you live in my town, you pick the local IPA, QSMG, so that if you ever end up in the hospital, you will go to First Quality Hospital. Your school district begins paying monthly premiums to Health Net.
Health Net pockets 15 to 20 percent of your premium to pay its CEO and administrators for the great job they do designing and selling their health plans; it gives the rest to QSMG to cover all of your health care costs for the month. Whether you never see the doctor or you need S15,000 worth of care for a hernia operation this month, Health Net pays the same amount to QSMG.
This is a great arrangement for insurance companies. They leave it to the IPA to administer the benefits of their plans, so when a subscriber wants a service that is not covered, cannot see an out-of-plan specialist, or cannot have a medicine he wants because it’s too expensive, he finds out from his primary care physician or from the I PA. So who’s on the front lines getting the complaints? The primary care physicians and the IPA. The insurance companies just sit back and count their profits. How much profit? The CEOs of the top ten insurance companies in 1995 split $7 billion.
That’s right: ten guys, $7 billion in one year.
I could gross $700 million if I examined ten million women or delivered 500,000 babies in a year; I guess CEOs think their great logos and TV ads are worth netting that much. So they tell us that the reason our IPA is insolvent is because it pays doctors too much. Draw your own conclusions. The insurance companies control the money because consumers’ employers pay them, and as long as they have the money, they can make the rules.
Some of the more ridiculous rules they make involve medications. Suppose you suffer from hay fever, including watery eyes, sneezing, runny nose, and scratchy throat. Benadryl clears you up, but your snoring through office meetings is taxing your boss’s patience.
I prescribe a medicine for your nose that works great, but you’re tired of showing up for dates looking like you just read Anna Karenina, so we decide to prescribe you a nonsedating antihistamine. If you watch TV, you have seen the ads for these, with children and parents in hot air balloons soaring over golden meadows, their hearts filled with glee and their air passages free from mucus.
We have a choice between Allegra, Claritin, Hismanal, and Zyrtec (I want to meet the marketing wizard who came up with that name). When deciding between nearly identical drugs, the patient and I opt for the cheapest and/or the one with the most convenient dosing schedule. But the choice is not ours to make anymore. Each insurance company has its own formulary, and we doctors must prescribe drugs on the formulary, or the insurance company won’t pay for it. Why? Because insurance and pharmaceutical companies make deals. So if Health Net made a deal with Schering this month, I have to know this and prescribe Claritin, even though Allegra is usually less expensive. If Schering and Health Net have a spat, and next month Janssen gets the deal, I have to switch the patient to Hismanal.
Then there is the whole issue of generic drugs. When a new medicine becomes available, the pharmaceutical company that patented it gets exclusive rights to sell it until its patent expires, at which time other companies can make the same medicine and sell it cheaper as a generic. Now, when a given drug’s patent expires, the company with the patent almost always makes a generic version that is identical to its brand-name product except it does not display the original logo on the pills or the label. So most generic drugs are exactly the same as the original, and they sell for less.
IPAs, in their efforts to control costs, are trying to get their physicians to prescribe generic medications. The pharmaceutical industry, to protect its huge profit margins, is trying to maximize the use of brand-name medications.
You go to the pharmacy with a prescription that specifies “Presslow pills” (not an actual drug name) for high blood pressure. Your pharmacist reads the prescription, knowing that Ruxarus Pharmaceuticals (fictitious name) makes a generic version of this drug that costs 40 percent less than the brand name. He also knows that Buxarus will give him a $20 rebate every time he dispenses the brand-name version, so he searches the prescription for the words “Dispense generic unless otherwise specified.” He doesn’t find them, because we have yet to educate most doctors to include those words on our preprinted prescription pads. Pharmacists, especially those running small private businesses, are caught in the vise of dwindling reimbursements and shrinking profits as much as the rest of us health care service providers, so he dispenses the brand-name product and pockets the $20, knowing he has helped increase the cost of health insurance in order to pay his rent.
Insurance companies can’t resist such temptation either. Most HMOs in California’s major cities are in the process of shifting or have already shifted the financial risk for their clients’ pharmacy costs to the IPAs by paying the IPAs a fixed, small amount of money per month for each patient to cover pharmacy costs. Having unloaded this responsibility, many HMOs have landed contracts with pharmaceutical companies that give them a rebate when the pharmacist dispenses the brand-name medication. Now the HMOs can encourage their patients to demand brand-name products; the rebates increase the HMOs’ profits, and the IPA pays for the more expensive medications.
Because of this, QSMG announced at the meeting that it is issuing us preprinted pads that include the phrase “Dispense generic unless otherwise specified." They also told us that the group will include pharmacy costs per patient in our quarterly “report cards,” which inform each primary care physician how much the care of his patients is costing the IPA. If we are “efficient” and spend less than a certain target amount in providing care, including the costs specialists incur while caring for our patients, the group will reward us. That is what the group tells us. The reality is that they will dock us less when the next round of reimbursement cuts comes, as they have never had money to give us bonuses in the past, and I do not see any reason to believe they will have any in the future. Those PCPs (primary-care physicians) who are above the targets will not get the “bonus” of a smaller pay cut.
If you have noticed that your doctor seems to have less time for you, to look more stressed than before, and to have less competent staff at the office, you are probably right. It will get worse before it gets better.
One might wonder why the IPAs cannot negotiate better contracts with the HMOs to get more money. The answer to an economist is simple: there are too many doctors and too many IPAs.
In our region, we have the two IPAs: QSMG and BPMG. When the HMOs come around every year to renew the contracts, the negotiations go something like the following.
The HMO’s CEO gives QSMG’s president an envelope with an offer, always for less money per patient than the previous year. With the envelope comes a clear message: “If you don’t accept this offer, we’ll take all of your patients down the road to BPMG." The CEO does the same thing when he meets with BPMG. The existence of the two IPAs allows the HMO to ratchet down its offer every year until one of the medical groups goes out of business. Both of our groups have powerhouse financial institutions backing them as capital partners. Both are running lean; BPMG has been particularly aggressive in cutting excess specialists and other surplus providers out of its plan to keep costs down. QSMG has been more loyal to its specialists, and that is the biggest reason its financial troubles are much worse.
The other major player in our region is Kaiser. Kaiser is now making a big push to drive down its premiums so low that the rest of us will go out of business, and they may succeed. The model that Kaiser and the other HMOs are moving toward to keep costs down is to restrict access to providers as much as possible. Each PCP in the plan will be responsible for about 4000 patients, twice as many as now. When a patient wants to talk to his PCP, he will use either his phone or computer to access a triage system that will take him through a series of decision trees and either recommend a treatment or allow him access to a health care provider.
That initial provider probably will not be your primary care provider (physician, nurse practitioner, or physician’s assistant), but someone with less training who works for less money. If your problem is too complex for that person, then maybe you will get to see or talk to your PCP. This system will also make much more use of mid-level practitioners (nurse practitioners and physician’s assistants) because they will work for less money than physicians. Physicians will see only those people with complex medical problems and will not get the opportunity to know their patients in times of good health, when we can emphasize the processes of building trust and preventing disease. We will supervise the care of scores of others whom we may never meet.
Systems such as these work for two types of people; those who almost never have to use it and those who are intelligent and assertive enough to work through it. A disproportionate number of people who will read this article fall into one or both categories, but for most people, this type of system will not maintain health, which will render the term Health Maintenance Organization ironic. Fond as I am of examples of true irony, I do not want my profession to be one of them.
Comments