 Facebook
Facebook
 X
X
 Instagram
Instagram
 TikTok
TikTok
 Youtube
Youtube
When someone dies in the state of California, we know, or can find out, what would seem to be everything we might want to know about the event: the place, date, and time of death; whether death took place in a convalescent hospital, at home, or other and if in a hospital, whether in ER, OP, or DOA; the names of a whole fleet of relations; whether it was from natural causes or by accident, suicide, homicide, pending investigation, or could not be determined; what the immediate cause of death was, and what cause that was due to, and what that was due to, and even what that was due to (along with any other significant conditions or operations); how long each of these contributory conditions kicked in before the patient kicked off; whether a biopsy or autopsy was performed; when the decedent was last attended by a doctor and last seen alive; the name (and license number) of the funeral director, the signature (and license number) of the embalmer, and the place of— ahem — final disposition.

But nobody knows the really important data on how we die. How many of us die painfully? Nobly? Tormented by regrets? With a sigh of relief? Peacefully? Angrily? Alone, lonely, and abandoned? Alone, thank God, at last? Surrounded by our relatives who have gathered to respect our life and our passage onwards? Surrounded by relatives who have gathered to squabble over our will?
To have some influence over how we die might seem to be one of life’s greatest ambitions, yet there is absolutely no reliable information on how people die or how they achieve a consummation devoutly to be wished, or to be feared. This unclear outcome is the linchpin of our fictions—the good dying peacefully or tragically, the bad falling from a great height onto sharp objects, the death perfectly or ironically illustrating the quality and virtue of the life—yet in real life we give no serious attention at all to how we ourselves want to die and how best to achieve that goal.
It’s a puzzle. We must be at least somewhat curious about it, given that a third of a million of us have bought Sherwin Nuland’s book How We Die, but all Nuland tells us is that we mostly die of disease processes that ultimately deprive some crucial muscle of oxygen. Yet most of us, in fact, spend most of our lives avoiding even thinking about death or what we want to make of it.

Which is more than a pity for two reasons. First, avoiding thinking about death tends to lead to exactly the death we fear; and second, there is an organization in San Diego whose sole purpose is to try to help us achieve (within limits) the kind of death we would like. Its name is — “Oh, for Pete’s sake,” you break in, “not another morbid article about death, surely?” Well, all right. In due course I’ll take you up on the notion that considering death must be morbid, but for the time being I’ll stick to safer ground and begin by looking at a weird and radical change that took place in medicine 50 years ago.
A BRIEF HISTORY Of DEATH
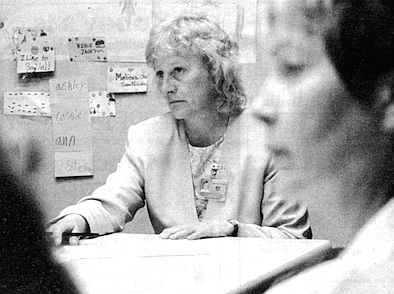
“If you look at American medical literature through the 1800s and 1900s,” said Dr. Laurel Herbst, medical director of San Diego Hospice, “death is accepted as inevitable. It’s the normal process, the classic lithograph of the physician at the child’s bedside— which, by the way, hangs in my living room. That was the norm."
The role of the doctor, in other words, was more compassionate, less technical. Sir William Osier, the great turn-of-the-century clinician, said that a physician needed three qualities: availability, affability, and ability, in that order. The doctor’s most valuable quality was his humanity in the face of a death that was all too often inevitable, even as a result of what we nowadays regard as minor illnesses.
But warfare is the mother of invention, and the Second World War vastly accelerated the development of medicine. Antibiotics, for example, developed rapidly by being tested in battlefield conditions. “We’d never have taken the risks in peacetime,” Dr. Doris Howell, a professor emerita of pediatrics at the University of California at San Diego Medical School, said caustically. “You don’t have to worry about ethics during a war.”

“And with penicillin,” Herbst said, “and with a couple of other drugs thrown in there, we, in a typical American fashion, just like in the Industrial Revolution, took off on another technological revolution. We’ve got drugs! We can fight things! We can make things better! We can change from these compassionate, hand-holding physicians into real fighters..,. We were absolutely convinced that if we threw enough money and technology into a problem, we could solve it. And then cancer really stymied us, and there was suddenly this realization that we aren’t going to win the war on cancer. Not in one drug, not in one Nobel Prize-winning breakthrough.” Medical science, which had seemed irresistible, had met its match, not only in cancer but subsequently in AIDS and, though this had somehow been overlooked in the heat of everyone’s enthusiasm, in death itself.
This has radical implications for how to treat patients with potentially terminal illness, how desperately to try every possible treatment before acknowledging death.
“I’m 47,” said Dr. Mary Margaret Loehr, codirector of the emergency department at Scripps Memorial Hospital, Chula Vista, and also a per diem physician at San Diego Hospice, “so I graduated from medical school in 1973. I was taught, as were all the physicians older than me and many physicians even younger, that it was my moral, ethical, and legal obligation to do everything I could for every patient.
The difference was that even in 1973, while we thought we could do a lot, say, in comparison to my father’s generation, compared to what we could do now, doing everything is nothing.
“When I was a medical student, taking care of an elderly patient with pneumonia, I ran out of drugs after one or two tries — even if I was excessively aggressive, I only had two or three weapons. Now we can be excessively aggressive for months and go down a whole formulary. So the inherent physical limitations on a physician’s ability to continue to intervene have been pushed back; and as a physician, to watch it happen — it’s staggering. We only used to put really pretty healthy people on dialysis; now we put 90-year-olds on it. So that as a physician, if I was inappropriately aggressive 10 or 15 years ago, the body stopped me anyway. Now that frontier is really pushed back, but the training hasn’t changed.
“And the other piece,” she continued, “is that as a physician you are trained that you must do even more for your patient than you would do for yourself or your own family. You leave your kids and your wife at home, and you get up and go to the hospital at night to take care of John Jones because he’s got chest pain. That is what you do, that is your ethic, that is your standard: do more. And we can talk a lot about rich physicians and all kind of other garbage, but by and large the huge mass of physicians has been trained — whatever it takes, whatever it costs, personally, professionally, economically, you must do whatever you can for your patient. The idea that we need to stop thinking in terms of doing whatever you can and start thinking in terms of doing what is best was never even before a question. Never had to be explained, because whatever you could do was best, and the best for the patient was whatever you could do, and they were equivalent in the medical thesaurus. They aren’t anymore.
“Within one generation we’ve gone from hand-holding to true therapy. Her father and grandfather were physicians, and there was a time when all they could do for someone with pneumonia was to hold their hands; they were part physician, part father figure, part shaman, part pastor. If they were called at 2:00 a.m. and told that someone had pneumonia, they knew that their job consisted of going to and sitting with the patient until he or she died. Now, her grandfather pointed out, when she is awakened at 2:00 a.m., whether she’s alert or not and whether she’s thinking or not may decide whether the patient lives or dies.”
Doctors were changing, medicine was changing, and hospitals were changing, developing their own gravity, drawing the practice of medicine toward them. It’s no coincidence that around 1940, for the first time in history, more babies were born in hospitals in the U.S. than at home. With medicine becoming ever more scientific, and its scientific equipment becoming ever more expensive and ever more centralized, and the public constantly tugging at the doctor’s sleeve, begging him to do something for the dying relative, between 1945 and 1995 the majority of Americans made a change that would previously have been unthinkable. We chose to die in the hospital.
A TERRIBLE PLACE TO DIE
Of course, we don’t see it that way. We rush to the hospital to try to avoid death, which is precisely the problem. The place that Is designed and equipped and staffed to avoid death is bound to convince both patient and family that death is one of the worst things that can happen. The flashing lights and the siren of the ambulance, the muttered orders, the efficiency and haste, the blinking lights and beeps of the monitors — everything that conveys urgency also conveys panic and implies meaning: that death is to be avoided at all costs. When else are tens of millions of dollars of equipment rushed to our disposal? For what else are we charged $5000 a day? It must be a terrible thing, this death, for us to mobilize such forces against it. If we detest hospitals so much — and it’s hard to find anyone who doesn’t — but we go there to die, it must be because we’re even more afraid of death than of hospitals. But hospitals convince us to fear death...and down we go in a whirlpool of fear and circular logic.
Once the heroic measures are clearly not working and the urgency fades, the hospital becomes little more than a warehouse in which the patient is stored (at enormous expense) until he dies. “You feel guilty [because] it becomes part of your routine,” explained Ester Sarabosing, R.N. “You’re not really spending time with them. Often they’re the last person you deal with because you think, well, they’re dying. For the first few days, for the first week, you spend the most time with them, but after that they become your last priority.” She told me the story of a man who was expected to die quickly but clung on for two weeks. During the first week his wife visited every day; on the second week she was down to an hour or two. “I was uncomfortable. He was no longer here but he was still here. When he finally died, everybody was relieved.”
Part of the reason a hospital is such a desolate and londy place to die is simply a lack of time to treat each person as an individual. “We get 50 or 60 people a shift,” said Joan Snyder, R.N., who works in a San Diego emergency room. “How can you relate with everyone you see? You don’t have that much to give out.”
But part of it also has to do with the bleak meaning that mainstream medicine ascribes to death. A medical education, whether a doctor’s or a nurse’s, does almost nothing to prepare staff to help patients and families through death; it doesn’t even prepare the staff to help themselves. Instead, they learn survival. The newly qualified nurse or doctor in the busy hospital, faced with death, is supposed to sink or swim and to learn to do so alone, without help, without any recognition, even, that he or she may be drowning.
“It’s very, very overwhelming to new nurses to deal with death on a daily basis when you don’t have time to deal with it,” Snyder explained. “It leaves a lot to be desired. It’s not discussed. They watch what you do, and if they see that you’re coping successfully with the attitudes you have, then they adopt them. In nursing school they never teach you about death. They don’t teach you about you, about your profound feelings about death and dying. You don’t know what to do about the anger and sadness that you feel when you have to deal with a newly diagnosed cancer or a person who’s just become a paraplegic or a quadriplegic. After a while you develop a [surviva] attitude, and if you haven’t got that, you flounder.”
When a medical student or student nurse does encounter death as part of his or her education, it often happens in a grim and harrowing fashion that may bear little or no resemblance to an actual death. Ester Sarabosing grew up in the Philippines; her first experience of death was that of her grandmother. As a young girl. Ester knew her grandmother as an active, alert woman. As she aged and became senile, Ester, by then a teenager, cared for her, as she was expected to. When her grandmother finally died, the whole family mourned and missed her, but Ester learned no fear of death from the experience.
Curiously, when I asked her about her first experience of death, what sprang to her mind was not the peaceful and natural death of her grandmother, but the dissection class in nursing school and the smell of formaldehyde. “What I remember most vividly is my first year of nursing and the smell of my first time in the morgue. When we had to go to the commissary afterwards to eat, the smell stayed with us and lingered for a week.”
It’s all too easy for that survival attitude to be simply a kind of emotional insulation, a just-do-your-job-and-get-on-with-the-next-case teeth-gritting that to the outsider can seem callous. The traditional hierarchy of the hospital makes it easier for the doctor to avoid the emotional content of death than for the nurse, who is left to deal with the aftermath, like the wife being left holding a soiled diaper while the husband goes off to work at Paine Webber. “The physician goes in,” Joan Snyder explained, “and tells the family that their loved one is dead. ‘I’m very sorry. I did the best I could, and my nurse Joan will take care of any problems you have.’ They have at most a five-minute involvement with the family, and then their duty is ended.”
Medical education is crucial, because medical personnel in turn pass on their beliefs about death, directly and indirectly, consciously and unconsciously, to the public — to patients and their families. “They don’t teach them that it’s okay to die at home,” Snyder said. “They don’t teach them that it’s okay to die. They give them the impression that there’s still something to be done, when there isn’t. They’re told, ‘We can do this, and this, and this,’ but they don’t say that they’re going to die.”
The more I listened to the medical personnel, the more the hospital, the institution, began to resemble Fortress America, that symbol of embattled solidarity that recurs with curious frequency throughout American history, from the earliest European settlements through the Alamo to Khe Sanh and Waco. Maybe it has to do with a militaristic mindset or a failure to conceive of community as the basis for civilization; but as in Vietnam, we’ve trucked and helicoptered in the most modern equipment and the most highly trained troops, and once again they’re in danger of being overrun. The hospital simply cannot fulfill all the roles expected of it.
“It goes back to the family and the support system,” explained jeannie Binder, R.N., of Scripps. “Most of our patients could be at home. There are not many things that need to take place within the hospital walls. There’s not any magic to delivering morphine or suctioning the patient. There’s no place for a hospital as we have them. Why should you spend $1000 a day just to be in here, to get this food, when you’d rather have a bowl of chicken noodle soup or a bologna sandwich anyway? If you’re a smoker and you want that last cigarette then, Jesus, you should be able to have it.”
All the parties involved conspire to make death harder. Death with dignity is easier for all concerned if the patient is informed about his condition, has considered the treatment he wants (or doesn’t want), and has talked it over with his family. But the double role of the hospital makes denial vastly more common. Edna Monzon, R.N., reported that although most of the intensive care patients at Scripps are 75 to 90 years old, and most have been in here time and again with chronic illnesses that will finally kill them, most have refused to think about death, let alone plan for it. “A lot of the time the family thinks, ‘This is just one episode. He’s a fighter. He’ll come out of it.’ So when they come into the hospital, they’re still hoping for the best; and when the patient turns sour, it’s hard for the nurses to get through to them.”
Meanwhile, most medical staff don’t have the time, the training, or the inclination to help a patient talk about his approaching death or help the family with their grief. Many physicians (and some families, especially those of Hispanic and Asian origins) still believe that a patient should not be told of a terminal illness.
“A person who’s diagnosed with a terminal illness should be told up front,” Joan Snyder said forcefully. “That’s where I think hospice is just great. They say, ‘We’ll teach you.’ There’s so many things to learn, and you only get to go through it once.”
Meanwhile, the need for sterility and efficiency creates its own diminishing returns. The patient feels like a stain on the crisp white linen, an inconvenience to the crisp running of the staff s schedules. The more miraculous and effective the technology, in theory, the more the physician, too, becomes a liability. As one doctor has written, the machinery of medicine needs to be infallible, which leads the physician to feel that he, too, must be perfect or else be shown up as the weak link in the system. In practice, no hospital has that kind of budget. Instead, everyone is aware of the space they don’t have, the equipment and the time they can’t afford. By thinking of medicine as something pharmaco-technical, we have helped to create a climate in which bitterness and frustration are epidemic. Death is simply the occasion when these feelings arise most vehemently.
Last fall I followed an old rum-runner’s trail up into the Green Mountains of Vermont, past a trout lake and up among the birches and blazing maples. Leaves rustled and crackled underfoot, sometimes six inches deep, and the silence of the woods was constantly punctuated by falling leaves and twigs. Above an abandoned beaver pond with its lodge and dam of grayed branches, one entire hillside had lost its leaves early, and the exposed branches and twigs blended into a mass of woven silver thread. Everywhere else the maples were crimson, red-gold, orange, yellow. What a paradox, I thought; in a hospital we try to avoid and conceal death, and as a result we create an utterly alien setting, a cross between a stationary submarine at permanent battle stations and a warehouse stocking nothing but sickness and blank suffering. Out here, time and change, growth and death, are unavoidable, are everywhere, yet the landscape was inexpressibly soothing, and the bad mood I’d started out with quickly evaporated, leaving me both alert and peaceful. It would be no great shame if I were to die here, I thought; and who knows if our panic and hand-wringing in the hospital corridor are at the thought that someone is dying or that someone is dying the wrong death, in the wrong place?
IN THE ICU
In the intensive care unit of a hospital in San Diego County, I catch a glimpse of a man splayed in the characteristic abandon of unconsciousness or a baby’s sleep, mouth gaping, an unnaturally beige-chosen-as-skin-color pair of tubes running out of his nose. It’s hard not to imagine it’s the other way around, and they are snaking into the nearest available orifice while he sleeps. In the next room is a Jane Doe. She is reaching feebly for the gadget that adjusts the electric bed, but her hand is entangled in her IV tubing and she can’t reach it. Nobody notices. At the tiny nurses’ station opposite, surrounded by beeping cardiac monitors and small black-and-white, closed-circuit screens, a young nurse has just gotten off the phone. “Can you believe it?” she is demanding of the four people gathered in the narrow hallway. A patient’s next of kin can make it over from Texas, but they have nowhere to stay and want to know if they can sleep in the lobby or on the floor of the ICU. “Can you imagine?”
As I was interviewing hospital staff in San Diego County, something Joan Snyder told me kept turning up in my thoughts. “I'm not Catholic, but I’m very, very sorry that Catholics have given up on the Last Rites. We serve a very large, very Catholic Hispanic community, and it’s a great loss when there’s nobody there to say, ‘Your loved one is with God....’ It’s been years and years and years since I’ve seen a minister or a priest or a rabbi come to the ER. If they’re a religious kind of people, they need that support now. Not three days down the road.”
Come to think of it, I’d never seen a chaplain in a hospital either, though I’ve seen a chapel. (Not that it means much. Even airports have chapels.) Surely we could use some spirit-lifting, even when we’re temporarily ill, let alone when we’re terminally ill. And I remembered a study that revealed how a great many ministers are just as uncomfortable about death as anyone else, and a story of a chaplain who would never go into the patients’ rooms but tried to talk to them from the doorway.
Glancing through the Yellow Pages under “Hospitals,” then, I was surprised to see “Chaplain” listed as one of the departments of Paradise Valley Hospital. How can a chaplain function in a modern hospital? I wondered. What good can he do?
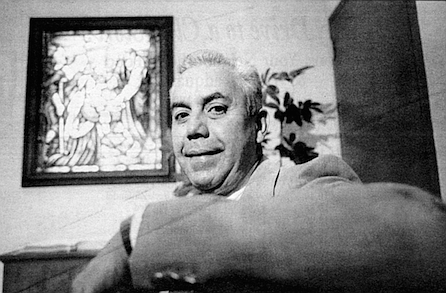
Chaplain Wilfred Reyna turned out to be a well-built man of medium height, possibly in his mid-50s, with magnificent eyebrows and silver hair brushed neatly back from his temples, dressed in a dark blue blazer, striped blue shirt, and tie. He spoke quietly, carefully, perhaps a little regretfully, with a slight accent I couldn’t place. His office was tidy and formal rather than warm.
In his 14 years at Paradise Valley, he began, he felt that he had done “an imperfect job of trying to provide a spiritual presence in the hospital.” The fact that the hospital, which is affiliated with the Seventh-day Adventist Church, gives him an office and employs him full-time is a sign of its commitment to its patients’ spiritual needs, he said.... An unspoken “but” hung in the air.
“We’re supposed to be more focused on the spiritual dimension, but what comes across to the patient depends on the personalities of those whose lives are touching the patient’s. There are a few doctors, unfortunately very few, to whom the religious aspect matters. They may stop me in the hall and say, ‘Oh, chaplain, I just diagnosed a patient with terminal c.a. (cancer, that is, in the usual hospital abbreviation/euphemism). They and their family may need some support from you.’ Many doctors are very uncomfortable leaving things to a higher power, to something beyond what they can control. If it’s not measurable, it’s not credible. With the majority of doctors, only when the patient is near death will they say, ‘It’s in God’s hands.’ ”
This makes perfect sense. The medical profession, too, has its faiths and its creeds, some of which stand in stark contrast to those of most religions. Every visit to the doctor is an opportunity for secular proselytizing, a chance to reinforce our belief in scientific materialism. I had a vision of the chaplain bobbing unhappily around a ring of medical personnel surrounding a patient like a stockade.
His self-appointed rounds go roughly as follows, he said. First, a brief devotional service—“a thought, a prayer, sometimes we sing” — with perhaps two dozen patients and staff in the inpatient psychiatric unit, then around 10:00 a.m. a similar meeting with the outpatient psychiatric group....
His beeper went off. Code blue in the emergency room, the dispatcher’s voice said. “I have to do that as well,” he said, half-apologetically. I asked him if he needed to leave at once. No, he said, glancing at the clock; for a code blue he would probably be needed for the family rather than the patient, “who is surrounded by doctors and nurses and technicians,” and it would probably be some time before the family arrived. It was about 3:20 p.m.
“After that, I drop into intensive care and post-intensive care,” he said, continuing to describe his daily routine, “and I try to visit the other floors if I’m not being paged too often. I’d have to say my work is basically crisis driven.”
Despite the hospital’s Adventist affiliation, he said, it was his job to try to minister to all faiths as best he could or bring in colleagues from the community. “I try hard to be a generic chaplain,” he said, smiling a little thinly. He once stayed with a grieving Japanese woman for two hours, he said, finding out eventually that she was Buddhist.
He was paged again and called the ER. As he listened, he made noises of concern, and his face was grave.
“Bad news?” I asked.
“A baby,” he said. “Didn’t make it.”
Almost immediately he was called again. The family had arrived. He invited me to follow him, and we headed briskly down the featureless corridor.
“This is a shortcut,” he said, and we passed from the groomed corridors of the administration section into an area that had the combination of elementary school and medical supplies warehouse that is instantly recognizable as an emergency department. Reyna looked a little hesitantly at the group of three nurses, one of whom directed him to a doctor in an impossibly small cubby-office behind their station. “It looks like suffocation,” the doctor told Reyna. As they spoke, I glanced through the open door of the room adjoining them. I caught sight of a bed that was empty — no, occupied at the far end only: some tubing and a small white blanket and something dark in it. Two young cops appeared beside us in yellow rain slickers, and it struck me that nobody knew if we were dealing with accidental death, SIDS, or murder.
The family was in a small room at the end of a short corridor — the mother, a beautiful young Japanese-American woman with the kind of skin blemishes that sometimes come with bad diet, and the father, an African-American in a maroon sweatsuit and Reeboks, nearly six feet tall, and built like a running back. She was wearing skintight pink exercise pants and boots. I honestly can’t picture what kind of shirt or jacket she was wearing. All I can see is her crying into her long black hair and her empty hands, held in front of her as if she were tom between wanting to reach out to hold someone and wanting to clutch her head. “My baby,” she cried. “My baby. My baby.” A young hospital social worker, in her 20s, was sitting next to her saying in an oddly upbeat tone, “This is the worst thing that can possibly happen.”
The father seemed to have frozen, staring at the floor. A nurse was taking their names, but he seemed not to hear anything she asked. Reyna tried to pat his shoulder, but he shrugged him away furiously. With each moment the father seemed to withdraw further, to become almost catatonic. Afterwards, Reyna told me he couldn’t decide whether the man was in shock or was trying to concoct a story to cover his actions.
Nothing was clear. The father had been at home, the mother somewhere else, apparently. They’d last seen the baby alive, asleep, at 9:30 or 1:00 a.m. The father had taken his daughter—by a previous marriage? — to school at some point and had then taken a nap — When? For how long?
Nothing fitted together. The baby had been lying oh “a big bed,” because they couldn’t afford a crib and had fallen or slipped into what the mother called “a hole” — a crevice between bed and bumper? The father had tried CPR, they said, but when was all this? The doctor had said that the baby had been dead for a couple of hours....
The door opened and another young African-American man peered in, and at once everything changed. The father recognized him, jumped up, and for a moment the two seemed to be wrestling, but then the father burst into tears, wailing, thrashing, while the other tried to comfort him and at the same time pin him down on the couch. The chaplain stepped back, nonplused, and I didn’t blame him — either man could have floored both of us in a second, and we still had no idea if we were dealing with a man who had just killed his own son.
“He’s all alone,” the mother said pitifully. “He’s all alone.”
One of the cops came in and stood uncertainly by the door, making the tiny room even more crowded. The newcomer turned out to be the father’s brother; the bereaved family’s other two kids were staying at his house for the time being. By now the mother, who was being ignored by the two men, was asking if she could see her baby, and it made sense all-around to usher her out into the corridor, leaving the two men together under police supervision.
Even so, nothing was easy, and Reyna’s job demanded that compassion be tempered by protocol. The parents couldn’t touch the baby, who in a grim way had taken on a new identity. It had become evidence. Reyna explained hesitantly that the coroner would shortly come and take the baby away to examine him. “Exam -ine?” the mother asked, uncomprehending. “Conduct a...post mortem,” Reyna explained awkwardly, “to see how your baby died. He’ll be done by...maybe tomorrow afternoon. Then you can make arrangements with a mortuary.”
Post mortem. Arrangements. Mortuary. Death involves a great deal of novelty, many difficult changes of direction and perspective. Taken one at a time, we can steer around or through them, stiffly, uncomfortably. When they arrive all at once, it’s like hitting a rock face.
The room was both barren and cluttered. All around the walls was the familiar ER paraphernalia, boxes and bags of sterile supplies, notices, like a large poster for “Easilav Adult Lavage System," that meant nothing to the uninitiated. All this and you couldn’t save my baby.... I’m injecting my own feelings here, I know—for the parents seemed oblivious to everything but the baby — but I could see how people could take the blank sheet of death and paint onto it their own feelings of the moment. This room was a self-fulfilling prophecy, the comfortless desolation of the room could all too easily become the comfortless desolation of death. By assuming clinical death, meaningless death, the final breakdown of the body’s systems followed by nothing at all, medical science and medical architecture have created an environment in which death can be little other than that. The context becomes the feeling and the meaning.
And a vicious circle starts spinning. The more empty and meaningless death seems to be, the more afraid of it we become, the more we tug at the oncologist’s sleeve, whimpering, “Please, doc, can’t you do something?” and we commit ourselves to the stainless grasp of a medicine that becomes ever more expensive, ever more invasive, ever more sterile. By running from it, we create the death we dread.
The mother was pleading to hold her baby. Reyna looked uncomfortable and went out to the hallway to talk it over. The group of nurses at the counter reminded me, bizarrely, of waitresses at a truck stop.
The nurse Reyna was talking to shrugged. “What are they going to do by holding him?” They looked at each other uncertainly for a moment, then Reyna went back in to the mother and told her she could hold the baby. “It’s against hospital protocol,” he muttered to me under his breath, looking unhappy.
The mother picked up her son carefully, as for some Dr. Laurel Herbst reason he was still attached to a tube and gathered him in the hospital blanket, which looked exactly like a receiving blanket. “My baby,” she repeated helplessly.
Back in the little waiting room, the father eventually pulled himself together, refused a sedative, and asked, a little belligerently, if he could see his baby. How could he know what he would and wouldn’t be allowed to do and what he might have to fight for? “Of course,” someone said, and he went down the corridor. When he saw his son, he seemed stunned. “He ain’t dead,” he said. “Look at him. He ain’t dead.” The baby looked asleep. He had reached the age when children look physically perfect, but still helpless. He had stunningly beautiful eyebrows, jet black against his lighter skin, and unusually straight and well defined, like acts of calligraphy.
This must be as bad as it gets. Sudden death, whatever we may say about wanting to go quickly, without knowing what hit us, creates the hardest grief to heal. Sudden infant death is the worst of all. The previous day, Susan Inot, director of maternal-child health at Scripps, had explained to me how they deal with stillbirth, bringing the baby to term and delivering it, encouraging the parents to claim the baby as their own. The labor itself gives the family time to take in what is going on, she explained. But here — this is the brick wall.
The father crouched in a corner, holding his head in his hands, muttering, “It’s my fault. I shouldn’t have...I’m supposed to be his father. How could I...” in a desperate monotone. His brother and one of the cops had disappeared; the other cop, a baby face on a huge body, wearing so much equipment on his chest he looked as if he were about to erupt with some spiky mechanical, alien, stood unobtrusively in the background, and I, for one, was glad to have him there. It no longer mattered who had done what. Someone that upset might do anything, might take sudden and furious offense at my presence or that of the chaplain (whom he had still barely acknowledged) or the social worker, who still seemed oddly chipper.
The mother stood at the head of the gurney, crying, asking Reyna questions he was wise enough not to try to answer.
Every so often he patted her on the shoulder. At a glance, the chaplain might have seemed to be doing almost nothing, but there was almost nothing to be done. Certainly, this was no time for pious platitudes or religious pronouncements that might actively irritate the family, given that their religious beliefs, if any, were still unclear, like the social worker, he was there; and if she was taking advantage of her youth and gender to offer more obvious comfort to the mother, he was better able to offer the calming presence of one who has seen more of the world, that parental gravity and stability that we sometimes want to cling to. In a colloquial sense, at least, this is a spiritual gift, if not a religious one. But all this is guesswork. They might not even have known he was there. The belief that he does any good must also often be an act of faith.
For what it’s worth, I was also engaged in an act of faith. I imagined myself sending my soul out to them, gliding across the room like a manta ray to embrace and comfort theirs. I felt like the angel in Wim Wenders’s Wings of Desire, watching them full of compassion, standing in another dimension. The parents, of course, paid me no attention at all. Who knows if this can really happen and you really can send your soul out flapping across the room like a sand ray, and even if you could, whether it would do any good or whether it’s just an act of well-intentioned self-deception, and you would just exhaust yourself in the process trying.
In the end, it was the mother who established the father’s credibility, if only temporarily, by forgiving him. “It’s not your fault,” she told him over and over, through her own tears. “Don’t blame yourself.” They formed themselves into a tight little protective knot, the mother with her arms around the baby, the father with his arms around the mother, and that’s how I last saw them, for a minute or two later a capable-looking woman in her 40s, wearing jeans, a plaid shirt, and a yellow rain slicker, arrived and announced that she was the crisis worker from the police department. “Looks as if you’ve got more than enough people here already,” she said, but the hospital social worker and the chaplain handed the situation over to her with some alacrity, and Reyna and I made our way back to his office.
For the chaplain, too, everything happens too quickly, and unlike the nurses and doctors, he doesn’t have another case waiting that will at least give him something to do with his hands, a chance to do better this time, to draw him back into his sense of his own value. When I left them, they were a bundle: the mother holding the baby, the father holding both of them, the worker from the crisis intervention program with her arms around them all.
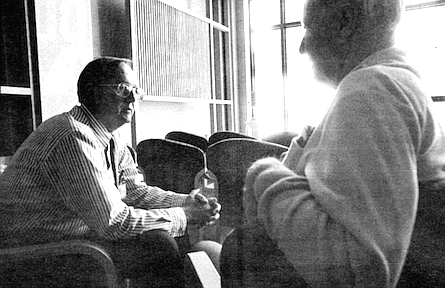
“Who looks after you?” I asked Reyna as he sat back down behind his desk.
“That is an issue,” he conceded, and sighed. “If I’m going to be effective, I have to be affected.” He paused. “I don’t have anyone in whom I confide. I have a lot of clergy friends, but clergy are used to being... prescriptive. I need someone to enter into it with me and go down into my valley, and only then can they help me.” He might have been talking about doctors, I thought.
He deals with the stress, he says, by trying to keep fit; he has NordicTrack in his bedroom. “My doctor told me I have the blood pressure of a 20-year-old,” he said proudly.
We shook hands and I left, feeling suddenly drained. What was most demanding was not the act of sympathetic connection, which has the sublime, sustaining quality of any act we believe to be wholly worthwhile. It was the re-entry afterwards into a world that seemed much more mundane and therefore, in a curious way, harder to take. Back in heavy traffic on 1-5, a sudden headache hit me like a squall line, and I felt very tired. If I were an ER nurse or doctor right now, I’d be denying my next patient something by having allowed myself to be so affected; but then again, if I didn’t allow myself to be affected, wouldn ’t I be denying myself something? One of the wisest things we can know, it seemed, is who we want around us when we have to grieve.
When I headed up the Coronado bridge between the patchy lights into the rain and darkness, it looked as if I were driving off the planet.
ABOUT THE AUTHOR
At this point, I should put my cards on the table. In 1979 my father died what I have come to think of as the standard brutal aggressive-oncology death, in England. After six months of increasingly disturbing symptoms, he was told he had cancer of the lymph system. Not to worry, the specialist said, they’d try this; and if this didn’t work, they’d try that. Chin up, what? Heavy, then heavier doses of radiation left him looking bruised and yellow, with a perpetually dry mouth; chemotherapy made his hair fall out and left him vomiting; and, just as importantly, he was subjected to the continual humiliation of being in a large hospital with a good reputation, treated like an infant, treated like a disease.
My mother was only allowed to see him during visiting hours, and she, too, was treated with routine dismissal, even though on a dozen occasions she found that he was being given the wrong medication or the wrong dosage. She ended up being a de facto private nurse, but the privileges that went with this position included only being allowed to give him suppositories; even though she begged the hospital to allow him to be released into her care so she could look after him at home, they refused, saying that untrained members of the public couldn’t be allowed to administer medication.
He eventually died in the hospital, alone. She, too, was alone, in a way. She had looked after him by herself, and his death left her carrying all his pain, his anger, his humiliation. It was too much to bear, but it was also too terrible to talk about, and it created a silent, dark divide between her and her children, whose grief was preempted by hers.
Fifteen years later, she, too, was told she had cancer, but instead of going into the hospital, she signed on with the local hospice. Her death was a completely different experience. She stayed at home in her flat with its sunny garden, surrounded by paintings she had painted and furniture she had carved, almost the entire time until she died. The medical personnel talked to her as an equal and saw her on our own turf; the whole family was involved, caring for her in shifts, constantly talking to her, to each other, making sense of what was going on, growing closer to her and to each other until it became clear that her death, though a tremendous loss, was a transaction involving gifts, too, that would enrich the rest of our lives.
THE HOSPICE ITSELF
Let’s clarify terms. While “a hospice” is usually a building, sometimes part of a hospital, sometimes a freestanding building with or without inpatient facilities of its own, “hospice” usually refers to the hospice movement in general and its attendant methods and philosophies concerning care for the terminally ill. To be “in hospice” doesn’t mean one is in the hospice building; it’s much more likely that one is “on service” (that is, receiving hospice care) at home.
There are five places a hospice patient might be at any given time.
• Ideally, at home, but this is possible only if the patient has a home and has family or neighbors able to give more or less continuous care.
• The acute-care center, if the hospice has one. This is for short-term medical treatment that can’t be done at home. (Of course, traditional thinking holds that nothing can be done at home, and the family is a bunch of meddling bumblers who, under no circumstances, should be put in charge of, say, morphine.) Most hospices deliberately have very few beds and try to send patients home after a couple of days, a week at most.
• Some other form of “managed-care facility” — in other words, a nursing home (or “convalescent hospital,” as they are now sometimes grandly styled) that has a contract with a hospice. Most often used when a patient has no family support and can’t live at home alone.
• A respite house, a stand-alone building specifically designed for the needs of the dying — that is to say, filled with light and flowers and music One respite house in Vermont runs the best children’s art program in the state, filling the place with life. A respite house fulfills the same needs as a managed-care facility, but usually much, much better.
• A hospital. Not for treatment, usually, but for respite. A number of hospices without inpatient beds have agreements with local hospitals that the patient can go in for a few days just to give the caregiver(s) a break.
Despite these various manifestations, the philosophy of every hospice is essentially the same: We will do everything we can to help you live what remains of your life as fully as possible. In its most clinical sense, this involves palliative medicine — that is, treatments aimed not to cure but to make life as comfortable as possible in the face of the old enemies, pain, nausea, vomiting, and constipation. In a broader sense, it involves taking care of the emotional and spiritual burdens that may be harder to bear than the physical pain. At this final stage of life, being separated from one’s dog or having unpaid bills may be more disturbing than simple pain.
At its most profound, hospice invites patients to turn their entire view of life around. Now that you know you have perhaps only a few months to live, why put off doing what you have always denied yourself? Why be afraid of other people’s opinions? Why carry that grudge against your sister? This approach not only transforms death, in some instances it transforms life, both of the dying and of those who are near them. For we are all, in effect, terminal; hospice encourages us to do what, if we’d had any sense, we’d have been doing all our lives.
SAN DIEGO HOSPICE
In a metaphysical sense, hospice exists wherever its patients live. In a postal sense, the San Diego Hospice consists of two linked buildings standing at the end of Third Avenue in Hillcrest, perched on the lip of Vauclain Point, overlooking Mission Valley. Across the ravine, the UCSD Medical Center juts up behind a fringe of trees, looking for all the world like a huge concrete waffle stood on end.
Even in a city of buildings competing for the attention of a roaming editor of Architectural Digest, the San Diego Hospice buildings are quietly remarkable — low, earth toned, looking somehow American, Japanese, and Mexican simultaneously, joined by two graceful arbors encircling a driveway in the middle of which is a single astonishing tree, a native of South Africa called a Naked Coral. Sinuous yet compact, it manages to look both startling and wise, as if the Tree of Life and the Tree of the Knowledge of Good and Evil had been interbred by a celestial gardener.
I’ve visited some half a dozen hospices, and the parking lot of the San Diego Hospice is bigger than any of them. Indoors, the buildings are furnished in what might be called the school of hospice art, transcendent but ecumenical: a fan-shaped soft sculpture in handmade paper, textured walls and carpets blending dove-gray and quiet blue, a sculpture of a dove, and a photograph of someone hang-gliding off a cliff, its symbolism lofty and hard to miss.
The hospice is considerably older than its headquarters. It was founded largely through the efforts of Dr. Doris Howell, a physician with an extraordinary pedigree in hospice. She is a friend of Cicely Saunders, founder (in 1967) of St. Christopher’s in London, the first modern-era hospice, and was also named to the board of the first U.S. hospice, founded in 1974 in New Haven by the dean of the Yale School of Nursing. She herself subsequently founded a children’s hospice in Philadelphia, though it did not survive when she left for the West Coast to become a professor of pediatrics at UCSD. She pooled her experience with members of Episcopal Community Services and other community figures, and the result, in 1977, was a small-budget, community-based home-care hospice run along the lines of a largely volunteer home health agency, as many hospices are still run today. One particularly lean year, she paid salaries out of her own pocket. The first physician hired, in 1978, was Dr. Laurel Herbst.
At the time, many in the medical establishment saw hospice as a grassroots community service that essentially acted out of charity and had little serious clinical significance — a professional dead end. Dr. Herbst found this out in the fall of 1978, at the second annual Scripps Memorial Hospital Cancer Symposium in San Diego, a national conference that is now a very big deal and was even then gathering momentum. Herbst, who had been at SDH only a few months, went to the conference to get continuing education credit for her medical license and to make contact, on behalf of the fledgling hospice, with her colleagues in the medical community.
As she expected, she knew a fair number of people at the conference from her training programs in Los Angeles and San Francisco, and they were delighted to see her after her nonmedical sabbatical in Colorado. “When I told them what I was doing, they would say, ‘Oh,’ and back away from me. It was so disturbing I actually had to leave the conference.”
When she went to the same conference the following year, people were a little more curious, asking, “Are you still with hospice?” The third year she went, the question became, “Are you still with hospice? Can I talk to you? We’re thinking of starting one in our town.” By the fourth year, she was finally being accepted as a colleague, and hospice as a viable field of work. “Let me talk to you about a case I had. What would you have done?”
SDH might have remained on this modest scale, but in the mid-1980s it was blessed with the kind of sudden, unexpected benefaction that every nonprofit organization dreams of. At the time, the organization employed perhaps two dozen people, but was modest enough to use Herbst as doctor and bookkeeper, because she was the only one who understood step-down accounting. Joan Kroc, widow of Ray Kroc (cofounder of McDonald’s, former owner of the San Diego Padres), was so impressed with hospice care her father received in Minnesota that she paid the bills — $18 million in all — for SDH to buy land, build buildings, furnish them, set up an inpatient facility, and be a teaching center for the philosophy and practice of hospice care. In December 1990 the home-care administration building was opened; the 24-bed acute-care and conference building followed in July 1991.
Any nonprofit that receives such massive one-time capitalization has to run hard to keep up with its good fortune, and it’s not surprising that soon afterward some 20 or 30 employees were laid off or that the administration (though not the medical staff) has seen a high turnover in the last four years. At the moment, the roughly 240 hospice employees work within an annual budget of some $12 million to serve about 220 patients (205 at home, 15 in the acute-care center), the whole census down from a peak of perhaps 250 last summer.
SDH operates in four teams, each of which oversees some 50 patients. Each team consists of nurses, social workers, home health aides (who visit two or three times a week to help with the patient’s personal care, grooming, bathing, shaving, fixing hair, and other services), homemakers (who visit weekly, doing light housekeeping, light cooking, and laundry), chaplains, and volunteers (who sit with the patient a minimum of three hours a week, offering respite for the primary caregiver to get out of the house to exercise, go shopping, or just have a break), plus a team director and a secretary for administrative support. All of them carry out the kind of paramedical functions that hospice is all about — chatting with the patient, bringing a cheery face into the home, passing the word if a clinical or spiritual visit seems to be needed.
This is, to put it mildly, an unusually well-staffed team; many hospices rely much more heavily on volunteers, and their smaller staffs find themselves spread far more thinly. Even in smaller hospices, though, this team approach, which also includes a hospice physician and the patient’s family and neighbors, changes altogether the alignment of medical power. The top-down hierarchy simply makes no sense when most of the clinical work will be done by a nurse and when the greatest amount of care in general comes from the patient’s family.
The hospice physicians, of which there are currently two full-time and several per diem, provide medical care in the acute-care center and also for home-care patients needing consultative conferences every other week. But the familiar power structure is completely altered in favor of a more egalitarian flavor, which many physicians find deeply disturbing. It’s as if they came upon the Empire State Building lying sideways along Fifth Avenue. From the patient’s point of view, though, the totalitarianism of the hospital is finally overthrown. Not only are they in their own homes, eating what they want, not being awakened at the crack of dawn to have their vital signs taken, but they and their families are respected as members of the healthcare team, for the simple reason that any other way doesn’t work.
All except the volunteers are paid; SDH is required by Medicare to provide all those services professionally. Medicare also requires that SDH provide bereavement services, though it doesn’t reimburse for them. Perhaps three-quarters of the SDH patients are covered by Medicare, which reimburses SDH about $102.33 per day; patients pay a 5 percent copayment for their pharmaceuticals used at home, and that’s it. Others are covered by MediCal, by insurance through their employers, or by an HMO; each plan has a different hospice benefit, but it’s usually comprehensive. A small category of people — the working poor, under 65 and either uninsured or underinsured — falls between these categories and has no means to pay. If they can, they pay out of pocket; if not, SDH may carry the cost. SDH may also have to make up the costs for those whose care is unreimbursed by Medicare or MediCal — a big category. “Last year we gave away three-quarters of a million dollars worth of care,” said Lisa Gaspard, the hospice’s public relations manager.
She walked me over to the acute-care center. Each wing has what is virtually an atrium, with cathedral windows. The rooms are more like a very expensive hotel than a hospital. Every room is private, with its own patio or balcony and a large private bathroom. The floors are half polished hardwood, half carpet, with a sofabed, television discreetly hidden in a cabinet, all the medical equipment similarly invisible. “We’ve hidden as much of the medical equipment as we can behind nice tumiture," Gaspard said, opening what looked like a liquor cabinet. “This is the dirty linen cart.” The bed can be wheeled outside, and the family is invited to stay, even to bring pets.
At the moment, of course, all the equipment and furnishings are virtually brand new. Maintaining them on Medicaid reimbursements of $100 a day will be the trick.
One or two features of the place leave me a little uncomfortable. Lisa shows me the therapy-dog scrapbook, page after page of snapshots of patients receiving visits from one of the hospice’s three therapy dogs, in every one a rottweiler or a retriever gamely wearing bunny ears or a clown hat or a pith helmet or a bandana and cowboy hat. “They have a different outfit every week.” The companionship of dogs is fine, but their therapeutic value doesn't depend on bunny ears. She also showed me the “library of donors,” in which SDH has taken the name-a-brick concept and replaced bricks with books. The baby grand piano in the “library” is real, but the “books” are essentially empty boxes with the donors’ names on the spines.
Such an artifice is a sign that the SDH administration, at least, is paddling like crazy in the troubled waters of modem health care. More than a dozen hospices have sprung up in San Diego since SDH was founded, and with such competition for market share, some bear precious little resemblance to the original foundations on either side of the Atlantic. Some are attached to specific HMOs, some to specific hospitals, some are even for profit.
“Everyone’s aligning into groups,” said Gaspard. “We don’t have a guaranteed base of referrals; however, we are contracting with insurance companies, hospital systems, and physician groups.”
The idea of a for-profit hospice makes my skin crawl. Any for-profit medical establishment has to jack its charges high enough to cover not only its medical expenses but also to spin dividends out to investors, not to mention the current fad for paying HMO CEOs anything from $1 million to $6 million a year. That has to come out of money that might be spent on the patient. And hospice, above all, was founded as a means of caring for people who are at their most vulnerable, not profiting from them.
MED ED ONE: LESS DRAMATIC BUT USEFUL
The development of hospice has always depended on its ability to educate and, to a lesser degree, to research. Until palliative care, in its broadest sense, was shown to work, conventional medicine could regard hospice as little more than a cross between a home health agency and a visit from the priest — which is, in fact, how many doctors still regard it — and comfortably ignore it, continuing to broadcast its own grim view of terminal illness and death. SDH had to take the education of future physicians into its own hands.
“After we built the building, which we did in the full view of the medical school over there, we finally got the attention of the university,” Herbst said. “We had had very little contact with them for years. We’d say, ‘Wouldn’t you like us to come help teach about pain management? About talking to dying patients? Doctor-patient relations?’ And in fact they did let me give a lecture every year to the first-year students on the art of discussing prognosis with a newly diagnosed terminally ill patient. But we really didn’t have their full and undivided attention until we put up a building, and all of a sudden it was much easier to get the idea across that we were different, that we had something else to offer, and over the last three and a half or four years we’ve developed a series of courses.” . San Diego Hospice is now one of the nation’s biggest hospice teaching programs for medical students and physicians in training, hosting perhaps 200 students a year. “The family practice residents are here a day a week for a month, and during that time they spend half their time in the acute-care center and half the time in home visits. And in the home visits they’re assigned a patient to go see who needs a doctor’s visit for some reason. They go with a hospice nurse, who helps them relate the hospice team issues. The geriatric fellows actually spend a whole month here, and we just negotiated a similar program for the internal medicine residents from Scripps Green Hospital.
“We have two nursing schools who send us students, and we have a couple different experiences for those students. Some just go on one-day home visits with a nurse and get to see what goes on in the nurse’s life and get to know just a little bit about palliative care. We also have nursing interns who come and actually do their internship time here (or externship, as they call them). They spend a month or six weeks acting in the capacity of a nurse, but with a supervisor.”
Well, yes, all right — but does a quick stop in the hospice sheep dip really affect the students, who are at all other times getting a total immersion baptism in traditional Western high-tech, high-pressure, high-stakes medicine?
“At the beginning of the ten-week elective for second-year students, we assign a home-care patient to them, and their requirement is to visit and talk to that patient at least once a week for the full ten weeks and get as much contact beyond that as they like — talk to the families, etc. At the end of the ten weeks, during which we’ve presented pain management, management of other symptoms, pediatrics, grief and bereavement, and ethics, we ask them to write a paper about their experience with the patient and relate it to what they’ve learned during the class. It’s fascinating reading. Fascinating. That helps us see who’s missing it. And nobody misses it.”
Later, she sent me some of the student manuscripts. Michael Miovic has written, “I came to hospice half expecting that I might meet face to face with the moment of death itself, that mysterious passage which seems all the more mysterious to me because I’ve never seen it at the bedside. What I came away with was something much less dramatic but more useful, an appreciation for life and a glimpse of the many quiet, hidden deaths that hover around us like angels of pain in life’s journey, ready to teach us if we consent. A number of things and experiences made an impression on me in this course, but none more than the way I carried hospice home with me.
“I am married, with a stepson aged 15, and I have noticed that the more I’ve thought about issues of death and dying, the more appreciative I’ve grown of the people in my life and the more loving I’ve become in my own quiet way. Especially I’ve noticed that I’ve started to grieve their deaths in advance, as it were, in moments here and there (most frequently as I drive home from hospice). As I imagine the deaths of my wife and son, their absence in my life, the reality and inevitability of loss sinks home a little deeper and I become more grateful for all the love and blessings I currently have.
“It occurs to me, too, that our loved ones are, in a sense, always dying to us. We form unspoken images of people in our minds, fix their natures and relations to us in certain ways, live in a gauze of dreams that only half describes the figure of the present and raises the future upon a foundation of shifting ether. Yet the full reality and destiny of those we love exceeds us, eludes our attempt to control the flow of life, and I have found that as I step back from my dreams and listen to their echo, the people I love are always dying unto me in the sense that I have no option but to let them go. Today they return, tomorrow they return, but I know that one day I will let the bird out to fly and it will not come back — or perhaps it returns with different feathers, a new color. And so, I have less urge to control, to impose my will and view of things; I treasure more the magic around me, the unknown side of wife and son, both the joy and pain that emerges unexpectedly when I have less stake in the outcome and more love for the gift of process....”
Somewhere in the Valhalla of medicine, Sir William Osier is punching the air, crying, “Yes! Yes!”
THE HOSPICE PATIENT
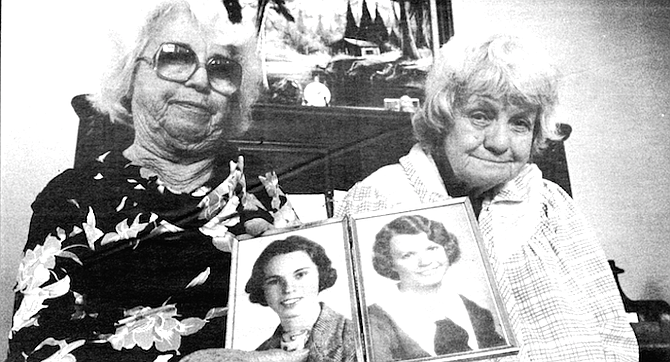
Ada and Edith Nichols live on Rancho Hills Drive in Paradise Hills, in one of the suburbs spread like butter on the earthen crust of the canyonlands above the Sweetwater River. It’s a heterogeneous neighborhood. In its front windows the nearest food market, Farm Direct, advertises pork feet, fresh blue crabs, jalapefto and serrano chilies, and milkfish. A battered ice cream van, most of its windows boarded up, tinkles and plonks through the quiet streets playing “The Entertainer Rag” and “Pop Goes the Weasel.” I am accompanied by Armando Garcia, one of SDH’s five social workers, slim, dark, neatly groomed, and nattily dressed in a dark blazer and pants.
Edith, who opens the door to us, has a pleasant, grandmotherly plumpness, wears a bright floral housedress, smiles, and talks readily. Ada, shorter and less erect, has a white thatch of hair and has safety-pinned a blue blanket like a shawl over her cotton house dress. Her ankles and feet are swollen into pads.
The tidy little living room sports large, bright, sentimental paintings of the Woolworth school, mostly landscapes. Armando and I sink into the maroon couch next to the piano, a well-worn Kingsbury that looks as if it came west from Abilene by wagon train. Ada and Edith pull up chairs and look at us expectantly.
Ada was born in Abilene, Kansas, Edith in Colorado; they moved to San Diego with their mother in 1928. Their mother lived into her 80s; their father, from whom she had separated, might have reached 100, Ada guesses.
At first, Edith does most of the talking for Ada. They first heard about hospice when someone at the hospital — Paradise Valley — recommended it. It seemed like a good idea, because the hospice would send someone over to take care of Ada’s nursing and personal hygiene. “I’m not a nurse,” Edith says, unembarrassed. “It’s not my cup of tea.” Ada says she didn’t pay much attention to the decision — probably, Armando chips in, because she was overmedicated at the time. In any event, hospice has been a blessing to both of them, they agree. “They’re real friendly and real polite,” Edith says. “They change her bandages and give her a bath.” Before hospice, Ada was left to take care of herself.
How does she feel about this phase of her life?
“It’s just like God wants it,” Ada says. “He can heal cancer as easily as he can heal anything else.”
This seems a little optimistic to me, but then again, it’s been nearly a year since she left the hospital.
“She’s a lot better than she was,” Edith says. “I think everybody lives one day at a time. Nobody knows what tomorrow will be.” This easygoing cheerfulness catches me off balance. I’ve simply never met anyone who seems less possessed by a fatal illness or has so simple and strong...what? Resolve? Protection? Buoyancy? Her comments also remind me of the research that Bernie Siegel quotes in Love, Medicine, and Miracles, suggesting that membership in a religious community correlates positively with longer life, fewer illnesses, swifter recovery. I find myself envying her.
The hospice chaplain calls ahead, then drops by every so often. “He describes world events,” Ada says affably, “leading up to the coming of Christ.”
Why does she prefer to be at home?
“Well, I can get up and go whenever I want to,” Ada says. “In the hospital you have to call someone to come and get you.” I think that maybe she’s simply talking about going to the bathroom, but I’ve underestimated her range of activities, as I will do time and again. Both sisters play the piano, which has Melodies of Praise and The Scribner Radio Music Library on its shelf. The hospital had a piano, Edith said, but you don’t feel as free to play it.
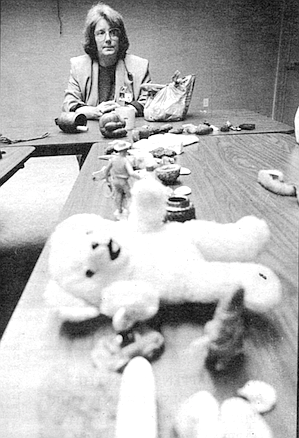
Then there’s Ada’s painting — Edith brings in a couple of oil paintings, a rural scene and a seascape, both a little blurred, but with a certain affection and energy — and her sewing. As a hobby, Edith says, they dress dolls. And give them to children?
I ask, uncomprehending. Sometimes we mean to, she explains, but when we get through dressing them, we wind up keeping them. Ada has already disappeared around the comer and now reappears with two sizable dolls, one in a satin dress and matching petticoat, one in red gingham — a little old-fashioned, but presentable enough. I should see Ada’s doll collection, Edith says. She has thousands.
Ada takes me around the house. In the “junk room” I catch a glimpse of a marimba and a large xylophone. Ada’s own room is a sunny extension, set up with the characteristic all-my-things-within-reach self-sufficiency of those who are no longer highly mobile. One little table is covered with neat boxes of ribbons and lace; another on the floor is full of spools of colored thread; patterns lie everywhere. The remaining space is taken up with dozens of family photographs, large and small, and several dolls. The commode stands beside the adjustable bed that the hospice provided. She kicks aside a cardboard box in her way, agile despite her swollen ankles, and leads me out to the back yard.
To the casual eye — mine, that is — the back yard is a bit of a mess, in keeping with the loose screens on the front door. The ground falls away gradually past a ramshackle chicken shed, then sharply into a ravine, on the opposite side of which are three rather untidy houses that look as if they need only one more decent shower to send them sliding down the small canyon and round the bend toward the Sweetwater.
But everything here has its surprises, its concealed life. A miscellaneous-looking piece of vegetation at the lip of the hill .is a mulberry tree; Desi and Kook, her niece and step-niece, take leaves into school for their silkworms to eat. On the left is a tangerine tree that I’d overlooked; it is unpruned and straggly but still has fruit. “The neighbor’s boy was up that tree at 2:30 in the morning,” Ada says. “If I’d had my shoes on. I’d have caught him, but I can’t run in my bare feet.” She reaches down and plucks at some straggling Bermuda grass. It’s been a day or two since she last did any weeding, she explains. “It helps me. I only work at it for an hour, an hour and a half maybe, and I’ve got it done.” The doll room, an overrun bedroom, is stunning. It has furniture, though it’s hard to see what. On every surface, laid out or piled up or collected into cardboard boxes, are dolls—big, small, old, pew, clad, naked. Gerbers, Barbies, Ideals, G.I. Joes, even an antique Effanbee Fluffy. At least half are in plastic bags “to keep the dirt off them.” Chuckling, Ada shows me an Army Barbie and Ken, still in their box, as is the Christie Brinkley “Real Model Coflection” doll and the African-American Costume Ball Barbie. The 1989 Holiday Barbie, Edith chimes in from the doorway, is now worth $400, though the fourth- and fifth-issue Barbies are probably more valuable. Here is the Canadian Barbie, and somewhere the English Barbie-equivalent, whose name neither sister can remember. As if to make up for this lapse, Ada shows me a boy doll in a Beefeater uniform with a threepence British stamp stuck to each of his sleeves. “That’s the prince,” she says, happily. "That’s the king of England.” Dolls are one of the three most frequently collected items in America, Edith tells Armando in the other room. Ada shows me another, a curly brunette. “This one’s been wigged,” she says, pulling off the wig to reveal a stubbled pink head. “We bought the booties. I don’t crochet.
“I started collecting them 20 or 30 years ago, because I had to have something to do,” she explains. “I can’t just sit down and twiddle my thumbs, so I started collecting.”
“Years ago I gave my son the G.L Joes,” Edith said. “Now I see them at antique auctions for $60 apiece. I paid $2.99. I wish I’d kept them now.”
By now Ada is on a roll and shows me what I take to be her only stamp album, and then another, much thicker one, packed with the glorious particularity of philatelic history; the 1929 Sullivan Expedition commemorative issue, the 1928 Aeronautics Conference, the 1929 Battle of Fallen Timbers, way back to an 1861 George Washington.
“They’re putting out Marilyn Monroe,” Edith says. “I want to get her. I don’t care about Elvis Presley.”
Now Ada is pulling out box after box of loose stamps, stamps in plastic sleeves, stamps in presentation booklets, postcards, first-day covers only a few months old, mailed in Huntsville, Alabama, by one of two stamp services she subscribes to. “When she was in the hospital, I paid ’em off,” Edith said. “I said, ‘Don’t send me any more.’ But they’re still sending them.”
What hospital would let her play the piano whenever and however she wanted? What nursing home would give her an entire room for her dolls? What establishment of any kind would allow her to live with Edith, who no longer drives and would effectively be separated from Ada almost all the time? It’s impossible to imagine one without the other, their voices calling from room to room like birds. These restrictions are more profound than they may seem. Any action is an act of knitting, raveling the past with the present to create the future, making things that will exist, that will have consequences, that will still be there to be given away or shown off like dolls.
Think of the purposelessness of the hospital and the nursing home. Inaction, the stricture of a sterile environment, severs the connection through time and thus suspends life, as if death had soaked like a beetroot stain backwards through time and saturated the fabric of life still left. It’s not just a matter of having things to look forward to or even things to do with our hands to keep our minds off our infirmities, it’s that what we make today we can admire, or refinish, or give away, tomorrow. Today’s work is tomorrow’s surroundings. If what we did yesterday was meaningless, how does that help us when we wake up today? What does it leave us? The smallest acts create continuous discovery; even the Bermuda grass and the neighbor’s boy add their own variety.
Seeing Ada’s life unfolding, room by surprising room, I felt straightened up, as if someone had slapped me hard across my assumptions and left me blinking and alert. Whatever we, on the outside, think of someone else’s life is almost always wrong—and that becomes more and more true as a person approaches death. We make death, the unknowable, into the dark screen onto which we project our worst fears; and then we judge the experience of the dying accordingly. The patient’s weakening voice is easily drowned out by the hysterical clamor of our own selfish helplessness and horror, sometimes literally, like the Mexican woman I was told about who was in the ICU time and again and eventually told the physician that next time she didn’t want to be resuscitated, she wanted to be allowed to die in peace. But when her next cardiac episode struck, her family insisted she be rushed into the hospital, insisted she be revived; and because the first step of resuscitation involves intubation, the woman was silenced and died with a tube down her throat.
This is the heart of it all, the crux. Nobody asks, “What is the experience of the dying? What do they want?” And they themselves become steadily less and less able to tell us, until they reach the absolute truth and fall silent. If there’s one thing we can be certain about death, it’s that it’s not what we think it is.
Before we leave, Edith produces her masterpiece, a black doll in shades and a gold lame suit. “Do you know anything about rock and roll?’’ she asks. “A little," I say, buying time, thinking Stevie Wonder? No. Ray Charles? Surely not. “Hammer," she says. “I paid $19 for him. He’ll be worth a lot one day. His glasses come off.”
LIVING AND DYING
Is Ada dying? It’s an absurd question. She is living, clearly, if she is also dying, so are we all. The hospice philosophy tends to see things in terms of life or death, but not in terms of dying. It’s an existential approach. If I wake up tomorrow, I’ll make the most of what energy I have — a crucial mental shift from negative to positive. I was about to write “especially for cancer patients, who tend to have patches of energy alternating with patches of fatigue," but then I realized what I’ve realized time and again in studying hospice. We all go through patches of energy and tiredness, though for differing reasons and to differing degrees, and what hospice teaches us about caring for the terminally ill applies in every single respect to caring for ourselves, the healthy, who are also terminal, though we lack a prognosis.
Most of the time when we use the word “dying," we do so to convey a sense of urgency or perhaps self-pity, it’s not a condition but a drama.
I can think of two ways in which “dying” might have meaning: a hard, outer one and a soft, inner one, like the shell and the oyster. Hospice staff speak of a phase of “active dying,” which is markedly different from everything that has gone on before, even a day or so before. Quite suddenly, the patient’s biosystems begin to shut down. Breathing and pulse become shallower and erratic, blood pressure drops, secretions build up in the throat, which the patient no longer has the ability (or want? or need?) to clear, causing a rattling sound, the mouth falls slack, blinking slows, the facial muscles relax, making the patient Iook peaceful, younger.
On its own, this would simply be Sherwin Nuland biodata, the perceived changes reported in the official language without curiosity, but colloquially everyone will admit the mystery at the core. Nobody knows why these changes suddenly kick in. The principal truth about death, even on this moment-by-moment scale, is that nobody knows when it will happen. Hence the second meaning of “dying,” the open secret, immune to calibration, but seen time and time again: that we choose when to die or, in the hospice phrase, to let go.
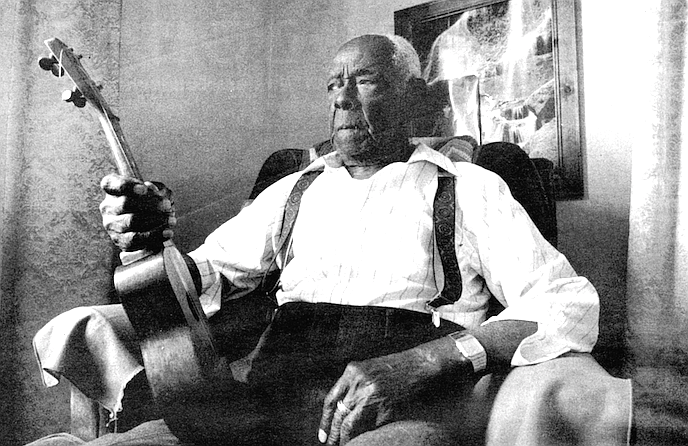
In many cases it’s hard to argue that someone has chosen to die, but perhaps that’s because they refused to let go and fought the changes in their bodies until their last breath. In other cases it seems perfectly transparent. “A new AIDS patient came in,” Kathy Ferdinandson said, “with herpetic lesions from head to toe, and I thought, ‘My God, how am I going to give this guy comfort?’ That was our immediate goal, and we also knew that his mother’s greatest grief would be for him to die in agony. We managed to get a morphine pump, we got some pain control, some wound care, we got him a different bed and mattress that wasn’t so painful to lie on, we taught the family how to turn him over so he didn’t scream with agony. Eventually one day he turned to his mother and said, ‘Mom, I’m comfortable. I’m ready to go now.’ And he died the next day.”
There’s perhaps one more meaning of “dying” that we use colloquially, meaning no longer engaged in living, living in body only, living without spirit. What do we give up when, in the name of staying alive, we agree to go to a hospital or nursing home? The conventional answer these days is “control,” and you’ll hear not only hospice staff but those in mainstream medicine starting to concede that the patient does better when he or she feels more in control. It’s more than that, though. If we leave hflme, we sever virtually all our connections with the normal processes of life that, no matter how apparently trivial, are vital. We opt for dying, of a kind.
LIKE GOD WANTS IT
The following day, something Ada had said still puzzled me: It’s just like God wants it. He can heal cancer as easily as he can heal anything else.
Was this faith or denial? She didn’t exactly seem to be in denial about her illness — I don’t think she meant “I’m going to get better” — but this raised the whole notion of an interventionist God, and prayer as a call for intervention, and disease as a sign of lack of faith.
To me, from my position as a wistful atheist, faith had always seemed to be something helpful and supportive, not only in life in general, but in giving the individual’s immune system (or spirit, depending on whom you’re asking) an extra boost in resisting infection or recovering from illness. Now it became clear that it could quite possibly be an additional burden.
I asked Geoff Copland, who is one of San Diego Hospice’s four chaplains, about this tricky theological issue. (Not every patient asks to see a hospice chaplain, but even so, spiritual support is regarded as one of the main thrusts of hospice care. For some patients, it may mean simply lending a sympathetic ear; for others, it may mean helping them discover sources of strength or coming to an understanding of both death and life; for others, it may involve an orthodox religious relationship. Virtually all hospice chaplains become adept at wearing a variety of hats or appearing to wear no hat at all.)
To some of the Pentecostal groups, Geoff said, a major illness would be a sign not of simple bad luck, overwork, or God testing one’s faith, but of the activity of Satan. What’s more, other members of the congregation might see the cancer as a sign of sin. He quoted me John 9, in which the disciples ask if the man blind from birth is being punished for the sins of his parents. Jesus doesn’t exactly help matters by saying no, he’s blind in order to show the glory of God, which He then demonstrates by curing him. This leaves the moral and spiritual status of other blind-since-birthers who didn’t happen to be cured by Jesus rather undecided.
In either case, this interpretation of disease-as-lack-of-faith would add to the impact of the illness, not help the patient deal with it (though it must be said that Ada and Edith seemed to be quite happy with their own faith), and leaves open not only the constant possibility of blaming the victim, especially, for example, AIDS patients. I shuddered.
The question hit close to home, Geoff said. His own son was born with bones missing in his arms and unusable thumbs; he has had a series of operations.
This dark question came up again when I went to visit a second hospice patient, Charles Bess, who has been a member of the Greater Apostolic Faith Temple Church for six decades, serving as deacon and Sunday school teacher. Armando was again acting as my guide.
“We’re going to Logan Heights. They don’t like white boys out there. That okay with you?” I assumed he was joking, but then I’m an easy mark. Vermont, where I live, is the whitest state in the union, and I’m an easy prey to racial fears. “We’re goin’ to Barrio Logan,” he told his team’s administrative assistant, winking. “Park close behind me,” he told me. With difficulty, I followed his BMW 733i down to the far end of Imperial Avenue, where he parked and fitted the steering wheel lock. “This is where I grew up.”
Charles Bess was sitting on a tubular aluminum lawn chair outside his house when we arrived, enjoying the warm January sun. He was wearing a ragg sweater, flecked with black, white, and gray, black pants, black socks, black loafers. He looked about 70. He is 97.
He took us into his neat little house, with its family photos, copies of let and Ebony on the marble-topped coffee table, next to a pamphlet from the Truth Apostolic Community Church. On the walls, plaques from his church thanked him and both his late wives for their leadership and service, and a remarkably touching painting depicted a bespectacled, middle-aged black man sitting by a front stoop reading to half a dozen small black children, who listened with rapt attention.
He came to San Diego in 1920 from Hawaii. He worked in Ocean Beach in an oil mill, raking oil seeds into a chute that loaded the freight cars, then moved to San Diego proper, and over the years worked as a janitor, in construction, as the “steam man” in a furniture plant, stoking the furnaces to keep the glue hot. In Hawaii he learned to play the guitar, the ukelele, the steel guitar, the piano, and his instrument of choice, the sax. But for an injury to his left thumb, he’d still be playing all of them, and he still liked to thump out tunes on the piano with his right hand. He married twice; both wives died, the second three and a half years ago. He had a son, three daughters, and “a whole heap of grandchildren.
“I feel healthy. I’ve been healthy all my life, so far. Just of late I’ve had this little heart congestion.”
He’s been on service for four months, at the recommendation of his doctor. “She didn’t tell me I had no congested heart failure. I just woke up in the middle of the night, 2:00 a.m., and I felt restless, and I didn’t know what to do. So I called my daughter, and she took me to the hospital, and they said I’d had heart failure in the middle of the night. Fluid was building up. They told me if I’d waited a little longer I’d have had a heart attack.... I noticed my legs begin to swell, so I’m taking water tablets — they keep you urinating pretty good. And I was beginning to wheeze a little. I thought I was getting a cold.”
“Why did the doctor recommend hospice?” I asked.
“I have no idea,” he said, surprised, as if this was the first time the question had occurred to him.
“So he can be independent, pain-free, and comfortable,” Armando chipped in. The nurse comes once a week to check him over, a homemaker comes once a week to clean and tidy, and Armando drops in when he’s in the neighborhood. “They’re very attentive. Nice people. I have no complaints,” Charles said.
As if to illustrate the hospice services, Colleen, a ten-year veteran hospice homemaker, arrives, makes herself busy, keeps out of the way. When I go to talk to her, she says she likes meeting different people, lets the hospice team know if someone seems to need a visit from the nurse, the social worker, the chaplain. She doesn’t seek the patients out for conversation, but sometimes they come over and talk to her while she works. She used to work for another housecleaning company; she likes working for hospice because they gave her a good training, likes being part of the team.
Charles Bess clearly had no plans to die in the immediate future. “I’ll shoot for a hundred. There’s no telling how long God will allow you to live. He has the last say.” (“Amen to that,” Armando added.) “He blesses you and keeps you and strengthens you, and you’re grateful for it. It don’t have nothing to do with anything you do for yourself. He’s the one who’s keeping you and encouraging you and strengthening you.”
I had no problem with that; so far, he was describing exactly the kind of spiritual, emotional, and physical sustenance that might not be measurable but is almost universally recognized in an anecdotal way. The clinical value of membership in any supportive community is now generally accepted, and Bess is a remarkably active member of the church community, going every Wednesday night, every Friday night, and then “pretty much all day Sunday.” He sits in on the Sunday school until about 10:30 a.m., though he no longer teaches, then attends “regular service” from 11:00 a.m. until 3:30 or 4:00 p.m., the church serves a full meal, “and then I’m back again from 7:00 until 10:00 or 10:30.”
Who could begrudge him his faith, the sustenance of his community? But my easy liberal tolerance is not reciprocated. “When you die in Christ, you can die with a smile on your face because you know you're going to die with Him.” He quotes Ephesians, “You have to have Christ in your life, and if you’re anchored in Christ you have no fear.” But if you don’t, he makes it clear to me, then you’re going to the pit.
But what about those who develop cancer at 70, or 50, I ask him. He looks at me hard. “The Bible says, Tf you believe in the word of God, it will make you whole,’ ” he said sternly. “Christ said that if we had faith the size of a mustard seed — and that’s a pretty small seed — it will help you move mountains.”
He didn’t go on to say that the weak are therefore weak in faith, but the implication was clear, especially as he went on to say that virtuous people who lack faith in Christ — my mother, for example — were unquestionably damned. I thought of the man blind since birth, the chaplain’s son — but by now he was asking me what my own faith was, and when I told him truthfully, if evasively, that I was baptized in the Church of England, this was clearly not a satisfactory answer. How was I baptized? In whose name? He was telling me forcefully, with the vigor of a man grown suddenly young and strong, about his own conversion during the depression, when he was rapidly becoming an unemployed musician, and about the people in his congregation who are filled with the Holy Ghost and speak an unintelligible language that is straight from Christ, when Armando finally got off the phone and we took our leave.
Hospice in the U.S. bears the unmistakable stamp of Elizabeth Kiibler-Ross — her medical humanism, her psychiatric observations of the stages of dying, her Swiss neutrality, and subsequently her religion-free curiosity about near-death experiences. As a movement, then, hospice has been in a cleft stick, promising spiritual support without ever seeming to be sure what spiritual support actually was. The National Hospice Organization had been in existence for ten full years before it convened a conference to discuss spirituality in hospice care, and it has still come to no kind of consensus. If hospice has a bible, it is the Tibetan Book of the Dead. Nothing I’ve ever heard at hospice conferences or read in hospice books says anything about what to do if your patient, his family, and his community believe that cancer is sent by Satan.
What was suddenly becoming stunningly clear to me was that in National City or Chula Vista or El Cajon or Logan Heights, this graceful new-age ecumenical dance was simply not going to cut it. Talk about preparing for death — all the time modern medicine
was going further and further in encouraging us to follow our natural disposition to avoid thinking about death, older and more authoritative forces had never abandoned the subject, had never let up. It had been perfectly clear to them for 100 years, or 200, or 2000, how to die with a smile on one’s face, and they didn’t need hospice chaplains or social workers, and some of them didn’t even need doctors to tell them what life and death were all about. And in a weird way, that’s fair enough, because if medicine and science want to focus only on treating the living, and the dying are in God’s hands, then who can blame us, especially those of us who have the foresight to consider our mortal ends ahead of time, for turning away from medicine and science and seeking the strange and powerful disciplines that are enacted in God’s name?
San Diego Hospice seems to be defying the national demographics, which suggest that hospice is used predominantly by the white, educated middle class, who are likely to have some spiritual convictions but not to be overpoweringly religious. It suddenly strikes me that the reason why it diverges from these trends, and the reason why I’m so uncomfortable under Charles Bess’s interrogation, is because it is successful. SDH has set out to serve the community, that conveniently undefined body of Americans so bekived in theory by liberals, and has produced, in President Clinton’s words, a patient body that looks like America. What happens when the patient doesn’t want your spiritual ecumenism? What happens when that very liberality makes you, in his eyes, eternally damned? You go in and dust the pictures. Launder the tablecloth. Vacuum the rug.
When I stopped at the light outside Bruno’s Market, just down the block, mine was the only Anglo face in sight.
A CONVERSION EXPERIENCE
One of the oddest features of hospice is that, far from being a depressing or morbid occupation staffed exclusively by saints or people of extraordinarily tough backbone, it seems to give back even more than it demands. Virtually everyone in hospice looks five to ten years younger than they really are, and it suffers an amazingly low burnout rate among volunteers, who work at the emotional coal-face as much as any paid staffers. This is perhaps the crux of the matter; by being such a vivid and potent experience, death forces us into emotional states we usually avoid. These states, like all crises, offer as much opportunity as threat. We can recoil from them, we can close down, we can shove others away from us — all these are common responses to death. We can also, often for the first time, accept help, admit weakness, recognize generosity and gratitude. This is a stunning transformation; it’s like a glimpse of an entirely new dimension. It not only helps us to accept death, it changes our whole view of life.
Kathy Ferdinandson worked for nine years in emergency room medicine before changing to hospice, where she has now worked for two. The day she decided to quit ER work came at a time when she had begun working for San Diego Hospice but was still working on a per diem basis at the Alvarado Hospital emergency room. One Friday she worked all day at the hospice, then went over to Alvarado to work the night shift. It was a very busy night. At one point, she was due to take the next ambulance run. When the ambulance came in, it was delivering an SDH patient.
“At the last moment, the family had freaked out and told the EMTs to go to the ER rather than the acute-care center" at the hospice, she says. “This was, in my feeling, divine intervention.” The patient was comatose, actively dying. “In the next bed a drunk was swearing obscenities, in another bed a baby with an earache was screaming bloody murder, bells were ringing, beepers were going off — it was crazy.” The family was distraught with grief and guilt, crying, “Why did we do this?” The ER doctor ordered x-rays, 02, lab work, even though the family had asked for their mother not to be resuscitated. Kathy took the doctor aside and told him, “Look. This is a hospice patient. The family has asked that she not be resuscitated. Please, please let me take her upstairs where we can find somewhere quiet for her to die in peace.”
The doctor agreed and signed the order. Kathy went back to the family. “Your mother is dying,” she told them. “I’m going to bring her upstairs. Please go with her. Talk to her. She can hear you.” When a room was found for her upstairs, the family gathered around her and prayed. The other nurses took over Kathy’s patient load — glad, she believes, that she had relieved them of such an emotionally difficult and volatile encounter.
Kathy barely had time to go downstairs to thank her colleagues for relieving her, when another nurse found her and told her that the mother had died. She rejoined the family, who sang the mother’s favorite songs and prayed. “It was the next best thing to being in the acute-care center [at the hospiceJ or at home. They thanked me over and over.
“When I came back downstairs, and I must have been with the family for nearly three hours from the moment when they came in, I knew that I was no longer focused on patch-’em-up, move-’em-out, we-need-this-bed. (A hospital staff] may think they’re treating a patient holistically, but they don’t. They talk about people as ‘the ankle in three, the broken arm in five, the earache in four.’ I can’t be that kind of nurse anymore.”
Her first hospice patient was Joe Wehlage. Joe and Mary Wehlage and their children moved to San Diego in 1948; Joe was in the Navy and had been assigned to train recruits. He finished his 20 years in the Navy in 1957, went to work for San Diego Gas and Electric for 23 years, and retired in 1980. In the fall of 1992, Joe, then in his mid-70s, began feeling back pains and protracted fatigue. Over the next few months his shoulder began hurting too. A rheumatologist, who apparently failed to take x-rays, dismissed the pain as bursitis, but by the following March, when Joe found blood in his urine, a bone scan revealed his entire skeletal system was cancerous. “There were hot spots throughout, and the whole shoulder area was deteriorated to the point where bone was just missing,” Mary said. (The rest of this narrative is her own.) “What was there was porous, just gone. His whole skeletal system was involved, and obviously some of the major organs, though at that time we weren’t told that. When the diagnosis finally came, it was, ‘This is terminal, and you probably have maybe three to six months to live.’
“Our primary-care doctor called. He waited till the end of his office hours, so he could really talk. I have nothing but the highest regard and affection for this man. He felt so badly about it, to have to tell us, and he said, ‘No wonder Joe doesn’t feel well — bone pain is just about the worst kind of pain there is, and when his whole body is affected, there is not a spot that is going to be pain-free.’ He said, ‘You had better get ahold of hospice, because you are really going to need them.’ I had heard the word — I knew they had a new building up there — but I didn’t really know anything at all about hospice. “We were terrified, just terrified. I mean, we hadn’t ever thought...you don’t think...you feel, you know, that someday one of you will die before the other, but to say, ‘Okay, this is it.’ Then you wonder if the doctor said six months to give you hope, but really meant three months. The impossible thing to take in was that by the end of the year, Joe was not going to be there.
“By that time the doctor put him on morphine medicines, which immediately affected his mental processes. One time when I had given him the medicine, he was sitting on the edge of his bed. He had a digital clock that would Hash, and he was sitting there just mesmerized by that clock and watching those numbers flash and rambling on about the stock market and train schedules. I was terrified all over again, because I couldn’t get through to him. He was just gone from me. He did have some lucid time after that — not a lot, but some where we could really sit down and talk and discuss things in the past and settle affairs that needed to be settled then.”
“Settling one’s affairs” is virtually a cliche, but it goes right to the heart of the distinction that hospice draws between pain and suffering. For many hospice patients, the physical pain is not their most pressing concern; they may be far more concerned about the personal matters that they won’t be able to take care of. Who will handle the family finances? Who will look after the kids? Anything that has emotional value — the dog, the guilty secret, the unspoken love, the unconfessed crime, even the unweeded garden — involves a departure that may gnaw at the dying person more persistently and painfully than any disease.
“Joe had always handled the money. I was so afraid of making a mistake that I about wore out the calculator the first couple of months, checking and rechecking every little detail and making sure that I hadn’t forgotten to pay any of the bills. Joe had a lot of credit cards and agreed now that they had better be canceled. By this time he was having trouble using the touch-tone phone, so we decided that I’d make the necessary calls. In this one instance — Citibank, I think — there was an 800 number to call, so I called it and said we don’t want to renew the card. ‘Who’s speaking?’ ‘It’s Mrs. Wehlage speaking.’ ‘Well, the account’s not in your name.’ ‘Yeah, I’m aware of that, but my husband is terminally ill, and we want to close this account.’ They said, ‘Well, you can’t do it, he will have to do it.’
“By that time he couldn’t manage the phone or balance the checkbook — there was something mentally deteriorating. For someone who had been so good at all that type of thing to not be able to really do it anymore was so frustrating and embarrassing. So I got the number for him, and I got whoever they said he had to speak to. By now his hearing wasn’t so good, and he didn’t understand what they had said, and he asked them to repeat it. Apparently whoever was on the other end was really rude, because Joe lost his temper, which was unusual for him in a situation like that. They wanted to know his mother’s maiden name. I knew his mother’s maiden name. I could have given them the information that they needed to close the account.”
Mary’s nephew called San Diego Hospice, and after an initial assessment, Kathy Ferdinandson went out to the Wehlages’ house.
“She just epitomizes what hospice is all about,” Mary said. “She was interested in Joe and both of us as individuals and as a couple. She was extremely sorry that she had to meet us under these circumstances, but that was her job. I was, like, ‘This is too good to be true.’ But as time went on.... Her immediate priority was to get Joe pain-free so that whatever time was left could be quality time. And she tried valiantly with ever-increasing doses of medication and changes of medication. She was in constant touch with our doctor downtown. She was supposed to come twice a week, but all I had to do was call, and she would come and stay as long as we needed her. I just can’t say enough about Kathy.
“One day Kathy said to me, ‘Are you eating?’ I thought, ‘Oh.’ She said, ‘Sit down here. Get a Coke. Now tell me what you’ve had to eat today.’ ‘Well, not much.’ She said, ‘You have to take care of yourself, because if you don’t, you’re not going to be able to take care of Joe.’ She’s young enough to be my daughter, but she would sort of reverse the roles and be like my big sister. She is a lot taller and bigger. When Kathy hugged me, I said, ‘I just was hugged by a grizzly bear.’ ”
In June one of Joe’s deteriorating shoulder bones broke with an audible snap as he was getting up from his wheelchair. “From then on, he didn’t believe any talk about the possibility of quality time. He expected that more bones would break and that all he could look forward to was worse and worse pain. He went into an emotional tailspin. Kathy was so concerned about him that she insisted I remove all of the medication from the dresser in his room, because she was afraid that he’d overdose himself out of desperation.
“She said, ‘You go on out in the kitchen or the living room or something, because Joe and I are going to talk.’ And what they did was just have a knockdown battle back there. But she had forgotten that I had a nursery monitor that I kept out here so that I could hear everything in case he needed me or wanted anything. I couldn’t really distinguish the words, but I could hear there was all this awful commotion going on. I think he gave up at that time. It just wasn’t a battle worth fighting. Which I guess it wasn’t. But Kathy tried, she tried and tried and tried to get on top of the pain, but we never did actually totally get on top of the pain, and his condition physically as well as emotionally and mentally just deteriorated steadily after that.
“Kathy kept saying,‘‘You cannot do this by yourself.’ I said, ‘I am not going to have a stranger in this house.’ She said, ‘Well, you cannot do it by yourself.’ But then someplace along in there, my sister and brother-in-law just came and moved in with us; and my brother-in-law helped me with the nursing, and my sister just took over the cooking and the housework. I was so fortunate that they would just drop their own lives and stay with us for two months. Joe’s situation really brought our family together and strengthened and established on new levels the bonds between all of us.
“I felt totally supported — by my family members, by the whole hospice organization — whereas if we had been dealing still with the doctor and in a hospital situation. I’d have been shut out, I couldn’t have been there all of the time. I was just grateful that we could keep him home for mostly all of the time.”
Joe died on July 21. “At the end, even the morphine pump just didn’t do it. His pain was worse and worse and worse, and I thought, 'This is it. Just order an ambulance and get him up to the acute-care center, please,’ which they did. It took probably 8 to 10 hours to really get him comfortable there. But for those last 24 hours of his life, at least, he was totally comfortable. My daughter and I stayed right there in the room with him, so we know that he was peaceful and comfortable when he died, and the people who loved him were there with him. When he died, he suddenly looked at least 10 years younger, maybe 20 years younger. My last recollection of him is that he looked young and happy and peaceful and contented and pain-free.”
SDH helped Mary arrange the cremation and burial — Joe’s ashes were scattered at sea by the Navy —and the host of other infuriating and time-consuming administrative details that accompany a death. After the funeral, Mary began, rather unwillingly, to attend the support group meetings twice a month in the home-care building with 10 to 20 other survivors. “I wasn’t going to go, because I had been a very private person, and I thought you just don’t go doing your crying and reminiscing and whatnot with a bunch of strangers. But Kathy encouraged me to go, and my sister insisted that we go. She said she would go with me.
“The first few times I don’t think I had very much to say, but I was glad afterwards that I had gone. You can feel the support all around you, and you don’t have to speak if you don’t want to. I never took my dark glasses off for the first several weeks. I wasn’t aware of that until later when Patty Clement remarked that it was the first time she’d seen my eyes. I have not missed a bereavement group meeting since I first went in August of 1993, and now I am a volunteer in the bereavement department.
“Kathy had asked me if I had given any thought to what I was going to do afterwards. I thought she meant what we were going to do about services and so on, but I think, looking back, she meant, ‘What was I going to do afterwards, as time went on?’ From the first time I ever met her, I knew that eventually I wanted to be a hospice volunteer.”
Like most hospices, SDH won’t allow anyone to become a volunteer until at least a year after a bereavement. The likelihood of mistaking one’s own grief for someone else’s is simply too strong. After waiting her year and undergoing training with Judy Davis and Patti Clement, Mary made her first support visit in January.
“I went to see a lady whose husband had died in November. She doesn’t really want to come to the group meetings and feels alone — which she is, so she’s entitled to feel alone. She’s a military widow, so we had that to talk about. She has three adult children, and so do I; plus, we both have cats. The rapport was there. It was great. I had been very apprehensive, because she was my first contact. What if I said all the wrong things and just tore this lady apart? But I feel much more confident now. Patty said, ‘Trust your intuitions. Just keep your mouth shut and trust your intuitions.’ ”
Hospice has taught her how to grieve and how to begin to remake her life.
“The medical attitudes [in the hospice] are just unbelievable. Everybody cares so much, and you can just feel there is an aura of love and caring in the whole establishment. I love to go up there and just stay and wander around on the grounds and sit and look at the view or whatever. To me it’s a healing place to be.” Every morning she walks down by Mission Bay, where on Saturdays she often sees the hospice group. “I cherish my time down there by myself. There are no phones. I like it when I meet somebody to visit with for a few minutes, but if I just want to look at the bay, and the birds, and the trees and think my own thoughts, that’s fine.”
RECRUITING THE FAMILY
Armando emerges from one of the rooms in the acute-care building, where one of his patients is actively dying. The building is quiet and full of light; outside the windows, leaves dance in the slight breeze. The dying man is calm, he tells me.
“ ‘Brother Joe, it looks like this is okay,’ I said to him. ‘It looks like you’re peaceful.’ And he nodded, like this. Physically he is diminishing, he is dying. However, beyond that, there is a peace, both of acceptance and of resignation.” (Resignation, I think, is not a quality much encouraged in young Americans, especially men.) “I sense no anguish from him,” Armando continues, “and therefore he evokes no anguish in me.”
Social workers are a crucial part of the geometry of hospice care, which instead of being hierarchical (doctor at the pinnacle, nurse somewhere beneath, patient on the bottom, patient’s family largely of nuisance value) is strikingly egalitarian. A terminally ill patient needs frequent, perhaps even constant care, though not all of it is care that needs professionally certified clinical skills. Meanwhile, the closure of a life is a time that cries out for reconciliation and summation. Nobody wants to die alone or with unfinished business. (The bitterest cry of Hamlet’s father’s ghost is that he was “cut off even in the blossoms of my sin, / Unhous’led, disappointed, unanel’d, / No reck’ning made, but sent to my account / With all my imperfections on my head.”) For both practical and personal purposes, then, it makes sense to draw the family together as a rapidly trained home health team, and this connecting of the points is the social worker’s job — a job that is often very difficult.
“If it’s a — let’s not say a pathological family, but a troubled family, then death will stir the pot,” Armando explains. “A lot of unresolved issues — whoosh!— will come up from 20 years back, 30 years back, 40 years back. They’ll come up, they’ll become very vivid, and both the dying and the living realize that something is ending, and it’s either going to end right, with peace, or it’s going to be unresolved, with anguish.”
Recruiting the family as caregivers brings up an entire history. The whole family tree is suddenly laid out between them like an embroidered tablecloth. Some may refuse to help out of ancient I’ll-never-forgive-you-for-what-you-said-to-Mom resentments; some, more obliquely, may simply be terrified of death. The wife of one of Armando’s patients refused her husband Paul’s wish to die in his own bed, because her own grandmother had died at home in the days before palliative care, and it had been a painful and troubling death. Three days before he died, she suddenly changed her mind. “You got me thinking about what Paul wants,” she told Armando. “I held her and said. Thank you. You’ve made everybody very happy.’ And she said, ‘I know.’ ”
One of Joe’s sons is in jail, but his wife, daughter, and other son are with him — quite an achievement, as his successful microbiologist son grew up bearing a bitter grudge against his father for spanking him long and hard for shooting ball bearings with a slingshot at a movie screen.
“His father was a good provider, a good teacher, a good companion in a lot of other ways," Armando explained, “but the son wouldn’t see that. So I took this strapping man and this fragile, now-diseased father, and I said to the father, ‘Would it be too much to ask Robert to forgive you? I know that he’s a man now, he’s grown bigger than both of us, but that little child in him is still injured and thinks that your insensitivity caused that great pain.’ And he did. The father said, ‘Can you forgive me, son, for causing you that pain?’ and the son choked up, and he just hugged him. It was beautiful. There were a lot of tears.”
In effecting such a reconciliation, hospice is changing the meaning of death and establishing a new family legacy concerning how to handle the frail and the dying. Perhaps the next generation won’t be so scared of death; perhaps they’ll see it as a time of opportunity, even, to heal old wounds. Many of the benefits of what we do, an English hospice physician told me, won’t be seen for another 20 years or more.
The four hardest deaths Armando’s seen were all of men who were very intelligent but very contentious and who refused to accept that they were dying. We often praise such people as “fighters,” but in refusing to accept death they also refuse to accept that “they can go hard or they can go peacefully” — that is, they can help create the circumstances and the experience of their own dying. While hospice can’t guarantee every patient a painless and peaceful last few weeks or months, refusing to admit the approach of death does little but harm.
Armando’s beat is the South Bay, and he seems to be the right person for the job, having grown up in the racial and cultural mix of Barrio Logan, in those straitened circumstances, that social fringe. He describes himself proudly as bilingual and bicultural. He’s worked with gangs, geriatrics, and mental patients; currently at SDH he has a caseload of 25,24 after Brother Joe leaves.
Many of his most delicate cases involve cultures — Hispanic, Asian — in which it is absolutely taboo to discuss death or even serious illness, especially with the patient. “They want [hospice’s) help — they want the nursing, they want the visits, they want the expertise — but they don’t want to be upfront with the patient. I’ve broken some barriers. I’ve taken the head of the household aside, and I’ve said, ‘Let’s say it was you.’ ‘Well, that would be different.’ 'What makes you say that?’ I make them think, at the very least.” How he approaches them depends on the degree of acculturation and assimilation. “If, for example, I see it’s a third-generation Mexican-American family I’d approach the topic of death and dying and disease a lot more freely than if they were one generation removed.
“I haven’t found any group I couldn’t work with, so far — Hmong, Vietnamese, Indians, Cambodians, African-Americans, all kinds of Latinos — Nicaraguetises, Colombianos, but that’s easier than Indochinese, because the language is the same and the cultures are similar. I think that if you come in with respect, they’ll pick it up. No matter how much they lack sophistication or education, they’ll still pick up your intentions.”
Dr. Mary Margaret Loehr echoed this difficulty. One of her hospice patients was from Thailand and spoke no English, and she had no idea whether to tell him about his condition or even if he understood anything anyone had told him. She asked Phong, a young hospice nurse originally from Cambodia, to act as translator, but that, too, created more layers of difficulty. She was younger than the patient, she was female — to admit vulnerability to her might have been an act of great shame for him. Finally Loehr told Phong, the nurse, “Ask him why he thinks he’s here.” The question was translated, the man looked Phong right in the eyes and said, in Thai, “I’m here because I have terminal cancer.” From then on, everything was much easier.
ANOTHER WELL-SPENT GRANT
There’s a story, possibly apocryphal, that the National Cancer Institute conducted a study to find out what would happen if people didn’t die of cancer, and they found out that...they would die of something else.
MED ED TWO
In one of the conference rooms in the acute-care center, Judy Davis, Director of Bereavement Services, was getting ready for the day’s small batch of medical students by scattering on the table stones of all shapes and colors, shards of sheepskin, model cars, shells, dolls, and weathered pieces of wood. As the students drifted in, she asked us to pick up one or two of the items that took our fancy. I took a brilliant-purple polished stone and a racing car in the shape of a shark; two of the students fought over a tiny plastic Tyrannosaurus rex.
In her two hours, Judy was trying to achieve at least three things; to outline the hospice’s bereavement support services, the most extensive I’ve ever come across; to show these doctors-to-be how to communicate with patients sympathetically and respectfully, and to get them to think just a little about how they think about death.
Traditionally, doctors think about death as little as possible and talk about it even less. Until the last decade or two, the vast majority of physicians avoided telling their patients when the diagnosis is terminal, arguing that the bad news will send the poor soul into a fast downward spiral. (As recently as 1972, 60 of 73 doctors in a private Detroit hospital refused to discuss their attitudes toward death and dying. And while all the remaining 13 agreed that a patient should be told if his illness is terminal, only 2 had ever actually done so. The task was either too difficult for them or they saw it as simply not their job.) This apparent concern for the patient’s spirits was more than somewhat undercut by the fact that instead of making up for the lack of information by kindness and support, the average doctor in fact chose this moment to vanish altogether, leaving the patient feeling not only sick and confused but abandoned.
Studies of nurses, meanwhile, showed that when patients said things like, “Am I dying?” eight out of ten nurses avoided any discussion of the patient’s thoughts or feelings — which again might show a commendable concern, but for the fact that other studies showed that when a terminally ill patient called or rang for a nurse, it took him or her almost twice as long to respond than to someone who was less ill.
My father’s death from cancer in 1979 was typical of this set of attitudes and beliefs. When he first became ill, he was seen by a steadily rising hierarchy of physicians until he reached the consultant, the “top man,” who was invariably cheerful and optimistic, refusing to discuss any possibility that the disease might not be curable. As radiation and chemotherapy treatments went on and their benefit became more and more temporary, the top man appeared less and less often, and my father slid back down the medical hierarchy. He was moved out of the prestigious urban hospital, because he was an embarrassment, a piece of bad publicity, at no point did anyone tell him that his cancer was looking incurable.
After 18 months, they finally took him off all treatments except morphine, and when his mind cleared, he asked, “Well, what’s the plan now?” The attending physician to whose level my father had now fallen was a young Indian doctor who took my mother out of the room and burst into tears. “I can’t tell him,” he said. So my mother went back in and told my father that they were letting his system clear itself out and then they were going to try something else. When he died a few days later, he was intermittently crazy. Knowing intuitively that he was dying, but never having been told, he put the two facts together and concluded that the hospital staff was secretly trying to kill him. When my brother visited him on what would be his last day, my father handed him a pair of scissors from the nightstand. “Take these,” my father said, “'they’ll try and get you on the stairs.”
The medical students drifted in. There were five of them, all in their third year, three men, two women. Some were in white coats, and one sported stethoscope and patella hammer. He and one of the women had just come from their surgery rotation. Most said they didn’t yet know what they’ll specialize in; one of the women, she who had just finished her surgery rotation, announced crisply that she intended to be a cardiothoracic surgeon. None had lost a close family member or friend.
This was their second half-day in the hospice. They had already seen the videotape of physicians with cancer, though it was hard to tell how much they had yet grasped. None could sum up the hospice philosophy. One or two yawns were smothered, though it was, after all, 8:15 a.m.
First she told us about the bereavement work at San Diego Hospice. Bereavement support is crucial because grief is so poorly understood. Survivors know what you’re going through. Neighbors may say, “Oh, aren’t you over that yet? It’s been a month, now.” Grief is like carbon monoxide, invisible, undetectable, often you don’t even know it’s there until something triggers you and you forget the rest of your sentence or drive into a wall.
The bereavement team, she said, calls family members at 2, 6, and 12 months after the death, more often if tipped off by a nurse, chaplain, or social worker that someone or a family is not doing well. Many people just need to talk to someone who has been there too. Like most major upheavals, death engenders experiences for survivors that other people just don’t seem to understand. We seem to acquire a new emotional vocabulary other people just don’t seem to have. SDH holds support groups during the day and in the evenings, involving children as young as three years old, who, far from being too young to be included, may be most at risk because they have so little life experience that it’s hard for them to put death in context.
Every Saturday a volunteer couple leads a walkabout for survivors, starting down by Mission Bay. This has developed into something of a social group, and some of them go on to brunch together afterwards and put on potluck suppers every so often. The hospice itself sets up potlucks too. The bereavement team also sends out a newsletter every month for 18 months, each issue designed to address the difficulties the bereaved may be facing at this point. Judy called it “a programmed learning about grief and loss.” Bereavement outreach volunteers visit those who can’t or don’t want to visit the hospice. Every family is sent a package of recommended readings, too — the whole family, not just the primary caregiver, the visible one. All these services are open not only to SDH families, but the community at large, especially to those who have lost a relative elsewhere in the country.
SDH is also called into the schools, especially by peer counselors who feel unequipped to discuss the deaths that affect students — car crashes, drug overdoses, gang shootings. Judy went through an exercise in which she stacked up a child’s blocks as if each were a stage in one’s life, then sent them crashing to the table top. This is what grief does to you. Life afterwards is a process of rebuilding, though one of the pieces is now missing.
She now handed each of us a dozen small, square pieces of scrap paper. Idly, I turned mine over. They seemed to be surplus copies of a promotional flier, five-by-five inches, on glossy, coated stock, that told the story of Glenn Wells, 82, who came into the hospice’s acute-care center with colon and liver cancer, in acute pain, and near death. Ten days later, the flier said, he went home free of pain and other symptoms, attended his grandson’s high school graduation, and resumed playing golf.
I’m of two minds about the flier. It reminds me too much of the slick, triumphant TV ads for the for-profit cancer hospitals. It’s careful not to say that Wells is “cured,” but it’s equally careful to avoid any mention of his long-term outcome or of death in general. True, hospice has to work hard to overcome a you-go-in-there-and-never-come-out-alive stigma, and in fact a good number of patients visit the acute-care center of any hospice for a short tune-up and then return home. All the same, such a “star patient” promotion seems slippery, quite at odds with the rooted, positive pragmatism of hospice in general.
On three of the squares of scrap paper, she said, we should write the names of three people who were our nearest and dearest. On another three we should write our three favorite possessions, on another three our favorite activities, and on the final three the qualities we like most about ourselves. (This in itself was quite a challenge.) Lay them on the table in front of you, she said, and follow the instructions I give you. She began to read from a sheet of paper.
“Picture yourself at your doctor’s office. It’s the middle of October and one of those perfectly wonderful fall days. There’s a nice breeze with a touch of coolness in it, but the sun feels warm on your skin. You see your doctor smile at you when he says hello, but the smile doesn’t reach his eyes. He looks tired to you, and suddenly you feel nervous. You hear him say that the test results are all in, and he is so sorry to tell you that the news is very bad.
“I am the virus. I am the virus that we call HIV, and I have supreme power. I can take things away, anything that I care to. Because I am so powerful and because I have complete power over you, you must do what I say. I now want you to let go of three things that you value. And let them go by throwing them into the middle of the circle now.
“You have just lost three things that you value. You are angry, resentful. Because I act slowly at times, you have an opportunity to regroup and adjust, time to take stock in what is left. And then suddenly I’m back; and because I am all-powerful, I demand that you let go of one more thing that you value. You must tear it up and throw it away.”
Now she had our attention. Except for her voice and the intermittent sound of tearing paper each time the disease progressed, the room was utterly silent. In her narrative, the months passed and the disease demanded more of the things we held most dear; in our imaginations, we were pretty shaken.
“I want you to take a look at the last two things in your hand, examine them, prioritize them, and now I, HIV, want you to let go of one more item that you hold dear. Because I am supreme, you must let go of it now.
“You are left with one very precious thing. And finally I return, and I want one more item from you. Look at the one thing in your hands and let go. You must do this. Tear it up. Now you are dead.”
After a stunned silence we talked the exercise over, agreeing that possessions mattered least and people most, discovering that the exercise had reopened some grief or loss in everyone’s life and made it available to them as something to learn from.
And what might they learn from it? Judy’s summing up showed how potent and long-lasting good and bad clinical communication can be, affecting one’s whole perception of a death, even of death itself. When her son died, she told us, in a hospital, the doctor didn’t come out and tell her himself. “I understand,” she said, “but I’ll never forgive him.” Instead, he sent a nurse. The nurse did something that, Judy said, she may forgive, but she will never forget. She smiled, perhaps out of nervousness. It was not a moment for smiling. She also came a little too close and in doing so left a strong whiff of perfume — and 20 years later, Judy realized that this was why she had hated perfumes all her adult life and had refused to use them.
Twenty years later, her father died. The doctor came out and told her himself, quietly and directly, “Your father’s died.” Not too distant, not too close, he asked, “What can I do to help?”
“Can I see him?” Judy asked.
“Of course,” the doctor said. “Would you like me to come with you?”
She asked him to go in with her, and after a few minutes she asked him to leave so she could be alone. He had done his job and had done it right.
“The work that you do with the dying and their relatives will last a lifetime,” she told the students, quietly but forcefully. “Do it well. And if you can’t, don’t do it.”
A THEATRICAL DETACHMENT
At this point, this article is going to seem to go seriously astray, so I might as well come clean. My aim is not simply to write about hospice, though that in itself is a worthwhile aim, as hospice is poorly understood even by the mainstream medical community. My aim is to make you less afraid of death, and examining hospice is one way to do this.
The odd fact is that the death we (will) experience is probably very, very different from what we think it will be, based on deaths we (may) have observed, especially deaths we’ve seen on television or in the movies. The best illustration of the difference between the death observed and the death experienced is in trauma—that is, major bodily injury of the kind to which we normally respond in shock and horror. When we talk about “horrible” and “ghastly” wounds, we’re actually describing our own reaction. The worse the injury, in fact, the less likely it is to involve pain and suffering — at the time, at least. The pain and suffering are actually part of the healing process.
Few injuries seem more terrifying than falling from a great height, for instance, yet in Choices in Healing, Michael Lemer points out that studies of Alpine climbers who have survived falls reveals that, as usual, popular culture has got it all wrong.
“As the fall begins, the climber does not scream as falling people do in the movies. Instead, time slows down enormously — as it does for many people just before a car accident. Everything seems to be taking place in slow motion. The [theoretical] survival benefit of this slowing down of time is that the falling climber has every opportunity to notice lifesaving possibilities — handholds or shrubs that might be grasped to break the fall. But if the opportunities for active self-preservation disappear, the faller then enters a state not of panic but of deep peace. He may experience the often-reported process of life recall, with his life flashing back before his eyes. He may hear celestial music. Hitting the ground is usually experienced without pain — he only hears the impact. Hearing is the last sense to disappear into unconsciousness.”
The same holds true in the more prosaic setting of the urban emergency room. “Some of the spiritually most peaceful deaths I’ve seen — that is, the calmest, the ones with least anguish, are in people who have been horribly injured,” said Dr. Mary Margaret Loehr. “Most people are very surprised, and kind of detached.” A man was admitted to the Scripps ER with a shotgun blast in the abdomen, still conscious, with “almost a theatrical detachment.” He was alert and functioning well enough to be able to tell them his own name but also to be able to refuse to name his own wife as the person who had shot him.
The greatest psychic anguish seems to be in those who are fighting to breathe and in general still feel they have some control over their condition. It’s when we lose or give up that control that we find the calm and detachment. “When people come in with severe heart attacks in great anxiety, we medicate them, but I’m often surprised by the degree of peace and calm that then come over them. It’s not just medicine.”
It’s almost a rule of thumb: the grimmer a person looks, the less he is suffering — unless he recovers, that is. Former San Diego police officer Donovan Jacobs walks a little stiffly, his left arm hanging at his side. He has scar tissue running down the left side of his throat and a deep dimple in the back of his neck where a bullet was dug out, and a long scar running a foot down from his navel where the surgeons went in to repair internal injuries. He doesn’t look like a cripple; he has the look of a man who has been battered but is still plunging on.
Jacobs, now a lawyer, is careful to explain that it’s very hard for him, especially after several weeks of painkillers and at ten years’ remove, to be certain what he experienced at the time or, perhaps more importantly, what he did not experience. He might have had the same curious lack of fear or pain that the climbers reported, or he may simply have lost those memories under the influence of morphine, Demerol, and Percodan and who knows what psychological defense mechanisms.
Ten years ago he was in his patrol car with his partner and a young woman observer, a “ride-along.” They pulled over a pickup truck driven by Sagon Penn. A fight developed, during which Penn managed to grab Donovan’s gun. He shot Donovan in the neck, then shot Donovan’s partner, killing him, shot the woman in the car, then drove the car over Donovan as he lay on the ground. Donovan probably came as close to dying as humanly possible. He lost 17 pints of blood, had both his shoulders dislocated and half a dozen ribs broken, suffered numerous internal injuries from being crushed by the cruiser, whose catalytic converter also inflicted third-degree burns on his arm. The bullet passed through the brachial plexus area of his neck, which is a major nerve junction, damaging a number of nerves including those to his left arm. Despite these massive injuries, he remembers only one brief moment of pain. His memories come in glimpses; the ellipses represent the blank spots between these glimpses.
“I stopped him...I asked for his license. He tried to hand me his wallet. When I told him that wouldn’t do, he turned and started to walk away from me...I may have grabbed his shoulder...I was hitting him in the back with my baton as he was fighting with my partner...he turned on me...we went to the ground...I was on top of him, wrestling with him, trying to get him turned over so I could handcuff him...we were surrounded by a crowd of about 30 non-hospitable people who seemed to be about a foot away, and I thought I was going to get my face kicked in by them...the next thing I remember. I’m shot and on the ground, thinking I had to get up and fight back...I think I remember hearing people scream...I realized he was driving the car toward me and wanted to run ifie over...I saw the undercarriage of the car as it passed over me, and I thought, 'God damn, this hurts’...lying there expecting the cavalry to be there...the paramedics were there putting me into a mast suit, which is a set of pressurized pants that push the blood from your lower body toward your upper extremities. I knew that had meant I’d lost a lot of blood, because I used to be an ambulance driver for the police...I was in a helicopter on a stretcher, looking up, thinking, 'They don’t give you much headroom on these things.’ I don’t know what I was seeing, but it was right above me, a few inches in front of my face. I guess they shelve you into something...I knew that Tom had been hurt, and I remember asking about him, and when they didn’t give me a response, I knew that was bad.”
He doesn’t remember anything of his first three or four days in intensive care, then he has vague memories of visits from friends and family. Continuous memories start from when he had been in the ICU for three weeks. By then he knew he was in pain, though the painkillers kept at bay both the physical sensation and the emotional impact of what had happened.
“I don’t remember ever entertaining thoughts that I was dying. I don’t remember feeling any pain at any point except when the police car ran over me.”
Trauma illustrates most clearly that we tend to talk about death the way we experience it as outsiders, onlookers. This not only affects our own attitude toward the death we expect to have (and may strenuously resist thinking about) but also affects the way we treat others who are dying. In a sense, if we have foolish attitudes about our own death, that’s our own business, but others who are dying are very, very vulnerable. It’s extremely easy to override their wishes and needs and to do so out of our own prejudices. The mother who wanted to die in peace but couldn’t say so because of the tube down her throat is only the most extreme example. Death is a process of individuation, hard though that may be for us, the living, to accept.
Perhaps the greatest and most enduring value of hospice is that it changes the context of death, and therefore the meaning of death. It gives us a glimpse of what death might be if it took place not in the helpless panic and emptiness of the ER or the ICU but at home, in the midst of a family newly reunited by the event, the dying person having taken care of all that kept him from moving on.
MOVING ON
Even to use such-a phrase as “moving on" implies, of course, a prodigious leap off the train of conventional medical thought and onto a different set of tracks altogether. It implies that we — or at any rate something of ourselves — survive death and continue in some other form of existence.
It’s often said that death is a mirror that makes us reflect on life. I want to look for life through death, like a physician examining the brain by shining a light through the black vacancy of the pupil or an astronomer wishing he could peer through a black hole to glimpse bizarre counter-realities on the other side.
In a hospital, death is a medical death. Everything, or so it seems, can be explained in the accepted medical terminology of the time. Hospice offers a chance to see death in a different light than the brilliant glare of the hospital, a chance to experience it more directly, in our own words and through our own assumptions. Hospice has also given authority and respect to those farther down the vanity ladder, to nurses, aides, volunteers, patients, and family members, those less thoroughly versed in the clinical explanations, and the results are startling. Probably the most commonly recommended book on a hospice bookshelf is Final Gifts, written by two hospice nurses who mattcr-of-factly spend over a quarter of the book discussing near-death experiences, those remarkably common intimations patients have of their own imminent death and the conversations they apparently have with those on the other side.
By dismissing such experiences, as many in mainstream medicine do, calling them hallucinations, we change the entire nature of the experience of death, denying comfort to both the dying and their families and, as the authors, Maggie Callanan and Patricia Kelley, point out, often causing great agitation and anxiety' to the dying who are trying to tell us the marvek>us things they’ve seen. Kathy Ferdinandson passed on two such stories.
An elderly woman’s husband had passed away several years beforehand. She was convinced that she would meet him in heaven and looked forward to the day when she would die. A week before she died, she said, “Kathy, I’m going home." She was in a skilled nursing facility, and Ferdinandson misunderstood her drift. “You are at home,” she replied. “This is your home.” She looked hard at Kathy. “I’m going home," she repeated firmly. Within a few days her physical condition took a clear turn, and she began actively dying. Kathy found her holding a conversation with John, her late husband. The nursing staff had noticed it too, though they dismissed it as hallucinating. When Kathy sat down next to her, the woman turned to a spot elsewhere in the room and said, “I will, John, I will."
“Who were you talking to?” Kathy asked.
“To John,” the woman said. “He was asking me if I was coming home.”
She died that night. Kathy believes that he had come to assist her in making the transition.
The second story involves a man who was seriously ill and so frightened of dying that he refused to talk about it, which made the hospice work very difficult. He had been on service for a while when his mother came to visit with the intention of helping take care of him. Shortly after she arrived, she had a heart attack and died on the kitchen floor. He was terribly upset. Kathy suggested, “Could it be possible that she died first to be the one to go ahead and show you the way, to help you over your fear of death?” He didn’t seem to want to entertain that notion.
Shortly afterwards, he began actively dying. The doctor noticed that he seemed to be looking at and responding to things that weren’t in the room and again considered what was happening to be some kind of hallucination. “Are they frightening?” he asked the patient. “Would you like me to make them go away?” — that is, by medicating him.
The man looked clearly at several different and distinct places around him. “No,” he said. “They’re beautiful.”
“What I thought,” Kathy said, “was that they were angels or spirits come to help him over because he thought death was so despicable.”
Near-death experience stories, brought back to us by the revived, are by nature less common in hospice, where revival is usually not the point, than in hospitals, but anyone who has broad experience with death has run into them.
“I’ve had patients say to me, ‘I saw that light, and I came back because I hadn’t finished telling my kids what I wanted to tell them,’ ” Laurel Herbst said.
“You’re not afraid when you’ve had someone die and come back to life and tell you about life on the other side,” said Joan Snyder, a staff nurse at Scripps Memorial Hospital, Chula Vista. “We had a physician who died on the golf course. He was coded. We kept bringing him back and bringing him back, and he said, ‘I’m happy where I am. Leave me alone.’ I’ve had people say, ‘I know you.’ I’ll say, ‘You can’t know me. You were coded when I was working on you.’ ‘No, I know you. I was up there in the corner watching.’ ”
AN UMBILICUS TO GOD
I can’t claim to have gone through this investigation unbiased or unmoved. But whose ambition is it to be unmoved by death? And what can we learn only by allowing ourselves to be moved? At the end of her session with the medical students, Judy Davis finally turned to the cornucopia of found objects that we had picked over two hours previously. She asked us to use one of the items that we had picked to make a point about grief, and the gist of her message seemed to be that if doctors use such third-party narrative ingredients or symbols, they are forced out of doktorspeak, they have to want to communicate clearly. But something weird was going on, all this talk about grief must have stirred the pot for me, at least, because I abandoned my journalistic detachment, not to say my common sense, and showed the group my polished purple stone and told them about my vision of the chromatogram of the soul.
In the weeks after my mother’s death, I said rather selfconsciously, I spent a lot of time in an odd, otherworldly state of joyful detachment. I was still operating in the material world, but it seemed to have lost its power to upset, irritate, or depress me, and instead of seeing reality at this stratum of anxiety, this stream of things-that-had-to-be-done that twittered like the gibberish on a shortwave radio, I felt as if I had an umbilicus to God. I moved at my own pace, possessed of a constant sense of wonder, and every so often I would see or think of something that sent a rush of sheer joy up through me, and I would clench my fists and think Yes! Yes!
It was as if I had moved to a new dimension that had always intersected with the world I knew, but I had never seen it — and even now it was not visible, though it was almost tangible, but I could sense it everywhere and see its outcomes and effects protruding into the events of ordinary being like the tips of warm icebergs. I found myself instinctively carrying out small acts of kindness or courtesy—waving drivers ahead of me at intersections, exchanging pleasantries with supermarket cashiers — and seeing joy and kindness everywhere in return.
During this remarkable time, I suddenly had a sense that I could imagine a chromatogram of my soul — not that I could see it, but that I knew what it would look like if it existed in visual terms. It would be rather like this polished stone, only instead of being predominantly purple, with fascinating flecks and spots of other colors, it was mostly yellow and white, with clearly defined dark patches like small vortices that were the parts of me that I still hid and was afraid of.
I was sorry to be so mystical, I said, feeling a little embarrassed, but one of the things I suspected about grief was that a death in the family takes us (in some instances, at least) through a more essential tijne in which we briefly realize how much other people mean to us and how powerful and lasting and redemptive this emotional or spiritual dimension of life is. When we stumble away toward our ordinary, workaday lives, their demands and values seem petty, unwholesome, ungrateful, demeaning — they miss the point. Everything seems like network television and junk food, spiritually destitute, lacking any real nourishment. We resist going back to it, and we are right to do so, seeing clearly its limitations. Yet everyone around us tells us that this is the real world, this is normal, and we simply must knuckle down and get back into it. No wonder some kinds of grief mimic depression.
The tragedy, then, is not so much when someone dear to us has died, but when we have the chance to learn something miraculous from this, their last gift to us, but don’t. Even as I write this, I find myself glancing at the clock, at my date book, checking to see what I need to do this afternoon, giving tiny mundane obligations the chance to throw me off stride, flinching away from the challenge of asking, “How would it be to live life well?” the weight of my habits slamming into me like small cars on a freeway hitting a tractor-trailer that has come to a halt sideways across all three lanes, pondering a turn to the right where no asphalt has yet been laid.
Yes, this is a strange form of journalism, isn’t it? But somehow it all leads up to this, that death, once the fear is overcome, is our severe but brilliant tutor on life, demanding nothing less than the truth and offering insights that leave us reeling, saying, “Leave your computer right now, stand downstairs in the winter sunlight for a while, and you will know what to write, saying that there is pain and loss but there is no need to be afraid. ”

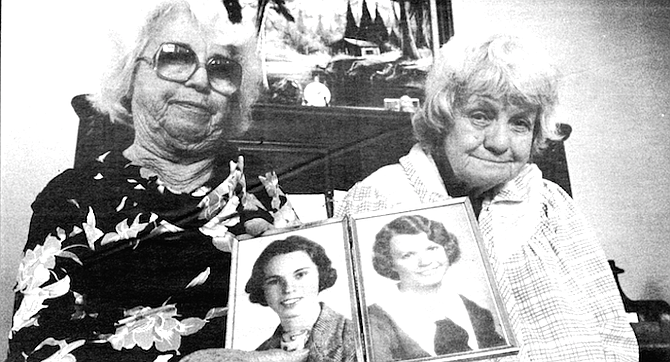
When someone dies in the state of California, we know, or can find out, what would seem to be everything we might want to know about the event: the place, date, and time of death; whether death took place in a convalescent hospital, at home, or other and if in a hospital, whether in ER, OP, or DOA; the names of a whole fleet of relations; whether it was from natural causes or by accident, suicide, homicide, pending investigation, or could not be determined; what the immediate cause of death was, and what cause that was due to, and what that was due to, and even what that was due to (along with any other significant conditions or operations); how long each of these contributory conditions kicked in before the patient kicked off; whether a biopsy or autopsy was performed; when the decedent was last attended by a doctor and last seen alive; the name (and license number) of the funeral director, the signature (and license number) of the embalmer, and the place of— ahem — final disposition.

But nobody knows the really important data on how we die. How many of us die painfully? Nobly? Tormented by regrets? With a sigh of relief? Peacefully? Angrily? Alone, lonely, and abandoned? Alone, thank God, at last? Surrounded by our relatives who have gathered to respect our life and our passage onwards? Surrounded by relatives who have gathered to squabble over our will?
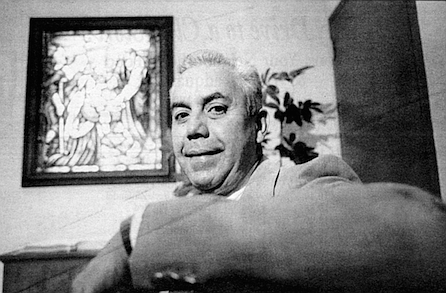
To have some influence over how we die might seem to be one of life’s greatest ambitions, yet there is absolutely no reliable information on how people die or how they achieve a consummation devoutly to be wished, or to be feared. This unclear outcome is the linchpin of our fictions—the good dying peacefully or tragically, the bad falling from a great height onto sharp objects, the death perfectly or ironically illustrating the quality and virtue of the life—yet in real life we give no serious attention at all to how we ourselves want to die and how best to achieve that goal.
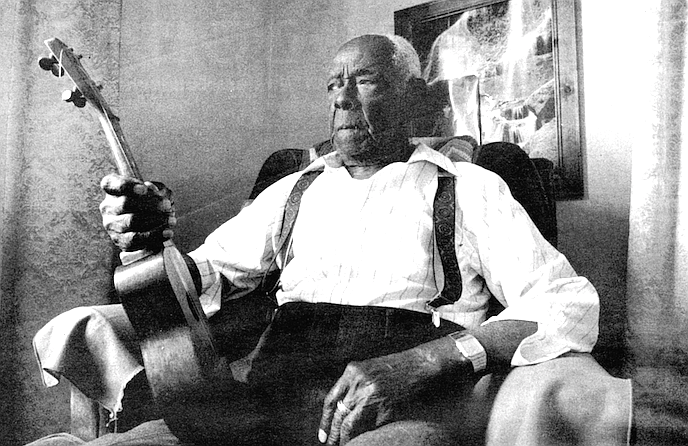
It’s a puzzle. We must be at least somewhat curious about it, given that a third of a million of us have bought Sherwin Nuland’s book How We Die, but all Nuland tells us is that we mostly die of disease processes that ultimately deprive some crucial muscle of oxygen. Yet most of us, in fact, spend most of our lives avoiding even thinking about death or what we want to make of it.

Which is more than a pity for two reasons. First, avoiding thinking about death tends to lead to exactly the death we fear; and second, there is an organization in San Diego whose sole purpose is to try to help us achieve (within limits) the kind of death we would like. Its name is — “Oh, for Pete’s sake,” you break in, “not another morbid article about death, surely?” Well, all right. In due course I’ll take you up on the notion that considering death must be morbid, but for the time being I’ll stick to safer ground and begin by looking at a weird and radical change that took place in medicine 50 years ago.
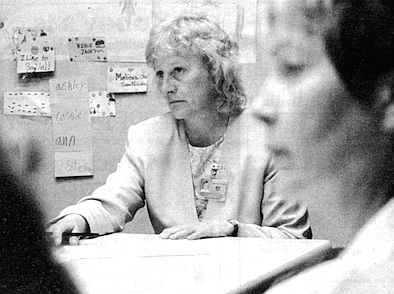
A BRIEF HISTORY Of DEATH
“If you look at American medical literature through the 1800s and 1900s,” said Dr. Laurel Herbst, medical director of San Diego Hospice, “death is accepted as inevitable. It’s the normal process, the classic lithograph of the physician at the child’s bedside— which, by the way, hangs in my living room. That was the norm."
The role of the doctor, in other words, was more compassionate, less technical. Sir William Osier, the great turn-of-the-century clinician, said that a physician needed three qualities: availability, affability, and ability, in that order. The doctor’s most valuable quality was his humanity in the face of a death that was all too often inevitable, even as a result of what we nowadays regard as minor illnesses.
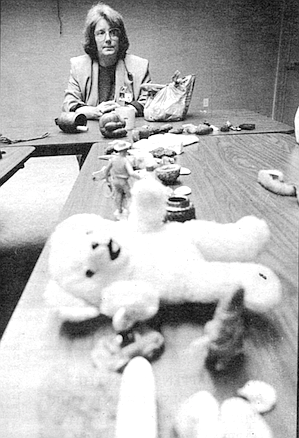
But warfare is the mother of invention, and the Second World War vastly accelerated the development of medicine. Antibiotics, for example, developed rapidly by being tested in battlefield conditions. “We’d never have taken the risks in peacetime,” Dr. Doris Howell, a professor emerita of pediatrics at the University of California at San Diego Medical School, said caustically. “You don’t have to worry about ethics during a war.”

“And with penicillin,” Herbst said, “and with a couple of other drugs thrown in there, we, in a typical American fashion, just like in the Industrial Revolution, took off on another technological revolution. We’ve got drugs! We can fight things! We can make things better! We can change from these compassionate, hand-holding physicians into real fighters..,. We were absolutely convinced that if we threw enough money and technology into a problem, we could solve it. And then cancer really stymied us, and there was suddenly this realization that we aren’t going to win the war on cancer. Not in one drug, not in one Nobel Prize-winning breakthrough.” Medical science, which had seemed irresistible, had met its match, not only in cancer but subsequently in AIDS and, though this had somehow been overlooked in the heat of everyone’s enthusiasm, in death itself.
This has radical implications for how to treat patients with potentially terminal illness, how desperately to try every possible treatment before acknowledging death.
“I’m 47,” said Dr. Mary Margaret Loehr, codirector of the emergency department at Scripps Memorial Hospital, Chula Vista, and also a per diem physician at San Diego Hospice, “so I graduated from medical school in 1973. I was taught, as were all the physicians older than me and many physicians even younger, that it was my moral, ethical, and legal obligation to do everything I could for every patient.
The difference was that even in 1973, while we thought we could do a lot, say, in comparison to my father’s generation, compared to what we could do now, doing everything is nothing.
“When I was a medical student, taking care of an elderly patient with pneumonia, I ran out of drugs after one or two tries — even if I was excessively aggressive, I only had two or three weapons. Now we can be excessively aggressive for months and go down a whole formulary. So the inherent physical limitations on a physician’s ability to continue to intervene have been pushed back; and as a physician, to watch it happen — it’s staggering. We only used to put really pretty healthy people on dialysis; now we put 90-year-olds on it. So that as a physician, if I was inappropriately aggressive 10 or 15 years ago, the body stopped me anyway. Now that frontier is really pushed back, but the training hasn’t changed.
“And the other piece,” she continued, “is that as a physician you are trained that you must do even more for your patient than you would do for yourself or your own family. You leave your kids and your wife at home, and you get up and go to the hospital at night to take care of John Jones because he’s got chest pain. That is what you do, that is your ethic, that is your standard: do more. And we can talk a lot about rich physicians and all kind of other garbage, but by and large the huge mass of physicians has been trained — whatever it takes, whatever it costs, personally, professionally, economically, you must do whatever you can for your patient. The idea that we need to stop thinking in terms of doing whatever you can and start thinking in terms of doing what is best was never even before a question. Never had to be explained, because whatever you could do was best, and the best for the patient was whatever you could do, and they were equivalent in the medical thesaurus. They aren’t anymore.
“Within one generation we’ve gone from hand-holding to true therapy. Her father and grandfather were physicians, and there was a time when all they could do for someone with pneumonia was to hold their hands; they were part physician, part father figure, part shaman, part pastor. If they were called at 2:00 a.m. and told that someone had pneumonia, they knew that their job consisted of going to and sitting with the patient until he or she died. Now, her grandfather pointed out, when she is awakened at 2:00 a.m., whether she’s alert or not and whether she’s thinking or not may decide whether the patient lives or dies.”
Doctors were changing, medicine was changing, and hospitals were changing, developing their own gravity, drawing the practice of medicine toward them. It’s no coincidence that around 1940, for the first time in history, more babies were born in hospitals in the U.S. than at home. With medicine becoming ever more scientific, and its scientific equipment becoming ever more expensive and ever more centralized, and the public constantly tugging at the doctor’s sleeve, begging him to do something for the dying relative, between 1945 and 1995 the majority of Americans made a change that would previously have been unthinkable. We chose to die in the hospital.
A TERRIBLE PLACE TO DIE
Of course, we don’t see it that way. We rush to the hospital to try to avoid death, which is precisely the problem. The place that Is designed and equipped and staffed to avoid death is bound to convince both patient and family that death is one of the worst things that can happen. The flashing lights and the siren of the ambulance, the muttered orders, the efficiency and haste, the blinking lights and beeps of the monitors — everything that conveys urgency also conveys panic and implies meaning: that death is to be avoided at all costs. When else are tens of millions of dollars of equipment rushed to our disposal? For what else are we charged $5000 a day? It must be a terrible thing, this death, for us to mobilize such forces against it. If we detest hospitals so much — and it’s hard to find anyone who doesn’t — but we go there to die, it must be because we’re even more afraid of death than of hospitals. But hospitals convince us to fear death...and down we go in a whirlpool of fear and circular logic.
Once the heroic measures are clearly not working and the urgency fades, the hospital becomes little more than a warehouse in which the patient is stored (at enormous expense) until he dies. “You feel guilty [because] it becomes part of your routine,” explained Ester Sarabosing, R.N. “You’re not really spending time with them. Often they’re the last person you deal with because you think, well, they’re dying. For the first few days, for the first week, you spend the most time with them, but after that they become your last priority.” She told me the story of a man who was expected to die quickly but clung on for two weeks. During the first week his wife visited every day; on the second week she was down to an hour or two. “I was uncomfortable. He was no longer here but he was still here. When he finally died, everybody was relieved.”
Part of the reason a hospital is such a desolate and londy place to die is simply a lack of time to treat each person as an individual. “We get 50 or 60 people a shift,” said Joan Snyder, R.N., who works in a San Diego emergency room. “How can you relate with everyone you see? You don’t have that much to give out.”
But part of it also has to do with the bleak meaning that mainstream medicine ascribes to death. A medical education, whether a doctor’s or a nurse’s, does almost nothing to prepare staff to help patients and families through death; it doesn’t even prepare the staff to help themselves. Instead, they learn survival. The newly qualified nurse or doctor in the busy hospital, faced with death, is supposed to sink or swim and to learn to do so alone, without help, without any recognition, even, that he or she may be drowning.
“It’s very, very overwhelming to new nurses to deal with death on a daily basis when you don’t have time to deal with it,” Snyder explained. “It leaves a lot to be desired. It’s not discussed. They watch what you do, and if they see that you’re coping successfully with the attitudes you have, then they adopt them. In nursing school they never teach you about death. They don’t teach you about you, about your profound feelings about death and dying. You don’t know what to do about the anger and sadness that you feel when you have to deal with a newly diagnosed cancer or a person who’s just become a paraplegic or a quadriplegic. After a while you develop a [surviva] attitude, and if you haven’t got that, you flounder.”
When a medical student or student nurse does encounter death as part of his or her education, it often happens in a grim and harrowing fashion that may bear little or no resemblance to an actual death. Ester Sarabosing grew up in the Philippines; her first experience of death was that of her grandmother. As a young girl. Ester knew her grandmother as an active, alert woman. As she aged and became senile, Ester, by then a teenager, cared for her, as she was expected to. When her grandmother finally died, the whole family mourned and missed her, but Ester learned no fear of death from the experience.
Curiously, when I asked her about her first experience of death, what sprang to her mind was not the peaceful and natural death of her grandmother, but the dissection class in nursing school and the smell of formaldehyde. “What I remember most vividly is my first year of nursing and the smell of my first time in the morgue. When we had to go to the commissary afterwards to eat, the smell stayed with us and lingered for a week.”
It’s all too easy for that survival attitude to be simply a kind of emotional insulation, a just-do-your-job-and-get-on-with-the-next-case teeth-gritting that to the outsider can seem callous. The traditional hierarchy of the hospital makes it easier for the doctor to avoid the emotional content of death than for the nurse, who is left to deal with the aftermath, like the wife being left holding a soiled diaper while the husband goes off to work at Paine Webber. “The physician goes in,” Joan Snyder explained, “and tells the family that their loved one is dead. ‘I’m very sorry. I did the best I could, and my nurse Joan will take care of any problems you have.’ They have at most a five-minute involvement with the family, and then their duty is ended.”
Medical education is crucial, because medical personnel in turn pass on their beliefs about death, directly and indirectly, consciously and unconsciously, to the public — to patients and their families. “They don’t teach them that it’s okay to die at home,” Snyder said. “They don’t teach them that it’s okay to die. They give them the impression that there’s still something to be done, when there isn’t. They’re told, ‘We can do this, and this, and this,’ but they don’t say that they’re going to die.”
The more I listened to the medical personnel, the more the hospital, the institution, began to resemble Fortress America, that symbol of embattled solidarity that recurs with curious frequency throughout American history, from the earliest European settlements through the Alamo to Khe Sanh and Waco. Maybe it has to do with a militaristic mindset or a failure to conceive of community as the basis for civilization; but as in Vietnam, we’ve trucked and helicoptered in the most modern equipment and the most highly trained troops, and once again they’re in danger of being overrun. The hospital simply cannot fulfill all the roles expected of it.
“It goes back to the family and the support system,” explained jeannie Binder, R.N., of Scripps. “Most of our patients could be at home. There are not many things that need to take place within the hospital walls. There’s not any magic to delivering morphine or suctioning the patient. There’s no place for a hospital as we have them. Why should you spend $1000 a day just to be in here, to get this food, when you’d rather have a bowl of chicken noodle soup or a bologna sandwich anyway? If you’re a smoker and you want that last cigarette then, Jesus, you should be able to have it.”
All the parties involved conspire to make death harder. Death with dignity is easier for all concerned if the patient is informed about his condition, has considered the treatment he wants (or doesn’t want), and has talked it over with his family. But the double role of the hospital makes denial vastly more common. Edna Monzon, R.N., reported that although most of the intensive care patients at Scripps are 75 to 90 years old, and most have been in here time and again with chronic illnesses that will finally kill them, most have refused to think about death, let alone plan for it. “A lot of the time the family thinks, ‘This is just one episode. He’s a fighter. He’ll come out of it.’ So when they come into the hospital, they’re still hoping for the best; and when the patient turns sour, it’s hard for the nurses to get through to them.”
Meanwhile, most medical staff don’t have the time, the training, or the inclination to help a patient talk about his approaching death or help the family with their grief. Many physicians (and some families, especially those of Hispanic and Asian origins) still believe that a patient should not be told of a terminal illness.
“A person who’s diagnosed with a terminal illness should be told up front,” Joan Snyder said forcefully. “That’s where I think hospice is just great. They say, ‘We’ll teach you.’ There’s so many things to learn, and you only get to go through it once.”
Meanwhile, the need for sterility and efficiency creates its own diminishing returns. The patient feels like a stain on the crisp white linen, an inconvenience to the crisp running of the staff s schedules. The more miraculous and effective the technology, in theory, the more the physician, too, becomes a liability. As one doctor has written, the machinery of medicine needs to be infallible, which leads the physician to feel that he, too, must be perfect or else be shown up as the weak link in the system. In practice, no hospital has that kind of budget. Instead, everyone is aware of the space they don’t have, the equipment and the time they can’t afford. By thinking of medicine as something pharmaco-technical, we have helped to create a climate in which bitterness and frustration are epidemic. Death is simply the occasion when these feelings arise most vehemently.
Last fall I followed an old rum-runner’s trail up into the Green Mountains of Vermont, past a trout lake and up among the birches and blazing maples. Leaves rustled and crackled underfoot, sometimes six inches deep, and the silence of the woods was constantly punctuated by falling leaves and twigs. Above an abandoned beaver pond with its lodge and dam of grayed branches, one entire hillside had lost its leaves early, and the exposed branches and twigs blended into a mass of woven silver thread. Everywhere else the maples were crimson, red-gold, orange, yellow. What a paradox, I thought; in a hospital we try to avoid and conceal death, and as a result we create an utterly alien setting, a cross between a stationary submarine at permanent battle stations and a warehouse stocking nothing but sickness and blank suffering. Out here, time and change, growth and death, are unavoidable, are everywhere, yet the landscape was inexpressibly soothing, and the bad mood I’d started out with quickly evaporated, leaving me both alert and peaceful. It would be no great shame if I were to die here, I thought; and who knows if our panic and hand-wringing in the hospital corridor are at the thought that someone is dying or that someone is dying the wrong death, in the wrong place?
IN THE ICU
In the intensive care unit of a hospital in San Diego County, I catch a glimpse of a man splayed in the characteristic abandon of unconsciousness or a baby’s sleep, mouth gaping, an unnaturally beige-chosen-as-skin-color pair of tubes running out of his nose. It’s hard not to imagine it’s the other way around, and they are snaking into the nearest available orifice while he sleeps. In the next room is a Jane Doe. She is reaching feebly for the gadget that adjusts the electric bed, but her hand is entangled in her IV tubing and she can’t reach it. Nobody notices. At the tiny nurses’ station opposite, surrounded by beeping cardiac monitors and small black-and-white, closed-circuit screens, a young nurse has just gotten off the phone. “Can you believe it?” she is demanding of the four people gathered in the narrow hallway. A patient’s next of kin can make it over from Texas, but they have nowhere to stay and want to know if they can sleep in the lobby or on the floor of the ICU. “Can you imagine?”
As I was interviewing hospital staff in San Diego County, something Joan Snyder told me kept turning up in my thoughts. “I'm not Catholic, but I’m very, very sorry that Catholics have given up on the Last Rites. We serve a very large, very Catholic Hispanic community, and it’s a great loss when there’s nobody there to say, ‘Your loved one is with God....’ It’s been years and years and years since I’ve seen a minister or a priest or a rabbi come to the ER. If they’re a religious kind of people, they need that support now. Not three days down the road.”
Come to think of it, I’d never seen a chaplain in a hospital either, though I’ve seen a chapel. (Not that it means much. Even airports have chapels.) Surely we could use some spirit-lifting, even when we’re temporarily ill, let alone when we’re terminally ill. And I remembered a study that revealed how a great many ministers are just as uncomfortable about death as anyone else, and a story of a chaplain who would never go into the patients’ rooms but tried to talk to them from the doorway.
Glancing through the Yellow Pages under “Hospitals,” then, I was surprised to see “Chaplain” listed as one of the departments of Paradise Valley Hospital. How can a chaplain function in a modern hospital? I wondered. What good can he do?
Chaplain Wilfred Reyna turned out to be a well-built man of medium height, possibly in his mid-50s, with magnificent eyebrows and silver hair brushed neatly back from his temples, dressed in a dark blue blazer, striped blue shirt, and tie. He spoke quietly, carefully, perhaps a little regretfully, with a slight accent I couldn’t place. His office was tidy and formal rather than warm.
In his 14 years at Paradise Valley, he began, he felt that he had done “an imperfect job of trying to provide a spiritual presence in the hospital.” The fact that the hospital, which is affiliated with the Seventh-day Adventist Church, gives him an office and employs him full-time is a sign of its commitment to its patients’ spiritual needs, he said.... An unspoken “but” hung in the air.
“We’re supposed to be more focused on the spiritual dimension, but what comes across to the patient depends on the personalities of those whose lives are touching the patient’s. There are a few doctors, unfortunately very few, to whom the religious aspect matters. They may stop me in the hall and say, ‘Oh, chaplain, I just diagnosed a patient with terminal c.a. (cancer, that is, in the usual hospital abbreviation/euphemism). They and their family may need some support from you.’ Many doctors are very uncomfortable leaving things to a higher power, to something beyond what they can control. If it’s not measurable, it’s not credible. With the majority of doctors, only when the patient is near death will they say, ‘It’s in God’s hands.’ ”
This makes perfect sense. The medical profession, too, has its faiths and its creeds, some of which stand in stark contrast to those of most religions. Every visit to the doctor is an opportunity for secular proselytizing, a chance to reinforce our belief in scientific materialism. I had a vision of the chaplain bobbing unhappily around a ring of medical personnel surrounding a patient like a stockade.
His self-appointed rounds go roughly as follows, he said. First, a brief devotional service—“a thought, a prayer, sometimes we sing” — with perhaps two dozen patients and staff in the inpatient psychiatric unit, then around 10:00 a.m. a similar meeting with the outpatient psychiatric group....
His beeper went off. Code blue in the emergency room, the dispatcher’s voice said. “I have to do that as well,” he said, half-apologetically. I asked him if he needed to leave at once. No, he said, glancing at the clock; for a code blue he would probably be needed for the family rather than the patient, “who is surrounded by doctors and nurses and technicians,” and it would probably be some time before the family arrived. It was about 3:20 p.m.
“After that, I drop into intensive care and post-intensive care,” he said, continuing to describe his daily routine, “and I try to visit the other floors if I’m not being paged too often. I’d have to say my work is basically crisis driven.”
Despite the hospital’s Adventist affiliation, he said, it was his job to try to minister to all faiths as best he could or bring in colleagues from the community. “I try hard to be a generic chaplain,” he said, smiling a little thinly. He once stayed with a grieving Japanese woman for two hours, he said, finding out eventually that she was Buddhist.
He was paged again and called the ER. As he listened, he made noises of concern, and his face was grave.
“Bad news?” I asked.
“A baby,” he said. “Didn’t make it.”
Almost immediately he was called again. The family had arrived. He invited me to follow him, and we headed briskly down the featureless corridor.
“This is a shortcut,” he said, and we passed from the groomed corridors of the administration section into an area that had the combination of elementary school and medical supplies warehouse that is instantly recognizable as an emergency department. Reyna looked a little hesitantly at the group of three nurses, one of whom directed him to a doctor in an impossibly small cubby-office behind their station. “It looks like suffocation,” the doctor told Reyna. As they spoke, I glanced through the open door of the room adjoining them. I caught sight of a bed that was empty — no, occupied at the far end only: some tubing and a small white blanket and something dark in it. Two young cops appeared beside us in yellow rain slickers, and it struck me that nobody knew if we were dealing with accidental death, SIDS, or murder.
The family was in a small room at the end of a short corridor — the mother, a beautiful young Japanese-American woman with the kind of skin blemishes that sometimes come with bad diet, and the father, an African-American in a maroon sweatsuit and Reeboks, nearly six feet tall, and built like a running back. She was wearing skintight pink exercise pants and boots. I honestly can’t picture what kind of shirt or jacket she was wearing. All I can see is her crying into her long black hair and her empty hands, held in front of her as if she were tom between wanting to reach out to hold someone and wanting to clutch her head. “My baby,” she cried. “My baby. My baby.” A young hospital social worker, in her 20s, was sitting next to her saying in an oddly upbeat tone, “This is the worst thing that can possibly happen.”
The father seemed to have frozen, staring at the floor. A nurse was taking their names, but he seemed not to hear anything she asked. Reyna tried to pat his shoulder, but he shrugged him away furiously. With each moment the father seemed to withdraw further, to become almost catatonic. Afterwards, Reyna told me he couldn’t decide whether the man was in shock or was trying to concoct a story to cover his actions.
Nothing was clear. The father had been at home, the mother somewhere else, apparently. They’d last seen the baby alive, asleep, at 9:30 or 1:00 a.m. The father had taken his daughter—by a previous marriage? — to school at some point and had then taken a nap — When? For how long?
Nothing fitted together. The baby had been lying oh “a big bed,” because they couldn’t afford a crib and had fallen or slipped into what the mother called “a hole” — a crevice between bed and bumper? The father had tried CPR, they said, but when was all this? The doctor had said that the baby had been dead for a couple of hours....
The door opened and another young African-American man peered in, and at once everything changed. The father recognized him, jumped up, and for a moment the two seemed to be wrestling, but then the father burst into tears, wailing, thrashing, while the other tried to comfort him and at the same time pin him down on the couch. The chaplain stepped back, nonplused, and I didn’t blame him — either man could have floored both of us in a second, and we still had no idea if we were dealing with a man who had just killed his own son.
“He’s all alone,” the mother said pitifully. “He’s all alone.”
One of the cops came in and stood uncertainly by the door, making the tiny room even more crowded. The newcomer turned out to be the father’s brother; the bereaved family’s other two kids were staying at his house for the time being. By now the mother, who was being ignored by the two men, was asking if she could see her baby, and it made sense all-around to usher her out into the corridor, leaving the two men together under police supervision.
Even so, nothing was easy, and Reyna’s job demanded that compassion be tempered by protocol. The parents couldn’t touch the baby, who in a grim way had taken on a new identity. It had become evidence. Reyna explained hesitantly that the coroner would shortly come and take the baby away to examine him. “Exam -ine?” the mother asked, uncomprehending. “Conduct a...post mortem,” Reyna explained awkwardly, “to see how your baby died. He’ll be done by...maybe tomorrow afternoon. Then you can make arrangements with a mortuary.”
Post mortem. Arrangements. Mortuary. Death involves a great deal of novelty, many difficult changes of direction and perspective. Taken one at a time, we can steer around or through them, stiffly, uncomfortably. When they arrive all at once, it’s like hitting a rock face.
The room was both barren and cluttered. All around the walls was the familiar ER paraphernalia, boxes and bags of sterile supplies, notices, like a large poster for “Easilav Adult Lavage System," that meant nothing to the uninitiated. All this and you couldn’t save my baby.... I’m injecting my own feelings here, I know—for the parents seemed oblivious to everything but the baby — but I could see how people could take the blank sheet of death and paint onto it their own feelings of the moment. This room was a self-fulfilling prophecy, the comfortless desolation of the room could all too easily become the comfortless desolation of death. By assuming clinical death, meaningless death, the final breakdown of the body’s systems followed by nothing at all, medical science and medical architecture have created an environment in which death can be little other than that. The context becomes the feeling and the meaning.
And a vicious circle starts spinning. The more empty and meaningless death seems to be, the more afraid of it we become, the more we tug at the oncologist’s sleeve, whimpering, “Please, doc, can’t you do something?” and we commit ourselves to the stainless grasp of a medicine that becomes ever more expensive, ever more invasive, ever more sterile. By running from it, we create the death we dread.
The mother was pleading to hold her baby. Reyna looked uncomfortable and went out to the hallway to talk it over. The group of nurses at the counter reminded me, bizarrely, of waitresses at a truck stop.
The nurse Reyna was talking to shrugged. “What are they going to do by holding him?” They looked at each other uncertainly for a moment, then Reyna went back in to the mother and told her she could hold the baby. “It’s against hospital protocol,” he muttered to me under his breath, looking unhappy.
The mother picked up her son carefully, as for some Dr. Laurel Herbst reason he was still attached to a tube and gathered him in the hospital blanket, which looked exactly like a receiving blanket. “My baby,” she repeated helplessly.
Back in the little waiting room, the father eventually pulled himself together, refused a sedative, and asked, a little belligerently, if he could see his baby. How could he know what he would and wouldn’t be allowed to do and what he might have to fight for? “Of course,” someone said, and he went down the corridor. When he saw his son, he seemed stunned. “He ain’t dead,” he said. “Look at him. He ain’t dead.” The baby looked asleep. He had reached the age when children look physically perfect, but still helpless. He had stunningly beautiful eyebrows, jet black against his lighter skin, and unusually straight and well defined, like acts of calligraphy.
This must be as bad as it gets. Sudden death, whatever we may say about wanting to go quickly, without knowing what hit us, creates the hardest grief to heal. Sudden infant death is the worst of all. The previous day, Susan Inot, director of maternal-child health at Scripps, had explained to me how they deal with stillbirth, bringing the baby to term and delivering it, encouraging the parents to claim the baby as their own. The labor itself gives the family time to take in what is going on, she explained. But here — this is the brick wall.
The father crouched in a corner, holding his head in his hands, muttering, “It’s my fault. I shouldn’t have...I’m supposed to be his father. How could I...” in a desperate monotone. His brother and one of the cops had disappeared; the other cop, a baby face on a huge body, wearing so much equipment on his chest he looked as if he were about to erupt with some spiky mechanical, alien, stood unobtrusively in the background, and I, for one, was glad to have him there. It no longer mattered who had done what. Someone that upset might do anything, might take sudden and furious offense at my presence or that of the chaplain (whom he had still barely acknowledged) or the social worker, who still seemed oddly chipper.
The mother stood at the head of the gurney, crying, asking Reyna questions he was wise enough not to try to answer.
Every so often he patted her on the shoulder. At a glance, the chaplain might have seemed to be doing almost nothing, but there was almost nothing to be done. Certainly, this was no time for pious platitudes or religious pronouncements that might actively irritate the family, given that their religious beliefs, if any, were still unclear, like the social worker, he was there; and if she was taking advantage of her youth and gender to offer more obvious comfort to the mother, he was better able to offer the calming presence of one who has seen more of the world, that parental gravity and stability that we sometimes want to cling to. In a colloquial sense, at least, this is a spiritual gift, if not a religious one. But all this is guesswork. They might not even have known he was there. The belief that he does any good must also often be an act of faith.
For what it’s worth, I was also engaged in an act of faith. I imagined myself sending my soul out to them, gliding across the room like a manta ray to embrace and comfort theirs. I felt like the angel in Wim Wenders’s Wings of Desire, watching them full of compassion, standing in another dimension. The parents, of course, paid me no attention at all. Who knows if this can really happen and you really can send your soul out flapping across the room like a sand ray, and even if you could, whether it would do any good or whether it’s just an act of well-intentioned self-deception, and you would just exhaust yourself in the process trying.
In the end, it was the mother who established the father’s credibility, if only temporarily, by forgiving him. “It’s not your fault,” she told him over and over, through her own tears. “Don’t blame yourself.” They formed themselves into a tight little protective knot, the mother with her arms around the baby, the father with his arms around the mother, and that’s how I last saw them, for a minute or two later a capable-looking woman in her 40s, wearing jeans, a plaid shirt, and a yellow rain slicker, arrived and announced that she was the crisis worker from the police department. “Looks as if you’ve got more than enough people here already,” she said, but the hospital social worker and the chaplain handed the situation over to her with some alacrity, and Reyna and I made our way back to his office.
For the chaplain, too, everything happens too quickly, and unlike the nurses and doctors, he doesn’t have another case waiting that will at least give him something to do with his hands, a chance to do better this time, to draw him back into his sense of his own value. When I left them, they were a bundle: the mother holding the baby, the father holding both of them, the worker from the crisis intervention program with her arms around them all.
“Who looks after you?” I asked Reyna as he sat back down behind his desk.
“That is an issue,” he conceded, and sighed. “If I’m going to be effective, I have to be affected.” He paused. “I don’t have anyone in whom I confide. I have a lot of clergy friends, but clergy are used to being... prescriptive. I need someone to enter into it with me and go down into my valley, and only then can they help me.” He might have been talking about doctors, I thought.
He deals with the stress, he says, by trying to keep fit; he has NordicTrack in his bedroom. “My doctor told me I have the blood pressure of a 20-year-old,” he said proudly.
We shook hands and I left, feeling suddenly drained. What was most demanding was not the act of sympathetic connection, which has the sublime, sustaining quality of any act we believe to be wholly worthwhile. It was the re-entry afterwards into a world that seemed much more mundane and therefore, in a curious way, harder to take. Back in heavy traffic on 1-5, a sudden headache hit me like a squall line, and I felt very tired. If I were an ER nurse or doctor right now, I’d be denying my next patient something by having allowed myself to be so affected; but then again, if I didn’t allow myself to be affected, wouldn ’t I be denying myself something? One of the wisest things we can know, it seemed, is who we want around us when we have to grieve.
When I headed up the Coronado bridge between the patchy lights into the rain and darkness, it looked as if I were driving off the planet.
ABOUT THE AUTHOR
At this point, I should put my cards on the table. In 1979 my father died what I have come to think of as the standard brutal aggressive-oncology death, in England. After six months of increasingly disturbing symptoms, he was told he had cancer of the lymph system. Not to worry, the specialist said, they’d try this; and if this didn’t work, they’d try that. Chin up, what? Heavy, then heavier doses of radiation left him looking bruised and yellow, with a perpetually dry mouth; chemotherapy made his hair fall out and left him vomiting; and, just as importantly, he was subjected to the continual humiliation of being in a large hospital with a good reputation, treated like an infant, treated like a disease.
My mother was only allowed to see him during visiting hours, and she, too, was treated with routine dismissal, even though on a dozen occasions she found that he was being given the wrong medication or the wrong dosage. She ended up being a de facto private nurse, but the privileges that went with this position included only being allowed to give him suppositories; even though she begged the hospital to allow him to be released into her care so she could look after him at home, they refused, saying that untrained members of the public couldn’t be allowed to administer medication.
He eventually died in the hospital, alone. She, too, was alone, in a way. She had looked after him by herself, and his death left her carrying all his pain, his anger, his humiliation. It was too much to bear, but it was also too terrible to talk about, and it created a silent, dark divide between her and her children, whose grief was preempted by hers.
Fifteen years later, she, too, was told she had cancer, but instead of going into the hospital, she signed on with the local hospice. Her death was a completely different experience. She stayed at home in her flat with its sunny garden, surrounded by paintings she had painted and furniture she had carved, almost the entire time until she died. The medical personnel talked to her as an equal and saw her on our own turf; the whole family was involved, caring for her in shifts, constantly talking to her, to each other, making sense of what was going on, growing closer to her and to each other until it became clear that her death, though a tremendous loss, was a transaction involving gifts, too, that would enrich the rest of our lives.
THE HOSPICE ITSELF
Let’s clarify terms. While “a hospice” is usually a building, sometimes part of a hospital, sometimes a freestanding building with or without inpatient facilities of its own, “hospice” usually refers to the hospice movement in general and its attendant methods and philosophies concerning care for the terminally ill. To be “in hospice” doesn’t mean one is in the hospice building; it’s much more likely that one is “on service” (that is, receiving hospice care) at home.
There are five places a hospice patient might be at any given time.
• Ideally, at home, but this is possible only if the patient has a home and has family or neighbors able to give more or less continuous care.
• The acute-care center, if the hospice has one. This is for short-term medical treatment that can’t be done at home. (Of course, traditional thinking holds that nothing can be done at home, and the family is a bunch of meddling bumblers who, under no circumstances, should be put in charge of, say, morphine.) Most hospices deliberately have very few beds and try to send patients home after a couple of days, a week at most.
• Some other form of “managed-care facility” — in other words, a nursing home (or “convalescent hospital,” as they are now sometimes grandly styled) that has a contract with a hospice. Most often used when a patient has no family support and can’t live at home alone.
• A respite house, a stand-alone building specifically designed for the needs of the dying — that is to say, filled with light and flowers and music One respite house in Vermont runs the best children’s art program in the state, filling the place with life. A respite house fulfills the same needs as a managed-care facility, but usually much, much better.
• A hospital. Not for treatment, usually, but for respite. A number of hospices without inpatient beds have agreements with local hospitals that the patient can go in for a few days just to give the caregiver(s) a break.
Despite these various manifestations, the philosophy of every hospice is essentially the same: We will do everything we can to help you live what remains of your life as fully as possible. In its most clinical sense, this involves palliative medicine — that is, treatments aimed not to cure but to make life as comfortable as possible in the face of the old enemies, pain, nausea, vomiting, and constipation. In a broader sense, it involves taking care of the emotional and spiritual burdens that may be harder to bear than the physical pain. At this final stage of life, being separated from one’s dog or having unpaid bills may be more disturbing than simple pain.
At its most profound, hospice invites patients to turn their entire view of life around. Now that you know you have perhaps only a few months to live, why put off doing what you have always denied yourself? Why be afraid of other people’s opinions? Why carry that grudge against your sister? This approach not only transforms death, in some instances it transforms life, both of the dying and of those who are near them. For we are all, in effect, terminal; hospice encourages us to do what, if we’d had any sense, we’d have been doing all our lives.
SAN DIEGO HOSPICE
In a metaphysical sense, hospice exists wherever its patients live. In a postal sense, the San Diego Hospice consists of two linked buildings standing at the end of Third Avenue in Hillcrest, perched on the lip of Vauclain Point, overlooking Mission Valley. Across the ravine, the UCSD Medical Center juts up behind a fringe of trees, looking for all the world like a huge concrete waffle stood on end.
Even in a city of buildings competing for the attention of a roaming editor of Architectural Digest, the San Diego Hospice buildings are quietly remarkable — low, earth toned, looking somehow American, Japanese, and Mexican simultaneously, joined by two graceful arbors encircling a driveway in the middle of which is a single astonishing tree, a native of South Africa called a Naked Coral. Sinuous yet compact, it manages to look both startling and wise, as if the Tree of Life and the Tree of the Knowledge of Good and Evil had been interbred by a celestial gardener.
I’ve visited some half a dozen hospices, and the parking lot of the San Diego Hospice is bigger than any of them. Indoors, the buildings are furnished in what might be called the school of hospice art, transcendent but ecumenical: a fan-shaped soft sculpture in handmade paper, textured walls and carpets blending dove-gray and quiet blue, a sculpture of a dove, and a photograph of someone hang-gliding off a cliff, its symbolism lofty and hard to miss.
The hospice is considerably older than its headquarters. It was founded largely through the efforts of Dr. Doris Howell, a physician with an extraordinary pedigree in hospice. She is a friend of Cicely Saunders, founder (in 1967) of St. Christopher’s in London, the first modern-era hospice, and was also named to the board of the first U.S. hospice, founded in 1974 in New Haven by the dean of the Yale School of Nursing. She herself subsequently founded a children’s hospice in Philadelphia, though it did not survive when she left for the West Coast to become a professor of pediatrics at UCSD. She pooled her experience with members of Episcopal Community Services and other community figures, and the result, in 1977, was a small-budget, community-based home-care hospice run along the lines of a largely volunteer home health agency, as many hospices are still run today. One particularly lean year, she paid salaries out of her own pocket. The first physician hired, in 1978, was Dr. Laurel Herbst.
At the time, many in the medical establishment saw hospice as a grassroots community service that essentially acted out of charity and had little serious clinical significance — a professional dead end. Dr. Herbst found this out in the fall of 1978, at the second annual Scripps Memorial Hospital Cancer Symposium in San Diego, a national conference that is now a very big deal and was even then gathering momentum. Herbst, who had been at SDH only a few months, went to the conference to get continuing education credit for her medical license and to make contact, on behalf of the fledgling hospice, with her colleagues in the medical community.
As she expected, she knew a fair number of people at the conference from her training programs in Los Angeles and San Francisco, and they were delighted to see her after her nonmedical sabbatical in Colorado. “When I told them what I was doing, they would say, ‘Oh,’ and back away from me. It was so disturbing I actually had to leave the conference.”
When she went to the same conference the following year, people were a little more curious, asking, “Are you still with hospice?” The third year she went, the question became, “Are you still with hospice? Can I talk to you? We’re thinking of starting one in our town.” By the fourth year, she was finally being accepted as a colleague, and hospice as a viable field of work. “Let me talk to you about a case I had. What would you have done?”
SDH might have remained on this modest scale, but in the mid-1980s it was blessed with the kind of sudden, unexpected benefaction that every nonprofit organization dreams of. At the time, the organization employed perhaps two dozen people, but was modest enough to use Herbst as doctor and bookkeeper, because she was the only one who understood step-down accounting. Joan Kroc, widow of Ray Kroc (cofounder of McDonald’s, former owner of the San Diego Padres), was so impressed with hospice care her father received in Minnesota that she paid the bills — $18 million in all — for SDH to buy land, build buildings, furnish them, set up an inpatient facility, and be a teaching center for the philosophy and practice of hospice care. In December 1990 the home-care administration building was opened; the 24-bed acute-care and conference building followed in July 1991.
Any nonprofit that receives such massive one-time capitalization has to run hard to keep up with its good fortune, and it’s not surprising that soon afterward some 20 or 30 employees were laid off or that the administration (though not the medical staff) has seen a high turnover in the last four years. At the moment, the roughly 240 hospice employees work within an annual budget of some $12 million to serve about 220 patients (205 at home, 15 in the acute-care center), the whole census down from a peak of perhaps 250 last summer.
SDH operates in four teams, each of which oversees some 50 patients. Each team consists of nurses, social workers, home health aides (who visit two or three times a week to help with the patient’s personal care, grooming, bathing, shaving, fixing hair, and other services), homemakers (who visit weekly, doing light housekeeping, light cooking, and laundry), chaplains, and volunteers (who sit with the patient a minimum of three hours a week, offering respite for the primary caregiver to get out of the house to exercise, go shopping, or just have a break), plus a team director and a secretary for administrative support. All of them carry out the kind of paramedical functions that hospice is all about — chatting with the patient, bringing a cheery face into the home, passing the word if a clinical or spiritual visit seems to be needed.
This is, to put it mildly, an unusually well-staffed team; many hospices rely much more heavily on volunteers, and their smaller staffs find themselves spread far more thinly. Even in smaller hospices, though, this team approach, which also includes a hospice physician and the patient’s family and neighbors, changes altogether the alignment of medical power. The top-down hierarchy simply makes no sense when most of the clinical work will be done by a nurse and when the greatest amount of care in general comes from the patient’s family.
The hospice physicians, of which there are currently two full-time and several per diem, provide medical care in the acute-care center and also for home-care patients needing consultative conferences every other week. But the familiar power structure is completely altered in favor of a more egalitarian flavor, which many physicians find deeply disturbing. It’s as if they came upon the Empire State Building lying sideways along Fifth Avenue. From the patient’s point of view, though, the totalitarianism of the hospital is finally overthrown. Not only are they in their own homes, eating what they want, not being awakened at the crack of dawn to have their vital signs taken, but they and their families are respected as members of the healthcare team, for the simple reason that any other way doesn’t work.
All except the volunteers are paid; SDH is required by Medicare to provide all those services professionally. Medicare also requires that SDH provide bereavement services, though it doesn’t reimburse for them. Perhaps three-quarters of the SDH patients are covered by Medicare, which reimburses SDH about $102.33 per day; patients pay a 5 percent copayment for their pharmaceuticals used at home, and that’s it. Others are covered by MediCal, by insurance through their employers, or by an HMO; each plan has a different hospice benefit, but it’s usually comprehensive. A small category of people — the working poor, under 65 and either uninsured or underinsured — falls between these categories and has no means to pay. If they can, they pay out of pocket; if not, SDH may carry the cost. SDH may also have to make up the costs for those whose care is unreimbursed by Medicare or MediCal — a big category. “Last year we gave away three-quarters of a million dollars worth of care,” said Lisa Gaspard, the hospice’s public relations manager.
She walked me over to the acute-care center. Each wing has what is virtually an atrium, with cathedral windows. The rooms are more like a very expensive hotel than a hospital. Every room is private, with its own patio or balcony and a large private bathroom. The floors are half polished hardwood, half carpet, with a sofabed, television discreetly hidden in a cabinet, all the medical equipment similarly invisible. “We’ve hidden as much of the medical equipment as we can behind nice tumiture," Gaspard said, opening what looked like a liquor cabinet. “This is the dirty linen cart.” The bed can be wheeled outside, and the family is invited to stay, even to bring pets.
At the moment, of course, all the equipment and furnishings are virtually brand new. Maintaining them on Medicaid reimbursements of $100 a day will be the trick.
One or two features of the place leave me a little uncomfortable. Lisa shows me the therapy-dog scrapbook, page after page of snapshots of patients receiving visits from one of the hospice’s three therapy dogs, in every one a rottweiler or a retriever gamely wearing bunny ears or a clown hat or a pith helmet or a bandana and cowboy hat. “They have a different outfit every week.” The companionship of dogs is fine, but their therapeutic value doesn't depend on bunny ears. She also showed me the “library of donors,” in which SDH has taken the name-a-brick concept and replaced bricks with books. The baby grand piano in the “library” is real, but the “books” are essentially empty boxes with the donors’ names on the spines.
Such an artifice is a sign that the SDH administration, at least, is paddling like crazy in the troubled waters of modem health care. More than a dozen hospices have sprung up in San Diego since SDH was founded, and with such competition for market share, some bear precious little resemblance to the original foundations on either side of the Atlantic. Some are attached to specific HMOs, some to specific hospitals, some are even for profit.
“Everyone’s aligning into groups,” said Gaspard. “We don’t have a guaranteed base of referrals; however, we are contracting with insurance companies, hospital systems, and physician groups.”
The idea of a for-profit hospice makes my skin crawl. Any for-profit medical establishment has to jack its charges high enough to cover not only its medical expenses but also to spin dividends out to investors, not to mention the current fad for paying HMO CEOs anything from $1 million to $6 million a year. That has to come out of money that might be spent on the patient. And hospice, above all, was founded as a means of caring for people who are at their most vulnerable, not profiting from them.
MED ED ONE: LESS DRAMATIC BUT USEFUL
The development of hospice has always depended on its ability to educate and, to a lesser degree, to research. Until palliative care, in its broadest sense, was shown to work, conventional medicine could regard hospice as little more than a cross between a home health agency and a visit from the priest — which is, in fact, how many doctors still regard it — and comfortably ignore it, continuing to broadcast its own grim view of terminal illness and death. SDH had to take the education of future physicians into its own hands.
“After we built the building, which we did in the full view of the medical school over there, we finally got the attention of the university,” Herbst said. “We had had very little contact with them for years. We’d say, ‘Wouldn’t you like us to come help teach about pain management? About talking to dying patients? Doctor-patient relations?’ And in fact they did let me give a lecture every year to the first-year students on the art of discussing prognosis with a newly diagnosed terminally ill patient. But we really didn’t have their full and undivided attention until we put up a building, and all of a sudden it was much easier to get the idea across that we were different, that we had something else to offer, and over the last three and a half or four years we’ve developed a series of courses.” . San Diego Hospice is now one of the nation’s biggest hospice teaching programs for medical students and physicians in training, hosting perhaps 200 students a year. “The family practice residents are here a day a week for a month, and during that time they spend half their time in the acute-care center and half the time in home visits. And in the home visits they’re assigned a patient to go see who needs a doctor’s visit for some reason. They go with a hospice nurse, who helps them relate the hospice team issues. The geriatric fellows actually spend a whole month here, and we just negotiated a similar program for the internal medicine residents from Scripps Green Hospital.
“We have two nursing schools who send us students, and we have a couple different experiences for those students. Some just go on one-day home visits with a nurse and get to see what goes on in the nurse’s life and get to know just a little bit about palliative care. We also have nursing interns who come and actually do their internship time here (or externship, as they call them). They spend a month or six weeks acting in the capacity of a nurse, but with a supervisor.”
Well, yes, all right — but does a quick stop in the hospice sheep dip really affect the students, who are at all other times getting a total immersion baptism in traditional Western high-tech, high-pressure, high-stakes medicine?
“At the beginning of the ten-week elective for second-year students, we assign a home-care patient to them, and their requirement is to visit and talk to that patient at least once a week for the full ten weeks and get as much contact beyond that as they like — talk to the families, etc. At the end of the ten weeks, during which we’ve presented pain management, management of other symptoms, pediatrics, grief and bereavement, and ethics, we ask them to write a paper about their experience with the patient and relate it to what they’ve learned during the class. It’s fascinating reading. Fascinating. That helps us see who’s missing it. And nobody misses it.”
Later, she sent me some of the student manuscripts. Michael Miovic has written, “I came to hospice half expecting that I might meet face to face with the moment of death itself, that mysterious passage which seems all the more mysterious to me because I’ve never seen it at the bedside. What I came away with was something much less dramatic but more useful, an appreciation for life and a glimpse of the many quiet, hidden deaths that hover around us like angels of pain in life’s journey, ready to teach us if we consent. A number of things and experiences made an impression on me in this course, but none more than the way I carried hospice home with me.
“I am married, with a stepson aged 15, and I have noticed that the more I’ve thought about issues of death and dying, the more appreciative I’ve grown of the people in my life and the more loving I’ve become in my own quiet way. Especially I’ve noticed that I’ve started to grieve their deaths in advance, as it were, in moments here and there (most frequently as I drive home from hospice). As I imagine the deaths of my wife and son, their absence in my life, the reality and inevitability of loss sinks home a little deeper and I become more grateful for all the love and blessings I currently have.
“It occurs to me, too, that our loved ones are, in a sense, always dying to us. We form unspoken images of people in our minds, fix their natures and relations to us in certain ways, live in a gauze of dreams that only half describes the figure of the present and raises the future upon a foundation of shifting ether. Yet the full reality and destiny of those we love exceeds us, eludes our attempt to control the flow of life, and I have found that as I step back from my dreams and listen to their echo, the people I love are always dying unto me in the sense that I have no option but to let them go. Today they return, tomorrow they return, but I know that one day I will let the bird out to fly and it will not come back — or perhaps it returns with different feathers, a new color. And so, I have less urge to control, to impose my will and view of things; I treasure more the magic around me, the unknown side of wife and son, both the joy and pain that emerges unexpectedly when I have less stake in the outcome and more love for the gift of process....”
Somewhere in the Valhalla of medicine, Sir William Osier is punching the air, crying, “Yes! Yes!”
THE HOSPICE PATIENT
Ada and Edith Nichols live on Rancho Hills Drive in Paradise Hills, in one of the suburbs spread like butter on the earthen crust of the canyonlands above the Sweetwater River. It’s a heterogeneous neighborhood. In its front windows the nearest food market, Farm Direct, advertises pork feet, fresh blue crabs, jalapefto and serrano chilies, and milkfish. A battered ice cream van, most of its windows boarded up, tinkles and plonks through the quiet streets playing “The Entertainer Rag” and “Pop Goes the Weasel.” I am accompanied by Armando Garcia, one of SDH’s five social workers, slim, dark, neatly groomed, and nattily dressed in a dark blazer and pants.
Edith, who opens the door to us, has a pleasant, grandmotherly plumpness, wears a bright floral housedress, smiles, and talks readily. Ada, shorter and less erect, has a white thatch of hair and has safety-pinned a blue blanket like a shawl over her cotton house dress. Her ankles and feet are swollen into pads.
The tidy little living room sports large, bright, sentimental paintings of the Woolworth school, mostly landscapes. Armando and I sink into the maroon couch next to the piano, a well-worn Kingsbury that looks as if it came west from Abilene by wagon train. Ada and Edith pull up chairs and look at us expectantly.
Ada was born in Abilene, Kansas, Edith in Colorado; they moved to San Diego with their mother in 1928. Their mother lived into her 80s; their father, from whom she had separated, might have reached 100, Ada guesses.
At first, Edith does most of the talking for Ada. They first heard about hospice when someone at the hospital — Paradise Valley — recommended it. It seemed like a good idea, because the hospice would send someone over to take care of Ada’s nursing and personal hygiene. “I’m not a nurse,” Edith says, unembarrassed. “It’s not my cup of tea.” Ada says she didn’t pay much attention to the decision — probably, Armando chips in, because she was overmedicated at the time. In any event, hospice has been a blessing to both of them, they agree. “They’re real friendly and real polite,” Edith says. “They change her bandages and give her a bath.” Before hospice, Ada was left to take care of herself.
How does she feel about this phase of her life?
“It’s just like God wants it,” Ada says. “He can heal cancer as easily as he can heal anything else.”
This seems a little optimistic to me, but then again, it’s been nearly a year since she left the hospital.
“She’s a lot better than she was,” Edith says. “I think everybody lives one day at a time. Nobody knows what tomorrow will be.” This easygoing cheerfulness catches me off balance. I’ve simply never met anyone who seems less possessed by a fatal illness or has so simple and strong...what? Resolve? Protection? Buoyancy? Her comments also remind me of the research that Bernie Siegel quotes in Love, Medicine, and Miracles, suggesting that membership in a religious community correlates positively with longer life, fewer illnesses, swifter recovery. I find myself envying her.
The hospice chaplain calls ahead, then drops by every so often. “He describes world events,” Ada says affably, “leading up to the coming of Christ.”
Why does she prefer to be at home?
“Well, I can get up and go whenever I want to,” Ada says. “In the hospital you have to call someone to come and get you.” I think that maybe she’s simply talking about going to the bathroom, but I’ve underestimated her range of activities, as I will do time and again. Both sisters play the piano, which has Melodies of Praise and The Scribner Radio Music Library on its shelf. The hospital had a piano, Edith said, but you don’t feel as free to play it.
Then there’s Ada’s painting — Edith brings in a couple of oil paintings, a rural scene and a seascape, both a little blurred, but with a certain affection and energy — and her sewing. As a hobby, Edith says, they dress dolls. And give them to children?
I ask, uncomprehending. Sometimes we mean to, she explains, but when we get through dressing them, we wind up keeping them. Ada has already disappeared around the comer and now reappears with two sizable dolls, one in a satin dress and matching petticoat, one in red gingham — a little old-fashioned, but presentable enough. I should see Ada’s doll collection, Edith says. She has thousands.
Ada takes me around the house. In the “junk room” I catch a glimpse of a marimba and a large xylophone. Ada’s own room is a sunny extension, set up with the characteristic all-my-things-within-reach self-sufficiency of those who are no longer highly mobile. One little table is covered with neat boxes of ribbons and lace; another on the floor is full of spools of colored thread; patterns lie everywhere. The remaining space is taken up with dozens of family photographs, large and small, and several dolls. The commode stands beside the adjustable bed that the hospice provided. She kicks aside a cardboard box in her way, agile despite her swollen ankles, and leads me out to the back yard.
To the casual eye — mine, that is — the back yard is a bit of a mess, in keeping with the loose screens on the front door. The ground falls away gradually past a ramshackle chicken shed, then sharply into a ravine, on the opposite side of which are three rather untidy houses that look as if they need only one more decent shower to send them sliding down the small canyon and round the bend toward the Sweetwater.
But everything here has its surprises, its concealed life. A miscellaneous-looking piece of vegetation at the lip of the hill .is a mulberry tree; Desi and Kook, her niece and step-niece, take leaves into school for their silkworms to eat. On the left is a tangerine tree that I’d overlooked; it is unpruned and straggly but still has fruit. “The neighbor’s boy was up that tree at 2:30 in the morning,” Ada says. “If I’d had my shoes on. I’d have caught him, but I can’t run in my bare feet.” She reaches down and plucks at some straggling Bermuda grass. It’s been a day or two since she last did any weeding, she explains. “It helps me. I only work at it for an hour, an hour and a half maybe, and I’ve got it done.” The doll room, an overrun bedroom, is stunning. It has furniture, though it’s hard to see what. On every surface, laid out or piled up or collected into cardboard boxes, are dolls—big, small, old, pew, clad, naked. Gerbers, Barbies, Ideals, G.I. Joes, even an antique Effanbee Fluffy. At least half are in plastic bags “to keep the dirt off them.” Chuckling, Ada shows me an Army Barbie and Ken, still in their box, as is the Christie Brinkley “Real Model Coflection” doll and the African-American Costume Ball Barbie. The 1989 Holiday Barbie, Edith chimes in from the doorway, is now worth $400, though the fourth- and fifth-issue Barbies are probably more valuable. Here is the Canadian Barbie, and somewhere the English Barbie-equivalent, whose name neither sister can remember. As if to make up for this lapse, Ada shows me a boy doll in a Beefeater uniform with a threepence British stamp stuck to each of his sleeves. “That’s the prince,” she says, happily. "That’s the king of England.” Dolls are one of the three most frequently collected items in America, Edith tells Armando in the other room. Ada shows me another, a curly brunette. “This one’s been wigged,” she says, pulling off the wig to reveal a stubbled pink head. “We bought the booties. I don’t crochet.
“I started collecting them 20 or 30 years ago, because I had to have something to do,” she explains. “I can’t just sit down and twiddle my thumbs, so I started collecting.”
“Years ago I gave my son the G.L Joes,” Edith said. “Now I see them at antique auctions for $60 apiece. I paid $2.99. I wish I’d kept them now.”
By now Ada is on a roll and shows me what I take to be her only stamp album, and then another, much thicker one, packed with the glorious particularity of philatelic history; the 1929 Sullivan Expedition commemorative issue, the 1928 Aeronautics Conference, the 1929 Battle of Fallen Timbers, way back to an 1861 George Washington.
“They’re putting out Marilyn Monroe,” Edith says. “I want to get her. I don’t care about Elvis Presley.”
Now Ada is pulling out box after box of loose stamps, stamps in plastic sleeves, stamps in presentation booklets, postcards, first-day covers only a few months old, mailed in Huntsville, Alabama, by one of two stamp services she subscribes to. “When she was in the hospital, I paid ’em off,” Edith said. “I said, ‘Don’t send me any more.’ But they’re still sending them.”
What hospital would let her play the piano whenever and however she wanted? What nursing home would give her an entire room for her dolls? What establishment of any kind would allow her to live with Edith, who no longer drives and would effectively be separated from Ada almost all the time? It’s impossible to imagine one without the other, their voices calling from room to room like birds. These restrictions are more profound than they may seem. Any action is an act of knitting, raveling the past with the present to create the future, making things that will exist, that will have consequences, that will still be there to be given away or shown off like dolls.
Think of the purposelessness of the hospital and the nursing home. Inaction, the stricture of a sterile environment, severs the connection through time and thus suspends life, as if death had soaked like a beetroot stain backwards through time and saturated the fabric of life still left. It’s not just a matter of having things to look forward to or even things to do with our hands to keep our minds off our infirmities, it’s that what we make today we can admire, or refinish, or give away, tomorrow. Today’s work is tomorrow’s surroundings. If what we did yesterday was meaningless, how does that help us when we wake up today? What does it leave us? The smallest acts create continuous discovery; even the Bermuda grass and the neighbor’s boy add their own variety.
Seeing Ada’s life unfolding, room by surprising room, I felt straightened up, as if someone had slapped me hard across my assumptions and left me blinking and alert. Whatever we, on the outside, think of someone else’s life is almost always wrong—and that becomes more and more true as a person approaches death. We make death, the unknowable, into the dark screen onto which we project our worst fears; and then we judge the experience of the dying accordingly. The patient’s weakening voice is easily drowned out by the hysterical clamor of our own selfish helplessness and horror, sometimes literally, like the Mexican woman I was told about who was in the ICU time and again and eventually told the physician that next time she didn’t want to be resuscitated, she wanted to be allowed to die in peace. But when her next cardiac episode struck, her family insisted she be rushed into the hospital, insisted she be revived; and because the first step of resuscitation involves intubation, the woman was silenced and died with a tube down her throat.
This is the heart of it all, the crux. Nobody asks, “What is the experience of the dying? What do they want?” And they themselves become steadily less and less able to tell us, until they reach the absolute truth and fall silent. If there’s one thing we can be certain about death, it’s that it’s not what we think it is.
Before we leave, Edith produces her masterpiece, a black doll in shades and a gold lame suit. “Do you know anything about rock and roll?’’ she asks. “A little," I say, buying time, thinking Stevie Wonder? No. Ray Charles? Surely not. “Hammer," she says. “I paid $19 for him. He’ll be worth a lot one day. His glasses come off.”
LIVING AND DYING
Is Ada dying? It’s an absurd question. She is living, clearly, if she is also dying, so are we all. The hospice philosophy tends to see things in terms of life or death, but not in terms of dying. It’s an existential approach. If I wake up tomorrow, I’ll make the most of what energy I have — a crucial mental shift from negative to positive. I was about to write “especially for cancer patients, who tend to have patches of energy alternating with patches of fatigue," but then I realized what I’ve realized time and again in studying hospice. We all go through patches of energy and tiredness, though for differing reasons and to differing degrees, and what hospice teaches us about caring for the terminally ill applies in every single respect to caring for ourselves, the healthy, who are also terminal, though we lack a prognosis.
Most of the time when we use the word “dying," we do so to convey a sense of urgency or perhaps self-pity, it’s not a condition but a drama.
I can think of two ways in which “dying” might have meaning: a hard, outer one and a soft, inner one, like the shell and the oyster. Hospice staff speak of a phase of “active dying,” which is markedly different from everything that has gone on before, even a day or so before. Quite suddenly, the patient’s biosystems begin to shut down. Breathing and pulse become shallower and erratic, blood pressure drops, secretions build up in the throat, which the patient no longer has the ability (or want? or need?) to clear, causing a rattling sound, the mouth falls slack, blinking slows, the facial muscles relax, making the patient Iook peaceful, younger.
On its own, this would simply be Sherwin Nuland biodata, the perceived changes reported in the official language without curiosity, but colloquially everyone will admit the mystery at the core. Nobody knows why these changes suddenly kick in. The principal truth about death, even on this moment-by-moment scale, is that nobody knows when it will happen. Hence the second meaning of “dying,” the open secret, immune to calibration, but seen time and time again: that we choose when to die or, in the hospice phrase, to let go.
In many cases it’s hard to argue that someone has chosen to die, but perhaps that’s because they refused to let go and fought the changes in their bodies until their last breath. In other cases it seems perfectly transparent. “A new AIDS patient came in,” Kathy Ferdinandson said, “with herpetic lesions from head to toe, and I thought, ‘My God, how am I going to give this guy comfort?’ That was our immediate goal, and we also knew that his mother’s greatest grief would be for him to die in agony. We managed to get a morphine pump, we got some pain control, some wound care, we got him a different bed and mattress that wasn’t so painful to lie on, we taught the family how to turn him over so he didn’t scream with agony. Eventually one day he turned to his mother and said, ‘Mom, I’m comfortable. I’m ready to go now.’ And he died the next day.”
There’s perhaps one more meaning of “dying” that we use colloquially, meaning no longer engaged in living, living in body only, living without spirit. What do we give up when, in the name of staying alive, we agree to go to a hospital or nursing home? The conventional answer these days is “control,” and you’ll hear not only hospice staff but those in mainstream medicine starting to concede that the patient does better when he or she feels more in control. It’s more than that, though. If we leave hflme, we sever virtually all our connections with the normal processes of life that, no matter how apparently trivial, are vital. We opt for dying, of a kind.
LIKE GOD WANTS IT
The following day, something Ada had said still puzzled me: It’s just like God wants it. He can heal cancer as easily as he can heal anything else.
Was this faith or denial? She didn’t exactly seem to be in denial about her illness — I don’t think she meant “I’m going to get better” — but this raised the whole notion of an interventionist God, and prayer as a call for intervention, and disease as a sign of lack of faith.
To me, from my position as a wistful atheist, faith had always seemed to be something helpful and supportive, not only in life in general, but in giving the individual’s immune system (or spirit, depending on whom you’re asking) an extra boost in resisting infection or recovering from illness. Now it became clear that it could quite possibly be an additional burden.
I asked Geoff Copland, who is one of San Diego Hospice’s four chaplains, about this tricky theological issue. (Not every patient asks to see a hospice chaplain, but even so, spiritual support is regarded as one of the main thrusts of hospice care. For some patients, it may mean simply lending a sympathetic ear; for others, it may mean helping them discover sources of strength or coming to an understanding of both death and life; for others, it may involve an orthodox religious relationship. Virtually all hospice chaplains become adept at wearing a variety of hats or appearing to wear no hat at all.)
To some of the Pentecostal groups, Geoff said, a major illness would be a sign not of simple bad luck, overwork, or God testing one’s faith, but of the activity of Satan. What’s more, other members of the congregation might see the cancer as a sign of sin. He quoted me John 9, in which the disciples ask if the man blind from birth is being punished for the sins of his parents. Jesus doesn’t exactly help matters by saying no, he’s blind in order to show the glory of God, which He then demonstrates by curing him. This leaves the moral and spiritual status of other blind-since-birthers who didn’t happen to be cured by Jesus rather undecided.
In either case, this interpretation of disease-as-lack-of-faith would add to the impact of the illness, not help the patient deal with it (though it must be said that Ada and Edith seemed to be quite happy with their own faith), and leaves open not only the constant possibility of blaming the victim, especially, for example, AIDS patients. I shuddered.
The question hit close to home, Geoff said. His own son was born with bones missing in his arms and unusable thumbs; he has had a series of operations.
This dark question came up again when I went to visit a second hospice patient, Charles Bess, who has been a member of the Greater Apostolic Faith Temple Church for six decades, serving as deacon and Sunday school teacher. Armando was again acting as my guide.
“We’re going to Logan Heights. They don’t like white boys out there. That okay with you?” I assumed he was joking, but then I’m an easy mark. Vermont, where I live, is the whitest state in the union, and I’m an easy prey to racial fears. “We’re goin’ to Barrio Logan,” he told his team’s administrative assistant, winking. “Park close behind me,” he told me. With difficulty, I followed his BMW 733i down to the far end of Imperial Avenue, where he parked and fitted the steering wheel lock. “This is where I grew up.”
Charles Bess was sitting on a tubular aluminum lawn chair outside his house when we arrived, enjoying the warm January sun. He was wearing a ragg sweater, flecked with black, white, and gray, black pants, black socks, black loafers. He looked about 70. He is 97.
He took us into his neat little house, with its family photos, copies of let and Ebony on the marble-topped coffee table, next to a pamphlet from the Truth Apostolic Community Church. On the walls, plaques from his church thanked him and both his late wives for their leadership and service, and a remarkably touching painting depicted a bespectacled, middle-aged black man sitting by a front stoop reading to half a dozen small black children, who listened with rapt attention.
He came to San Diego in 1920 from Hawaii. He worked in Ocean Beach in an oil mill, raking oil seeds into a chute that loaded the freight cars, then moved to San Diego proper, and over the years worked as a janitor, in construction, as the “steam man” in a furniture plant, stoking the furnaces to keep the glue hot. In Hawaii he learned to play the guitar, the ukelele, the steel guitar, the piano, and his instrument of choice, the sax. But for an injury to his left thumb, he’d still be playing all of them, and he still liked to thump out tunes on the piano with his right hand. He married twice; both wives died, the second three and a half years ago. He had a son, three daughters, and “a whole heap of grandchildren.
“I feel healthy. I’ve been healthy all my life, so far. Just of late I’ve had this little heart congestion.”
He’s been on service for four months, at the recommendation of his doctor. “She didn’t tell me I had no congested heart failure. I just woke up in the middle of the night, 2:00 a.m., and I felt restless, and I didn’t know what to do. So I called my daughter, and she took me to the hospital, and they said I’d had heart failure in the middle of the night. Fluid was building up. They told me if I’d waited a little longer I’d have had a heart attack.... I noticed my legs begin to swell, so I’m taking water tablets — they keep you urinating pretty good. And I was beginning to wheeze a little. I thought I was getting a cold.”
“Why did the doctor recommend hospice?” I asked.
“I have no idea,” he said, surprised, as if this was the first time the question had occurred to him.
“So he can be independent, pain-free, and comfortable,” Armando chipped in. The nurse comes once a week to check him over, a homemaker comes once a week to clean and tidy, and Armando drops in when he’s in the neighborhood. “They’re very attentive. Nice people. I have no complaints,” Charles said.
As if to illustrate the hospice services, Colleen, a ten-year veteran hospice homemaker, arrives, makes herself busy, keeps out of the way. When I go to talk to her, she says she likes meeting different people, lets the hospice team know if someone seems to need a visit from the nurse, the social worker, the chaplain. She doesn’t seek the patients out for conversation, but sometimes they come over and talk to her while she works. She used to work for another housecleaning company; she likes working for hospice because they gave her a good training, likes being part of the team.
Charles Bess clearly had no plans to die in the immediate future. “I’ll shoot for a hundred. There’s no telling how long God will allow you to live. He has the last say.” (“Amen to that,” Armando added.) “He blesses you and keeps you and strengthens you, and you’re grateful for it. It don’t have nothing to do with anything you do for yourself. He’s the one who’s keeping you and encouraging you and strengthening you.”
I had no problem with that; so far, he was describing exactly the kind of spiritual, emotional, and physical sustenance that might not be measurable but is almost universally recognized in an anecdotal way. The clinical value of membership in any supportive community is now generally accepted, and Bess is a remarkably active member of the church community, going every Wednesday night, every Friday night, and then “pretty much all day Sunday.” He sits in on the Sunday school until about 10:30 a.m., though he no longer teaches, then attends “regular service” from 11:00 a.m. until 3:30 or 4:00 p.m., the church serves a full meal, “and then I’m back again from 7:00 until 10:00 or 10:30.”
Who could begrudge him his faith, the sustenance of his community? But my easy liberal tolerance is not reciprocated. “When you die in Christ, you can die with a smile on your face because you know you're going to die with Him.” He quotes Ephesians, “You have to have Christ in your life, and if you’re anchored in Christ you have no fear.” But if you don’t, he makes it clear to me, then you’re going to the pit.
But what about those who develop cancer at 70, or 50, I ask him. He looks at me hard. “The Bible says, Tf you believe in the word of God, it will make you whole,’ ” he said sternly. “Christ said that if we had faith the size of a mustard seed — and that’s a pretty small seed — it will help you move mountains.”
He didn’t go on to say that the weak are therefore weak in faith, but the implication was clear, especially as he went on to say that virtuous people who lack faith in Christ — my mother, for example — were unquestionably damned. I thought of the man blind since birth, the chaplain’s son — but by now he was asking me what my own faith was, and when I told him truthfully, if evasively, that I was baptized in the Church of England, this was clearly not a satisfactory answer. How was I baptized? In whose name? He was telling me forcefully, with the vigor of a man grown suddenly young and strong, about his own conversion during the depression, when he was rapidly becoming an unemployed musician, and about the people in his congregation who are filled with the Holy Ghost and speak an unintelligible language that is straight from Christ, when Armando finally got off the phone and we took our leave.
Hospice in the U.S. bears the unmistakable stamp of Elizabeth Kiibler-Ross — her medical humanism, her psychiatric observations of the stages of dying, her Swiss neutrality, and subsequently her religion-free curiosity about near-death experiences. As a movement, then, hospice has been in a cleft stick, promising spiritual support without ever seeming to be sure what spiritual support actually was. The National Hospice Organization had been in existence for ten full years before it convened a conference to discuss spirituality in hospice care, and it has still come to no kind of consensus. If hospice has a bible, it is the Tibetan Book of the Dead. Nothing I’ve ever heard at hospice conferences or read in hospice books says anything about what to do if your patient, his family, and his community believe that cancer is sent by Satan.
What was suddenly becoming stunningly clear to me was that in National City or Chula Vista or El Cajon or Logan Heights, this graceful new-age ecumenical dance was simply not going to cut it. Talk about preparing for death — all the time modern medicine
was going further and further in encouraging us to follow our natural disposition to avoid thinking about death, older and more authoritative forces had never abandoned the subject, had never let up. It had been perfectly clear to them for 100 years, or 200, or 2000, how to die with a smile on one’s face, and they didn’t need hospice chaplains or social workers, and some of them didn’t even need doctors to tell them what life and death were all about. And in a weird way, that’s fair enough, because if medicine and science want to focus only on treating the living, and the dying are in God’s hands, then who can blame us, especially those of us who have the foresight to consider our mortal ends ahead of time, for turning away from medicine and science and seeking the strange and powerful disciplines that are enacted in God’s name?
San Diego Hospice seems to be defying the national demographics, which suggest that hospice is used predominantly by the white, educated middle class, who are likely to have some spiritual convictions but not to be overpoweringly religious. It suddenly strikes me that the reason why it diverges from these trends, and the reason why I’m so uncomfortable under Charles Bess’s interrogation, is because it is successful. SDH has set out to serve the community, that conveniently undefined body of Americans so bekived in theory by liberals, and has produced, in President Clinton’s words, a patient body that looks like America. What happens when the patient doesn’t want your spiritual ecumenism? What happens when that very liberality makes you, in his eyes, eternally damned? You go in and dust the pictures. Launder the tablecloth. Vacuum the rug.
When I stopped at the light outside Bruno’s Market, just down the block, mine was the only Anglo face in sight.
A CONVERSION EXPERIENCE
One of the oddest features of hospice is that, far from being a depressing or morbid occupation staffed exclusively by saints or people of extraordinarily tough backbone, it seems to give back even more than it demands. Virtually everyone in hospice looks five to ten years younger than they really are, and it suffers an amazingly low burnout rate among volunteers, who work at the emotional coal-face as much as any paid staffers. This is perhaps the crux of the matter; by being such a vivid and potent experience, death forces us into emotional states we usually avoid. These states, like all crises, offer as much opportunity as threat. We can recoil from them, we can close down, we can shove others away from us — all these are common responses to death. We can also, often for the first time, accept help, admit weakness, recognize generosity and gratitude. This is a stunning transformation; it’s like a glimpse of an entirely new dimension. It not only helps us to accept death, it changes our whole view of life.
Kathy Ferdinandson worked for nine years in emergency room medicine before changing to hospice, where she has now worked for two. The day she decided to quit ER work came at a time when she had begun working for San Diego Hospice but was still working on a per diem basis at the Alvarado Hospital emergency room. One Friday she worked all day at the hospice, then went over to Alvarado to work the night shift. It was a very busy night. At one point, she was due to take the next ambulance run. When the ambulance came in, it was delivering an SDH patient.
“At the last moment, the family had freaked out and told the EMTs to go to the ER rather than the acute-care center" at the hospice, she says. “This was, in my feeling, divine intervention.” The patient was comatose, actively dying. “In the next bed a drunk was swearing obscenities, in another bed a baby with an earache was screaming bloody murder, bells were ringing, beepers were going off — it was crazy.” The family was distraught with grief and guilt, crying, “Why did we do this?” The ER doctor ordered x-rays, 02, lab work, even though the family had asked for their mother not to be resuscitated. Kathy took the doctor aside and told him, “Look. This is a hospice patient. The family has asked that she not be resuscitated. Please, please let me take her upstairs where we can find somewhere quiet for her to die in peace.”
The doctor agreed and signed the order. Kathy went back to the family. “Your mother is dying,” she told them. “I’m going to bring her upstairs. Please go with her. Talk to her. She can hear you.” When a room was found for her upstairs, the family gathered around her and prayed. The other nurses took over Kathy’s patient load — glad, she believes, that she had relieved them of such an emotionally difficult and volatile encounter.
Kathy barely had time to go downstairs to thank her colleagues for relieving her, when another nurse found her and told her that the mother had died. She rejoined the family, who sang the mother’s favorite songs and prayed. “It was the next best thing to being in the acute-care center [at the hospiceJ or at home. They thanked me over and over.
“When I came back downstairs, and I must have been with the family for nearly three hours from the moment when they came in, I knew that I was no longer focused on patch-’em-up, move-’em-out, we-need-this-bed. (A hospital staff] may think they’re treating a patient holistically, but they don’t. They talk about people as ‘the ankle in three, the broken arm in five, the earache in four.’ I can’t be that kind of nurse anymore.”
Her first hospice patient was Joe Wehlage. Joe and Mary Wehlage and their children moved to San Diego in 1948; Joe was in the Navy and had been assigned to train recruits. He finished his 20 years in the Navy in 1957, went to work for San Diego Gas and Electric for 23 years, and retired in 1980. In the fall of 1992, Joe, then in his mid-70s, began feeling back pains and protracted fatigue. Over the next few months his shoulder began hurting too. A rheumatologist, who apparently failed to take x-rays, dismissed the pain as bursitis, but by the following March, when Joe found blood in his urine, a bone scan revealed his entire skeletal system was cancerous. “There were hot spots throughout, and the whole shoulder area was deteriorated to the point where bone was just missing,” Mary said. (The rest of this narrative is her own.) “What was there was porous, just gone. His whole skeletal system was involved, and obviously some of the major organs, though at that time we weren’t told that. When the diagnosis finally came, it was, ‘This is terminal, and you probably have maybe three to six months to live.’
“Our primary-care doctor called. He waited till the end of his office hours, so he could really talk. I have nothing but the highest regard and affection for this man. He felt so badly about it, to have to tell us, and he said, ‘No wonder Joe doesn’t feel well — bone pain is just about the worst kind of pain there is, and when his whole body is affected, there is not a spot that is going to be pain-free.’ He said, ‘You had better get ahold of hospice, because you are really going to need them.’ I had heard the word — I knew they had a new building up there — but I didn’t really know anything at all about hospice. “We were terrified, just terrified. I mean, we hadn’t ever thought...you don’t think...you feel, you know, that someday one of you will die before the other, but to say, ‘Okay, this is it.’ Then you wonder if the doctor said six months to give you hope, but really meant three months. The impossible thing to take in was that by the end of the year, Joe was not going to be there.
“By that time the doctor put him on morphine medicines, which immediately affected his mental processes. One time when I had given him the medicine, he was sitting on the edge of his bed. He had a digital clock that would Hash, and he was sitting there just mesmerized by that clock and watching those numbers flash and rambling on about the stock market and train schedules. I was terrified all over again, because I couldn’t get through to him. He was just gone from me. He did have some lucid time after that — not a lot, but some where we could really sit down and talk and discuss things in the past and settle affairs that needed to be settled then.”
“Settling one’s affairs” is virtually a cliche, but it goes right to the heart of the distinction that hospice draws between pain and suffering. For many hospice patients, the physical pain is not their most pressing concern; they may be far more concerned about the personal matters that they won’t be able to take care of. Who will handle the family finances? Who will look after the kids? Anything that has emotional value — the dog, the guilty secret, the unspoken love, the unconfessed crime, even the unweeded garden — involves a departure that may gnaw at the dying person more persistently and painfully than any disease.
“Joe had always handled the money. I was so afraid of making a mistake that I about wore out the calculator the first couple of months, checking and rechecking every little detail and making sure that I hadn’t forgotten to pay any of the bills. Joe had a lot of credit cards and agreed now that they had better be canceled. By this time he was having trouble using the touch-tone phone, so we decided that I’d make the necessary calls. In this one instance — Citibank, I think — there was an 800 number to call, so I called it and said we don’t want to renew the card. ‘Who’s speaking?’ ‘It’s Mrs. Wehlage speaking.’ ‘Well, the account’s not in your name.’ ‘Yeah, I’m aware of that, but my husband is terminally ill, and we want to close this account.’ They said, ‘Well, you can’t do it, he will have to do it.’
“By that time he couldn’t manage the phone or balance the checkbook — there was something mentally deteriorating. For someone who had been so good at all that type of thing to not be able to really do it anymore was so frustrating and embarrassing. So I got the number for him, and I got whoever they said he had to speak to. By now his hearing wasn’t so good, and he didn’t understand what they had said, and he asked them to repeat it. Apparently whoever was on the other end was really rude, because Joe lost his temper, which was unusual for him in a situation like that. They wanted to know his mother’s maiden name. I knew his mother’s maiden name. I could have given them the information that they needed to close the account.”
Mary’s nephew called San Diego Hospice, and after an initial assessment, Kathy Ferdinandson went out to the Wehlages’ house.
“She just epitomizes what hospice is all about,” Mary said. “She was interested in Joe and both of us as individuals and as a couple. She was extremely sorry that she had to meet us under these circumstances, but that was her job. I was, like, ‘This is too good to be true.’ But as time went on.... Her immediate priority was to get Joe pain-free so that whatever time was left could be quality time. And she tried valiantly with ever-increasing doses of medication and changes of medication. She was in constant touch with our doctor downtown. She was supposed to come twice a week, but all I had to do was call, and she would come and stay as long as we needed her. I just can’t say enough about Kathy.
“One day Kathy said to me, ‘Are you eating?’ I thought, ‘Oh.’ She said, ‘Sit down here. Get a Coke. Now tell me what you’ve had to eat today.’ ‘Well, not much.’ She said, ‘You have to take care of yourself, because if you don’t, you’re not going to be able to take care of Joe.’ She’s young enough to be my daughter, but she would sort of reverse the roles and be like my big sister. She is a lot taller and bigger. When Kathy hugged me, I said, ‘I just was hugged by a grizzly bear.’ ”
In June one of Joe’s deteriorating shoulder bones broke with an audible snap as he was getting up from his wheelchair. “From then on, he didn’t believe any talk about the possibility of quality time. He expected that more bones would break and that all he could look forward to was worse and worse pain. He went into an emotional tailspin. Kathy was so concerned about him that she insisted I remove all of the medication from the dresser in his room, because she was afraid that he’d overdose himself out of desperation.
“She said, ‘You go on out in the kitchen or the living room or something, because Joe and I are going to talk.’ And what they did was just have a knockdown battle back there. But she had forgotten that I had a nursery monitor that I kept out here so that I could hear everything in case he needed me or wanted anything. I couldn’t really distinguish the words, but I could hear there was all this awful commotion going on. I think he gave up at that time. It just wasn’t a battle worth fighting. Which I guess it wasn’t. But Kathy tried, she tried and tried and tried to get on top of the pain, but we never did actually totally get on top of the pain, and his condition physically as well as emotionally and mentally just deteriorated steadily after that.
“Kathy kept saying,‘‘You cannot do this by yourself.’ I said, ‘I am not going to have a stranger in this house.’ She said, ‘Well, you cannot do it by yourself.’ But then someplace along in there, my sister and brother-in-law just came and moved in with us; and my brother-in-law helped me with the nursing, and my sister just took over the cooking and the housework. I was so fortunate that they would just drop their own lives and stay with us for two months. Joe’s situation really brought our family together and strengthened and established on new levels the bonds between all of us.
“I felt totally supported — by my family members, by the whole hospice organization — whereas if we had been dealing still with the doctor and in a hospital situation. I’d have been shut out, I couldn’t have been there all of the time. I was just grateful that we could keep him home for mostly all of the time.”
Joe died on July 21. “At the end, even the morphine pump just didn’t do it. His pain was worse and worse and worse, and I thought, 'This is it. Just order an ambulance and get him up to the acute-care center, please,’ which they did. It took probably 8 to 10 hours to really get him comfortable there. But for those last 24 hours of his life, at least, he was totally comfortable. My daughter and I stayed right there in the room with him, so we know that he was peaceful and comfortable when he died, and the people who loved him were there with him. When he died, he suddenly looked at least 10 years younger, maybe 20 years younger. My last recollection of him is that he looked young and happy and peaceful and contented and pain-free.”
SDH helped Mary arrange the cremation and burial — Joe’s ashes were scattered at sea by the Navy —and the host of other infuriating and time-consuming administrative details that accompany a death. After the funeral, Mary began, rather unwillingly, to attend the support group meetings twice a month in the home-care building with 10 to 20 other survivors. “I wasn’t going to go, because I had been a very private person, and I thought you just don’t go doing your crying and reminiscing and whatnot with a bunch of strangers. But Kathy encouraged me to go, and my sister insisted that we go. She said she would go with me.
“The first few times I don’t think I had very much to say, but I was glad afterwards that I had gone. You can feel the support all around you, and you don’t have to speak if you don’t want to. I never took my dark glasses off for the first several weeks. I wasn’t aware of that until later when Patty Clement remarked that it was the first time she’d seen my eyes. I have not missed a bereavement group meeting since I first went in August of 1993, and now I am a volunteer in the bereavement department.
“Kathy had asked me if I had given any thought to what I was going to do afterwards. I thought she meant what we were going to do about services and so on, but I think, looking back, she meant, ‘What was I going to do afterwards, as time went on?’ From the first time I ever met her, I knew that eventually I wanted to be a hospice volunteer.”
Like most hospices, SDH won’t allow anyone to become a volunteer until at least a year after a bereavement. The likelihood of mistaking one’s own grief for someone else’s is simply too strong. After waiting her year and undergoing training with Judy Davis and Patti Clement, Mary made her first support visit in January.
“I went to see a lady whose husband had died in November. She doesn’t really want to come to the group meetings and feels alone — which she is, so she’s entitled to feel alone. She’s a military widow, so we had that to talk about. She has three adult children, and so do I; plus, we both have cats. The rapport was there. It was great. I had been very apprehensive, because she was my first contact. What if I said all the wrong things and just tore this lady apart? But I feel much more confident now. Patty said, ‘Trust your intuitions. Just keep your mouth shut and trust your intuitions.’ ”
Hospice has taught her how to grieve and how to begin to remake her life.
“The medical attitudes [in the hospice] are just unbelievable. Everybody cares so much, and you can just feel there is an aura of love and caring in the whole establishment. I love to go up there and just stay and wander around on the grounds and sit and look at the view or whatever. To me it’s a healing place to be.” Every morning she walks down by Mission Bay, where on Saturdays she often sees the hospice group. “I cherish my time down there by myself. There are no phones. I like it when I meet somebody to visit with for a few minutes, but if I just want to look at the bay, and the birds, and the trees and think my own thoughts, that’s fine.”
RECRUITING THE FAMILY
Armando emerges from one of the rooms in the acute-care building, where one of his patients is actively dying. The building is quiet and full of light; outside the windows, leaves dance in the slight breeze. The dying man is calm, he tells me.
“ ‘Brother Joe, it looks like this is okay,’ I said to him. ‘It looks like you’re peaceful.’ And he nodded, like this. Physically he is diminishing, he is dying. However, beyond that, there is a peace, both of acceptance and of resignation.” (Resignation, I think, is not a quality much encouraged in young Americans, especially men.) “I sense no anguish from him,” Armando continues, “and therefore he evokes no anguish in me.”
Social workers are a crucial part of the geometry of hospice care, which instead of being hierarchical (doctor at the pinnacle, nurse somewhere beneath, patient on the bottom, patient’s family largely of nuisance value) is strikingly egalitarian. A terminally ill patient needs frequent, perhaps even constant care, though not all of it is care that needs professionally certified clinical skills. Meanwhile, the closure of a life is a time that cries out for reconciliation and summation. Nobody wants to die alone or with unfinished business. (The bitterest cry of Hamlet’s father’s ghost is that he was “cut off even in the blossoms of my sin, / Unhous’led, disappointed, unanel’d, / No reck’ning made, but sent to my account / With all my imperfections on my head.”) For both practical and personal purposes, then, it makes sense to draw the family together as a rapidly trained home health team, and this connecting of the points is the social worker’s job — a job that is often very difficult.
“If it’s a — let’s not say a pathological family, but a troubled family, then death will stir the pot,” Armando explains. “A lot of unresolved issues — whoosh!— will come up from 20 years back, 30 years back, 40 years back. They’ll come up, they’ll become very vivid, and both the dying and the living realize that something is ending, and it’s either going to end right, with peace, or it’s going to be unresolved, with anguish.”
Recruiting the family as caregivers brings up an entire history. The whole family tree is suddenly laid out between them like an embroidered tablecloth. Some may refuse to help out of ancient I’ll-never-forgive-you-for-what-you-said-to-Mom resentments; some, more obliquely, may simply be terrified of death. The wife of one of Armando’s patients refused her husband Paul’s wish to die in his own bed, because her own grandmother had died at home in the days before palliative care, and it had been a painful and troubling death. Three days before he died, she suddenly changed her mind. “You got me thinking about what Paul wants,” she told Armando. “I held her and said. Thank you. You’ve made everybody very happy.’ And she said, ‘I know.’ ”
One of Joe’s sons is in jail, but his wife, daughter, and other son are with him — quite an achievement, as his successful microbiologist son grew up bearing a bitter grudge against his father for spanking him long and hard for shooting ball bearings with a slingshot at a movie screen.
“His father was a good provider, a good teacher, a good companion in a lot of other ways," Armando explained, “but the son wouldn’t see that. So I took this strapping man and this fragile, now-diseased father, and I said to the father, ‘Would it be too much to ask Robert to forgive you? I know that he’s a man now, he’s grown bigger than both of us, but that little child in him is still injured and thinks that your insensitivity caused that great pain.’ And he did. The father said, ‘Can you forgive me, son, for causing you that pain?’ and the son choked up, and he just hugged him. It was beautiful. There were a lot of tears.”
In effecting such a reconciliation, hospice is changing the meaning of death and establishing a new family legacy concerning how to handle the frail and the dying. Perhaps the next generation won’t be so scared of death; perhaps they’ll see it as a time of opportunity, even, to heal old wounds. Many of the benefits of what we do, an English hospice physician told me, won’t be seen for another 20 years or more.
The four hardest deaths Armando’s seen were all of men who were very intelligent but very contentious and who refused to accept that they were dying. We often praise such people as “fighters,” but in refusing to accept death they also refuse to accept that “they can go hard or they can go peacefully” — that is, they can help create the circumstances and the experience of their own dying. While hospice can’t guarantee every patient a painless and peaceful last few weeks or months, refusing to admit the approach of death does little but harm.
Armando’s beat is the South Bay, and he seems to be the right person for the job, having grown up in the racial and cultural mix of Barrio Logan, in those straitened circumstances, that social fringe. He describes himself proudly as bilingual and bicultural. He’s worked with gangs, geriatrics, and mental patients; currently at SDH he has a caseload of 25,24 after Brother Joe leaves.
Many of his most delicate cases involve cultures — Hispanic, Asian — in which it is absolutely taboo to discuss death or even serious illness, especially with the patient. “They want [hospice’s) help — they want the nursing, they want the visits, they want the expertise — but they don’t want to be upfront with the patient. I’ve broken some barriers. I’ve taken the head of the household aside, and I’ve said, ‘Let’s say it was you.’ ‘Well, that would be different.’ 'What makes you say that?’ I make them think, at the very least.” How he approaches them depends on the degree of acculturation and assimilation. “If, for example, I see it’s a third-generation Mexican-American family I’d approach the topic of death and dying and disease a lot more freely than if they were one generation removed.
“I haven’t found any group I couldn’t work with, so far — Hmong, Vietnamese, Indians, Cambodians, African-Americans, all kinds of Latinos — Nicaraguetises, Colombianos, but that’s easier than Indochinese, because the language is the same and the cultures are similar. I think that if you come in with respect, they’ll pick it up. No matter how much they lack sophistication or education, they’ll still pick up your intentions.”
Dr. Mary Margaret Loehr echoed this difficulty. One of her hospice patients was from Thailand and spoke no English, and she had no idea whether to tell him about his condition or even if he understood anything anyone had told him. She asked Phong, a young hospice nurse originally from Cambodia, to act as translator, but that, too, created more layers of difficulty. She was younger than the patient, she was female — to admit vulnerability to her might have been an act of great shame for him. Finally Loehr told Phong, the nurse, “Ask him why he thinks he’s here.” The question was translated, the man looked Phong right in the eyes and said, in Thai, “I’m here because I have terminal cancer.” From then on, everything was much easier.
ANOTHER WELL-SPENT GRANT
There’s a story, possibly apocryphal, that the National Cancer Institute conducted a study to find out what would happen if people didn’t die of cancer, and they found out that...they would die of something else.
MED ED TWO
In one of the conference rooms in the acute-care center, Judy Davis, Director of Bereavement Services, was getting ready for the day’s small batch of medical students by scattering on the table stones of all shapes and colors, shards of sheepskin, model cars, shells, dolls, and weathered pieces of wood. As the students drifted in, she asked us to pick up one or two of the items that took our fancy. I took a brilliant-purple polished stone and a racing car in the shape of a shark; two of the students fought over a tiny plastic Tyrannosaurus rex.
In her two hours, Judy was trying to achieve at least three things; to outline the hospice’s bereavement support services, the most extensive I’ve ever come across; to show these doctors-to-be how to communicate with patients sympathetically and respectfully, and to get them to think just a little about how they think about death.
Traditionally, doctors think about death as little as possible and talk about it even less. Until the last decade or two, the vast majority of physicians avoided telling their patients when the diagnosis is terminal, arguing that the bad news will send the poor soul into a fast downward spiral. (As recently as 1972, 60 of 73 doctors in a private Detroit hospital refused to discuss their attitudes toward death and dying. And while all the remaining 13 agreed that a patient should be told if his illness is terminal, only 2 had ever actually done so. The task was either too difficult for them or they saw it as simply not their job.) This apparent concern for the patient’s spirits was more than somewhat undercut by the fact that instead of making up for the lack of information by kindness and support, the average doctor in fact chose this moment to vanish altogether, leaving the patient feeling not only sick and confused but abandoned.
Studies of nurses, meanwhile, showed that when patients said things like, “Am I dying?” eight out of ten nurses avoided any discussion of the patient’s thoughts or feelings — which again might show a commendable concern, but for the fact that other studies showed that when a terminally ill patient called or rang for a nurse, it took him or her almost twice as long to respond than to someone who was less ill.
My father’s death from cancer in 1979 was typical of this set of attitudes and beliefs. When he first became ill, he was seen by a steadily rising hierarchy of physicians until he reached the consultant, the “top man,” who was invariably cheerful and optimistic, refusing to discuss any possibility that the disease might not be curable. As radiation and chemotherapy treatments went on and their benefit became more and more temporary, the top man appeared less and less often, and my father slid back down the medical hierarchy. He was moved out of the prestigious urban hospital, because he was an embarrassment, a piece of bad publicity, at no point did anyone tell him that his cancer was looking incurable.
After 18 months, they finally took him off all treatments except morphine, and when his mind cleared, he asked, “Well, what’s the plan now?” The attending physician to whose level my father had now fallen was a young Indian doctor who took my mother out of the room and burst into tears. “I can’t tell him,” he said. So my mother went back in and told my father that they were letting his system clear itself out and then they were going to try something else. When he died a few days later, he was intermittently crazy. Knowing intuitively that he was dying, but never having been told, he put the two facts together and concluded that the hospital staff was secretly trying to kill him. When my brother visited him on what would be his last day, my father handed him a pair of scissors from the nightstand. “Take these,” my father said, “'they’ll try and get you on the stairs.”
The medical students drifted in. There were five of them, all in their third year, three men, two women. Some were in white coats, and one sported stethoscope and patella hammer. He and one of the women had just come from their surgery rotation. Most said they didn’t yet know what they’ll specialize in; one of the women, she who had just finished her surgery rotation, announced crisply that she intended to be a cardiothoracic surgeon. None had lost a close family member or friend.
This was their second half-day in the hospice. They had already seen the videotape of physicians with cancer, though it was hard to tell how much they had yet grasped. None could sum up the hospice philosophy. One or two yawns were smothered, though it was, after all, 8:15 a.m.
First she told us about the bereavement work at San Diego Hospice. Bereavement support is crucial because grief is so poorly understood. Survivors know what you’re going through. Neighbors may say, “Oh, aren’t you over that yet? It’s been a month, now.” Grief is like carbon monoxide, invisible, undetectable, often you don’t even know it’s there until something triggers you and you forget the rest of your sentence or drive into a wall.
The bereavement team, she said, calls family members at 2, 6, and 12 months after the death, more often if tipped off by a nurse, chaplain, or social worker that someone or a family is not doing well. Many people just need to talk to someone who has been there too. Like most major upheavals, death engenders experiences for survivors that other people just don’t seem to understand. We seem to acquire a new emotional vocabulary other people just don’t seem to have. SDH holds support groups during the day and in the evenings, involving children as young as three years old, who, far from being too young to be included, may be most at risk because they have so little life experience that it’s hard for them to put death in context.
Every Saturday a volunteer couple leads a walkabout for survivors, starting down by Mission Bay. This has developed into something of a social group, and some of them go on to brunch together afterwards and put on potluck suppers every so often. The hospice itself sets up potlucks too. The bereavement team also sends out a newsletter every month for 18 months, each issue designed to address the difficulties the bereaved may be facing at this point. Judy called it “a programmed learning about grief and loss.” Bereavement outreach volunteers visit those who can’t or don’t want to visit the hospice. Every family is sent a package of recommended readings, too — the whole family, not just the primary caregiver, the visible one. All these services are open not only to SDH families, but the community at large, especially to those who have lost a relative elsewhere in the country.
SDH is also called into the schools, especially by peer counselors who feel unequipped to discuss the deaths that affect students — car crashes, drug overdoses, gang shootings. Judy went through an exercise in which she stacked up a child’s blocks as if each were a stage in one’s life, then sent them crashing to the table top. This is what grief does to you. Life afterwards is a process of rebuilding, though one of the pieces is now missing.
She now handed each of us a dozen small, square pieces of scrap paper. Idly, I turned mine over. They seemed to be surplus copies of a promotional flier, five-by-five inches, on glossy, coated stock, that told the story of Glenn Wells, 82, who came into the hospice’s acute-care center with colon and liver cancer, in acute pain, and near death. Ten days later, the flier said, he went home free of pain and other symptoms, attended his grandson’s high school graduation, and resumed playing golf.
I’m of two minds about the flier. It reminds me too much of the slick, triumphant TV ads for the for-profit cancer hospitals. It’s careful not to say that Wells is “cured,” but it’s equally careful to avoid any mention of his long-term outcome or of death in general. True, hospice has to work hard to overcome a you-go-in-there-and-never-come-out-alive stigma, and in fact a good number of patients visit the acute-care center of any hospice for a short tune-up and then return home. All the same, such a “star patient” promotion seems slippery, quite at odds with the rooted, positive pragmatism of hospice in general.
On three of the squares of scrap paper, she said, we should write the names of three people who were our nearest and dearest. On another three we should write our three favorite possessions, on another three our favorite activities, and on the final three the qualities we like most about ourselves. (This in itself was quite a challenge.) Lay them on the table in front of you, she said, and follow the instructions I give you. She began to read from a sheet of paper.
“Picture yourself at your doctor’s office. It’s the middle of October and one of those perfectly wonderful fall days. There’s a nice breeze with a touch of coolness in it, but the sun feels warm on your skin. You see your doctor smile at you when he says hello, but the smile doesn’t reach his eyes. He looks tired to you, and suddenly you feel nervous. You hear him say that the test results are all in, and he is so sorry to tell you that the news is very bad.
“I am the virus. I am the virus that we call HIV, and I have supreme power. I can take things away, anything that I care to. Because I am so powerful and because I have complete power over you, you must do what I say. I now want you to let go of three things that you value. And let them go by throwing them into the middle of the circle now.
“You have just lost three things that you value. You are angry, resentful. Because I act slowly at times, you have an opportunity to regroup and adjust, time to take stock in what is left. And then suddenly I’m back; and because I am all-powerful, I demand that you let go of one more thing that you value. You must tear it up and throw it away.”
Now she had our attention. Except for her voice and the intermittent sound of tearing paper each time the disease progressed, the room was utterly silent. In her narrative, the months passed and the disease demanded more of the things we held most dear; in our imaginations, we were pretty shaken.
“I want you to take a look at the last two things in your hand, examine them, prioritize them, and now I, HIV, want you to let go of one more item that you hold dear. Because I am supreme, you must let go of it now.
“You are left with one very precious thing. And finally I return, and I want one more item from you. Look at the one thing in your hands and let go. You must do this. Tear it up. Now you are dead.”
After a stunned silence we talked the exercise over, agreeing that possessions mattered least and people most, discovering that the exercise had reopened some grief or loss in everyone’s life and made it available to them as something to learn from.
And what might they learn from it? Judy’s summing up showed how potent and long-lasting good and bad clinical communication can be, affecting one’s whole perception of a death, even of death itself. When her son died, she told us, in a hospital, the doctor didn’t come out and tell her himself. “I understand,” she said, “but I’ll never forgive him.” Instead, he sent a nurse. The nurse did something that, Judy said, she may forgive, but she will never forget. She smiled, perhaps out of nervousness. It was not a moment for smiling. She also came a little too close and in doing so left a strong whiff of perfume — and 20 years later, Judy realized that this was why she had hated perfumes all her adult life and had refused to use them.
Twenty years later, her father died. The doctor came out and told her himself, quietly and directly, “Your father’s died.” Not too distant, not too close, he asked, “What can I do to help?”
“Can I see him?” Judy asked.
“Of course,” the doctor said. “Would you like me to come with you?”
She asked him to go in with her, and after a few minutes she asked him to leave so she could be alone. He had done his job and had done it right.
“The work that you do with the dying and their relatives will last a lifetime,” she told the students, quietly but forcefully. “Do it well. And if you can’t, don’t do it.”
A THEATRICAL DETACHMENT
At this point, this article is going to seem to go seriously astray, so I might as well come clean. My aim is not simply to write about hospice, though that in itself is a worthwhile aim, as hospice is poorly understood even by the mainstream medical community. My aim is to make you less afraid of death, and examining hospice is one way to do this.
The odd fact is that the death we (will) experience is probably very, very different from what we think it will be, based on deaths we (may) have observed, especially deaths we’ve seen on television or in the movies. The best illustration of the difference between the death observed and the death experienced is in trauma—that is, major bodily injury of the kind to which we normally respond in shock and horror. When we talk about “horrible” and “ghastly” wounds, we’re actually describing our own reaction. The worse the injury, in fact, the less likely it is to involve pain and suffering — at the time, at least. The pain and suffering are actually part of the healing process.
Few injuries seem more terrifying than falling from a great height, for instance, yet in Choices in Healing, Michael Lemer points out that studies of Alpine climbers who have survived falls reveals that, as usual, popular culture has got it all wrong.
“As the fall begins, the climber does not scream as falling people do in the movies. Instead, time slows down enormously — as it does for many people just before a car accident. Everything seems to be taking place in slow motion. The [theoretical] survival benefit of this slowing down of time is that the falling climber has every opportunity to notice lifesaving possibilities — handholds or shrubs that might be grasped to break the fall. But if the opportunities for active self-preservation disappear, the faller then enters a state not of panic but of deep peace. He may experience the often-reported process of life recall, with his life flashing back before his eyes. He may hear celestial music. Hitting the ground is usually experienced without pain — he only hears the impact. Hearing is the last sense to disappear into unconsciousness.”
The same holds true in the more prosaic setting of the urban emergency room. “Some of the spiritually most peaceful deaths I’ve seen — that is, the calmest, the ones with least anguish, are in people who have been horribly injured,” said Dr. Mary Margaret Loehr. “Most people are very surprised, and kind of detached.” A man was admitted to the Scripps ER with a shotgun blast in the abdomen, still conscious, with “almost a theatrical detachment.” He was alert and functioning well enough to be able to tell them his own name but also to be able to refuse to name his own wife as the person who had shot him.
The greatest psychic anguish seems to be in those who are fighting to breathe and in general still feel they have some control over their condition. It’s when we lose or give up that control that we find the calm and detachment. “When people come in with severe heart attacks in great anxiety, we medicate them, but I’m often surprised by the degree of peace and calm that then come over them. It’s not just medicine.”
It’s almost a rule of thumb: the grimmer a person looks, the less he is suffering — unless he recovers, that is. Former San Diego police officer Donovan Jacobs walks a little stiffly, his left arm hanging at his side. He has scar tissue running down the left side of his throat and a deep dimple in the back of his neck where a bullet was dug out, and a long scar running a foot down from his navel where the surgeons went in to repair internal injuries. He doesn’t look like a cripple; he has the look of a man who has been battered but is still plunging on.
Jacobs, now a lawyer, is careful to explain that it’s very hard for him, especially after several weeks of painkillers and at ten years’ remove, to be certain what he experienced at the time or, perhaps more importantly, what he did not experience. He might have had the same curious lack of fear or pain that the climbers reported, or he may simply have lost those memories under the influence of morphine, Demerol, and Percodan and who knows what psychological defense mechanisms.
Ten years ago he was in his patrol car with his partner and a young woman observer, a “ride-along.” They pulled over a pickup truck driven by Sagon Penn. A fight developed, during which Penn managed to grab Donovan’s gun. He shot Donovan in the neck, then shot Donovan’s partner, killing him, shot the woman in the car, then drove the car over Donovan as he lay on the ground. Donovan probably came as close to dying as humanly possible. He lost 17 pints of blood, had both his shoulders dislocated and half a dozen ribs broken, suffered numerous internal injuries from being crushed by the cruiser, whose catalytic converter also inflicted third-degree burns on his arm. The bullet passed through the brachial plexus area of his neck, which is a major nerve junction, damaging a number of nerves including those to his left arm. Despite these massive injuries, he remembers only one brief moment of pain. His memories come in glimpses; the ellipses represent the blank spots between these glimpses.
“I stopped him...I asked for his license. He tried to hand me his wallet. When I told him that wouldn’t do, he turned and started to walk away from me...I may have grabbed his shoulder...I was hitting him in the back with my baton as he was fighting with my partner...he turned on me...we went to the ground...I was on top of him, wrestling with him, trying to get him turned over so I could handcuff him...we were surrounded by a crowd of about 30 non-hospitable people who seemed to be about a foot away, and I thought I was going to get my face kicked in by them...the next thing I remember. I’m shot and on the ground, thinking I had to get up and fight back...I think I remember hearing people scream...I realized he was driving the car toward me and wanted to run ifie over...I saw the undercarriage of the car as it passed over me, and I thought, 'God damn, this hurts’...lying there expecting the cavalry to be there...the paramedics were there putting me into a mast suit, which is a set of pressurized pants that push the blood from your lower body toward your upper extremities. I knew that had meant I’d lost a lot of blood, because I used to be an ambulance driver for the police...I was in a helicopter on a stretcher, looking up, thinking, 'They don’t give you much headroom on these things.’ I don’t know what I was seeing, but it was right above me, a few inches in front of my face. I guess they shelve you into something...I knew that Tom had been hurt, and I remember asking about him, and when they didn’t give me a response, I knew that was bad.”
He doesn’t remember anything of his first three or four days in intensive care, then he has vague memories of visits from friends and family. Continuous memories start from when he had been in the ICU for three weeks. By then he knew he was in pain, though the painkillers kept at bay both the physical sensation and the emotional impact of what had happened.
“I don’t remember ever entertaining thoughts that I was dying. I don’t remember feeling any pain at any point except when the police car ran over me.”
Trauma illustrates most clearly that we tend to talk about death the way we experience it as outsiders, onlookers. This not only affects our own attitude toward the death we expect to have (and may strenuously resist thinking about) but also affects the way we treat others who are dying. In a sense, if we have foolish attitudes about our own death, that’s our own business, but others who are dying are very, very vulnerable. It’s extremely easy to override their wishes and needs and to do so out of our own prejudices. The mother who wanted to die in peace but couldn’t say so because of the tube down her throat is only the most extreme example. Death is a process of individuation, hard though that may be for us, the living, to accept.
Perhaps the greatest and most enduring value of hospice is that it changes the context of death, and therefore the meaning of death. It gives us a glimpse of what death might be if it took place not in the helpless panic and emptiness of the ER or the ICU but at home, in the midst of a family newly reunited by the event, the dying person having taken care of all that kept him from moving on.
MOVING ON
Even to use such-a phrase as “moving on" implies, of course, a prodigious leap off the train of conventional medical thought and onto a different set of tracks altogether. It implies that we — or at any rate something of ourselves — survive death and continue in some other form of existence.
It’s often said that death is a mirror that makes us reflect on life. I want to look for life through death, like a physician examining the brain by shining a light through the black vacancy of the pupil or an astronomer wishing he could peer through a black hole to glimpse bizarre counter-realities on the other side.
In a hospital, death is a medical death. Everything, or so it seems, can be explained in the accepted medical terminology of the time. Hospice offers a chance to see death in a different light than the brilliant glare of the hospital, a chance to experience it more directly, in our own words and through our own assumptions. Hospice has also given authority and respect to those farther down the vanity ladder, to nurses, aides, volunteers, patients, and family members, those less thoroughly versed in the clinical explanations, and the results are startling. Probably the most commonly recommended book on a hospice bookshelf is Final Gifts, written by two hospice nurses who mattcr-of-factly spend over a quarter of the book discussing near-death experiences, those remarkably common intimations patients have of their own imminent death and the conversations they apparently have with those on the other side.
By dismissing such experiences, as many in mainstream medicine do, calling them hallucinations, we change the entire nature of the experience of death, denying comfort to both the dying and their families and, as the authors, Maggie Callanan and Patricia Kelley, point out, often causing great agitation and anxiety' to the dying who are trying to tell us the marvek>us things they’ve seen. Kathy Ferdinandson passed on two such stories.
An elderly woman’s husband had passed away several years beforehand. She was convinced that she would meet him in heaven and looked forward to the day when she would die. A week before she died, she said, “Kathy, I’m going home." She was in a skilled nursing facility, and Ferdinandson misunderstood her drift. “You are at home,” she replied. “This is your home.” She looked hard at Kathy. “I’m going home," she repeated firmly. Within a few days her physical condition took a clear turn, and she began actively dying. Kathy found her holding a conversation with John, her late husband. The nursing staff had noticed it too, though they dismissed it as hallucinating. When Kathy sat down next to her, the woman turned to a spot elsewhere in the room and said, “I will, John, I will."
“Who were you talking to?” Kathy asked.
“To John,” the woman said. “He was asking me if I was coming home.”
She died that night. Kathy believes that he had come to assist her in making the transition.
The second story involves a man who was seriously ill and so frightened of dying that he refused to talk about it, which made the hospice work very difficult. He had been on service for a while when his mother came to visit with the intention of helping take care of him. Shortly after she arrived, she had a heart attack and died on the kitchen floor. He was terribly upset. Kathy suggested, “Could it be possible that she died first to be the one to go ahead and show you the way, to help you over your fear of death?” He didn’t seem to want to entertain that notion.
Shortly afterwards, he began actively dying. The doctor noticed that he seemed to be looking at and responding to things that weren’t in the room and again considered what was happening to be some kind of hallucination. “Are they frightening?” he asked the patient. “Would you like me to make them go away?” — that is, by medicating him.
The man looked clearly at several different and distinct places around him. “No,” he said. “They’re beautiful.”
“What I thought,” Kathy said, “was that they were angels or spirits come to help him over because he thought death was so despicable.”
Near-death experience stories, brought back to us by the revived, are by nature less common in hospice, where revival is usually not the point, than in hospitals, but anyone who has broad experience with death has run into them.
“I’ve had patients say to me, ‘I saw that light, and I came back because I hadn’t finished telling my kids what I wanted to tell them,’ ” Laurel Herbst said.
“You’re not afraid when you’ve had someone die and come back to life and tell you about life on the other side,” said Joan Snyder, a staff nurse at Scripps Memorial Hospital, Chula Vista. “We had a physician who died on the golf course. He was coded. We kept bringing him back and bringing him back, and he said, ‘I’m happy where I am. Leave me alone.’ I’ve had people say, ‘I know you.’ I’ll say, ‘You can’t know me. You were coded when I was working on you.’ ‘No, I know you. I was up there in the corner watching.’ ”
AN UMBILICUS TO GOD
I can’t claim to have gone through this investigation unbiased or unmoved. But whose ambition is it to be unmoved by death? And what can we learn only by allowing ourselves to be moved? At the end of her session with the medical students, Judy Davis finally turned to the cornucopia of found objects that we had picked over two hours previously. She asked us to use one of the items that we had picked to make a point about grief, and the gist of her message seemed to be that if doctors use such third-party narrative ingredients or symbols, they are forced out of doktorspeak, they have to want to communicate clearly. But something weird was going on, all this talk about grief must have stirred the pot for me, at least, because I abandoned my journalistic detachment, not to say my common sense, and showed the group my polished purple stone and told them about my vision of the chromatogram of the soul.
In the weeks after my mother’s death, I said rather selfconsciously, I spent a lot of time in an odd, otherworldly state of joyful detachment. I was still operating in the material world, but it seemed to have lost its power to upset, irritate, or depress me, and instead of seeing reality at this stratum of anxiety, this stream of things-that-had-to-be-done that twittered like the gibberish on a shortwave radio, I felt as if I had an umbilicus to God. I moved at my own pace, possessed of a constant sense of wonder, and every so often I would see or think of something that sent a rush of sheer joy up through me, and I would clench my fists and think Yes! Yes!
It was as if I had moved to a new dimension that had always intersected with the world I knew, but I had never seen it — and even now it was not visible, though it was almost tangible, but I could sense it everywhere and see its outcomes and effects protruding into the events of ordinary being like the tips of warm icebergs. I found myself instinctively carrying out small acts of kindness or courtesy—waving drivers ahead of me at intersections, exchanging pleasantries with supermarket cashiers — and seeing joy and kindness everywhere in return.
During this remarkable time, I suddenly had a sense that I could imagine a chromatogram of my soul — not that I could see it, but that I knew what it would look like if it existed in visual terms. It would be rather like this polished stone, only instead of being predominantly purple, with fascinating flecks and spots of other colors, it was mostly yellow and white, with clearly defined dark patches like small vortices that were the parts of me that I still hid and was afraid of.
I was sorry to be so mystical, I said, feeling a little embarrassed, but one of the things I suspected about grief was that a death in the family takes us (in some instances, at least) through a more essential tijne in which we briefly realize how much other people mean to us and how powerful and lasting and redemptive this emotional or spiritual dimension of life is. When we stumble away toward our ordinary, workaday lives, their demands and values seem petty, unwholesome, ungrateful, demeaning — they miss the point. Everything seems like network television and junk food, spiritually destitute, lacking any real nourishment. We resist going back to it, and we are right to do so, seeing clearly its limitations. Yet everyone around us tells us that this is the real world, this is normal, and we simply must knuckle down and get back into it. No wonder some kinds of grief mimic depression.
The tragedy, then, is not so much when someone dear to us has died, but when we have the chance to learn something miraculous from this, their last gift to us, but don’t. Even as I write this, I find myself glancing at the clock, at my date book, checking to see what I need to do this afternoon, giving tiny mundane obligations the chance to throw me off stride, flinching away from the challenge of asking, “How would it be to live life well?” the weight of my habits slamming into me like small cars on a freeway hitting a tractor-trailer that has come to a halt sideways across all three lanes, pondering a turn to the right where no asphalt has yet been laid.
Yes, this is a strange form of journalism, isn’t it? But somehow it all leads up to this, that death, once the fear is overcome, is our severe but brilliant tutor on life, demanding nothing less than the truth and offering insights that leave us reeling, saying, “Leave your computer right now, stand downstairs in the winter sunlight for a while, and you will know what to write, saying that there is pain and loss but there is no need to be afraid. ”
Comments