 Facebook
Facebook
 X
X
 Instagram
Instagram
 TikTok
TikTok
 Youtube
Youtube
It dominates the hill like some neo-Roman rebuild of an ancient Greek acropolis, covers it, a dozen crossed layers of cream-colored cake and tinted glass. Across a spreading slope below, spangles of sunlight bounce through a ripple of breeze-blown trees in a lake of parked cars. Nearest the building, empty buses idle.

Walking from a far corner of the visitors’ lot, I approach the main entrance to the Veterans Administration Medical Center, San Diego. It overlooks La Jolla Village Drive and a long stretch of I-5.
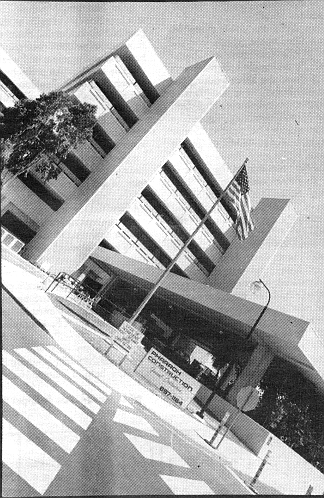
Strangely, it looks less hospital than computer plant. A few old men sit at the steps, waiting, their faces frozen, deeply creased, like living gargoyles.
Passing the old men (their eyes as silent as their mouths), I come to sliding glass doors — opening, closing, opening, like heart valves — and slip inside. First sensation is smell; then a sickly memory that always follows. (This time, I think of being ten years old, receiving the only enema in my life.)
A 50-ish man of 300-plus pounds exits the building in an electric wheelchair. He resembles Jabba the Hut and sports a black cap with “Old Fart” emblazoned in bright orange. A scarved woman of equal weight but considerably less height escorts him out the door.
In a cubbyhole office, a black security guard sits studying his hands. At a silent signal, his eyes lift and pause with suspicion on mine. I move away from his gaze and stand in front of a portable bulletin board announcing classes on proper nutrition.
Across the lobby, clustered by a semienclosure of tables, four elderly men laugh. I approach the one sitting sideways behind the front table; his right arm rests on the tabletop. Scars reveal that the hand had once been butchered and later sewn together into three grotesque fingers. White letters on a shiny-black tag declare his name — JIM. Jim looks up and smiles at me with the honest sincerity of my father.
“Yes, sir. Can I help you?” he says.
Public relations isn’t my normal duty,” explains Bob Stevens, whose title — administrative assistant to the medical center director — is as broad as his job. “I provide administrative support to the director on any and everything he has to do, all the reports and contracts, I run the medical staff office, and then I do facility planning, coordinating all the movement, projects, things like that. Our public relations person is out on maternity leave. I’m just covering that while she’s gone.”
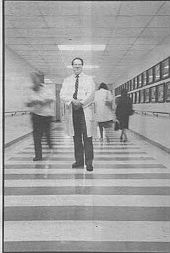
Slight of build and soft-spoken, Stevens handles himself with an air of adroitness. Everything about him is conservative: knit V-neck vest, cotton shirt, dull-blue striped tie, wire-framed glasses, mustache that’s scarcely visible, and hair (receding, thinning, graying) parted on his left. Number-three man on the administrative side of the house, Stevens is fairly high up this “corporate” ladder. (His office has a window — with a view.)
Overall, however, he’s a small part of an incomprehensibly complex bureaucratic machine. The Veterans Administration is the second largest federal agency and employs one of every eight fulltime government workers. San Diego’s VAMC is just one of 172 such medical centers.
I’d come to his office to arrange a quick tour and set up some interviews. But I also came as a veteran. A combat veteran 60 percent disabled in an ambush 22 years ago. I have been to the Wall (Vietnam Veteran’s Memorial in Washington, D.C.) and read the names of those I knew would be chiseled in. And I found the names of others I didn’t know would be chiseled in. But more startling, there were guys I’d seen horribly wounded whose names I’d expected to be there — that weren’t. No doubt, some of those boys returned home, healed, and today are just another middle-aged Joe on the job. But what about guys like my platoon sergeant, Staff Sergeant Blankenbaker — who got most of his head blown away by a mortar round? His name’s not on the Wall. Where do they keep the vegetables?
Stevens looks at me benignly. “Before I came here I was at Fort Lyons. It was strictly long term. And there are others in the A system that specialize strictly in the long-term care. In Colorado we had a unit that was totally, you know, what you call vegetable-type patients that have been there for 10 or 15 years. They’re totally fed by a tube. They’re just — they’re vegetables. In a layman’s term, that’s all they are. And they’ll be there till they die.”
Vietnam wounded?
“Yes.”
Head wounds, mostly?
“Yeah, mostly.”
I’m the chief of voluntary service. That’s my title,” says John Stewart, a big, broad-faced man with a thick swoop of dark hair, a rapid-fire manner of speech and a physical demeanor that suggests the street-tough loyalty of a Sicilian bodyguard. High on the wall behind his desk, prominently displayed away from an adjoining wall covered with plaques and certificates, hangs an autographed picture of George Allen.
“I’m a native Californian, and when the Rams fired Allen, it made me mad. So when he moved to Washington, I started following the Redskins. And then by fluke accident I got transferred to Washington, D.C. — in fact, that’s where I trained to be a voluntary-service chief. George used to bring Sonny Jurgensen and Billy Kilmer to the hospital every year to visit the patients.”
I ask Bob if he is a veteran.
“I’m a Vietnam-era veteran; I was in during Laos and stuff like that, and I was in the Air Force, so I’m not one of these guys going on the front lines getting shot at. There’s a lot of difference between getting shot at and sayin’ you were in the war.
“You'll probably find a rule, it’s kind of an unwritten rule. The people that bitch the most probably deserve the least, and the people who bitch the least — probably we owe ’em everything. Just like some of my volunteers are also patients, outpatients, and they represent various wars. There’s a guy sitting out here at the front desk that’s a leg amputee, a World War II pilot. His name’s Jim.
“Another guy, this guy’s a Congressional Medal of Honor recipient — means he did something. It’s the highest award the country gives. And here he’s over in Vietnam, and he was a sergeant, and supposedly he literally went back and forth carrying his men one at a time off this hill where they were surrounded and being shot at by the Vietnamese, and he got shot himself. He did this, comes home and gets the highest award, and then he rolls in here and his diabetes causes him trouble, and they’re deciding to amputate his leg. Well, he was always in here happy, and flirtin’ with my secretary a little bit, and kiddin’ me a little bit, you know. And he coaches football out here at one of the high schools. And he’s in a wheelchair, then all of a sudden he’s walking — he’s on crutches but he’s just gettin’ where he’s off the crutches and he’s starting to walk on his own a little bit. And he’s always been so upbeat. He’s just the nicest man in the world.
“Then you have somebody else, say they were in basic training, had a nervous breakdown, and they come through the door and say, ‘I’m a vet’ran. You owe me!’ Or somebody gets on drugs, wants to blame the military ’cause they got on drugs. Well, you know — there’s no comparison.”
Lot of people try to milk the system?
“That’s true. I’d been a therapist before I got into this job. I’ve been in the A over 20 years. And I told my dad one time, ‘I’d like to have a job where I just went from hospital to hospital acting like a patient and uncover the people that are milking the system.’ He says, ‘Yeah, and you’d wake up in the alley with your neck slit sometime.’ And he’s probably right. But how many times do the government and the taxpayers owe a person to go through the detox program? One time? Twice? Ten times?
“I worked in Danville VA hospital as a recreation therapist, and one of the guys I had there as a patient — nice guy, don’t get me wrong — was in and out of that place for alcoholism. Not once, not twice, maybe three times. Then I left there and went to Washington, D.C. Then I went to Omaha, Nebraska, and then to Westside Chicago. My first day at work at Westside, I walk in and I hear this guy say, ‘Hey, Stew!’ And I turn around and here’s this same guy. Later on I transferred across town to Hines — here’s the same guy. So that means that this guy’s been in three of the hospitals that I’ve been in, see, and treated in every one of them for alcoholism. I think he’s probably dead by now. Probably drunk himself to death. He was a nice guy, but how many times do the taxpayers owe a guy like that?”
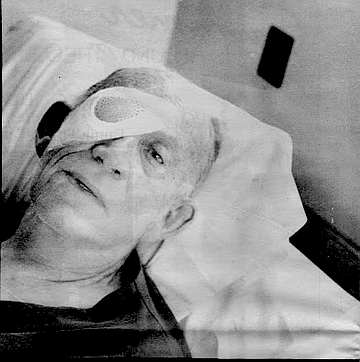
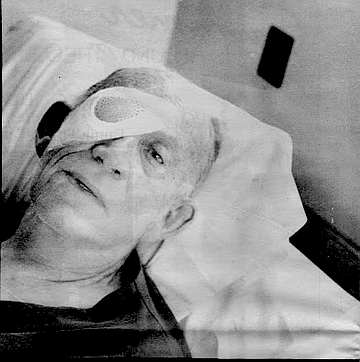
Charlie, an ex-Marine, looks dead on the narrow bed; long forearms and liver-spotted hands limp upon his chest, old fingers intertwined. The sleeves of his dark-crimson pajamas are shoved to the elbows — like a man unafraid of work. Top’s unbuttoned, splayed to the sides, and a still-strapping torso breathes silently in a white T-shirt. I touch his forearm.
“Mr. Deasher?”
His eyes open slightly. He shows no alarm. No concern.
“Remember me?”
“Who?” he says, unblinking.
“I met you at the front desk. You said I could interview you.” “Oh. Okay.” He closes his eyes and swallows. “Okay.”
His front teeth are gone, the gums purple. I start lightly: Tell me about yourself.
“I’m legally blind.” (His eyes remain closed.) “My job as a volunteer now is I work at the front desk, and tell people as they come in how to get to different wards, like to X-ray and eye clinic, and where to check in, ‘I’ve never been here before....’ Things like that.”
What’s your surgery for tomorrow?
“Routine eye surgery, which is number 13 eye surgery. Damage from the war and the atomic bomb.”
You saw Nagasaki when you were a POW?
“Yeah.”
Would you tell me about it?
“In the first place, I was too tall to work in the coal mines. I couldn’t walk through the tunnels. So I tell ’em, ‘Me farmer boy — cut weeds!’ Damn if I didn’t get a job cuttin’ weeds. The hell, it’s hard work though. And this particular day I was cuttin’ the weeds, and the guard was up there with me, and I noticed a lot of American planes, carrier planes, to the south of us. And about that time, the civilian guard decided he had no place to be up there on that hill. He bugged out. So I sat down and watched the airplanes. He left his lunch pail with little rice balls with the special insides in it, which was not too bad. And so I was sittin’ there just watchin’, and then I saw the blast.
“It was just like the picture shows. When it went up it was brown, and up like that,” he separates his fingers and gestures with his hands, “and mushroomed, then come back down.”
When I ask him about being taken prisoner, his eyes open, and he lifts his head.
“The United States Government knew many, many weeks before the war started, before Pearl Harbor got hit, that the Japs was gonna come.” He lays his head back. Closes his eyes.
“When they hit the Philippines Navy yard, they killed 2500 civilians out of 7000 civilians, and one Marine, and 130 service that I know of, plus all the ships that went down, and all the men that went down with the ships, which we’ll never know how many men it was.”
How old were you then?
“About 30 years old.”
How old are you now?
“I'm about 78. I’ll be 79 in November.”
Were you in the Death March?
“I didn’t make the Death March. I was on Bataan when Pearl Harbor got hit. I come back to Clark when it got blowed off the map. And then the colonel called. See, I had the motor pool, I was in charge — corporal. The colonel had me go to the Navy yard to assess the damage. Why, then I come back with a pickup truck and hauled the injured.
"This ensign took ’n’ helped me with the injured and put ’em in the truck, and we took ’em back an’ forth to the hospital three miles away. That was a bad mess. The town and everything was all ruined. There was so many dead and everything. Then we went all the way up to Bataan for some time before we went over to Corregidor for beach defense.”
How were you taken prisoner? “Capitulation. We stood by, and [the Japanese] brought soldiers up, destroyed our weapons, an marched us to an enclosure, what they called 92nd Garage. A very infested hellhole. They had dug holes with tractors for defecation. It was really a bad situation.
"There was malaria and pneumonia and everything like that. I was put on a workin' party, and I had to go out in the water an’ pull in the dead Japanese soldiers — the ones that had the sabers and leather belts and stuff — to pull ’em in on the dry land, and then I had to strip ’em, strip the leather goods an’ all that stuff off the dead Japs.
“And then they set us underneath the tree there t’ take a break. And ’course I knew the island perfect, and I went over the top of the hill. We went an’ hid out in some caves I knew was over there. And then when it started t’get little toward evening, I went up by the water where I found me a bucket and got a pail o’ water ’n’ come back t’ the [POW] camp through the gate an’ back in the enclosure where it’s safe. It’s all tricks o’ the trade o’ survival.
“Then they took us to Manila, put us in cattle boats, stuff they put horses in, things like that, and then dumped us out — some places in three-foot water and some places over your head. We swam to shore, an’ then parade us up ’n’ down the streets of Manila. They put us in prison overnight, then moved us on next day. That group I was in stayed in the Philippines six months, then we disbanded and they shipped us to Japan.
“They kept us in the holds. Too many people. Most of the ships was torpedoed by the American torpedoes — submarines — because none of ’em was marked with ‘Prisoners of War,’ an’ that’s where a lot of our prisoners was killed. They wouldn’t let us come out an’ be identified, an’ they lowered buckets down to put our — what ya call — bathroom facilities, an’ they pulled it out an’ dumped it over the sides, an’ then run it back down to us again. They spilled it on us ’n’ made a hell of a mess of it. Very unsanitary.”
I notice that the tips of most of his left fingers are missing. How?
“Well, I was just an on’ry old sonofagun, a farm boy — five’n’half years old. And I just took a dynamite cap over at grandmother’s place. I took ’n’ hit it with a hammer, an’ the damn thing blew up. We was right there on the edge of the desert, an’ we used to chase jackrabbits, an’ play with the snakes, catch monkey-faced owls and give some o’ the stuff t’ the San Diego Zoo. Then later I was a lineman, worked for the power company, climb poles up to 55 feet, stringin’ wires an’ stuff like that. Learned all kinds of tricks ’n’ trades. Bailed hay. Pitched watermelons. I’d work with the green-card workers’n Imperial Valley there, side by side with ’em. Thinnin’ lettuce, 17 cents an hour. But we didn’t starve.
“Depression in the ’30s, we had a big ol’ garden. We sold about 1500 rabbits a year. And my brother an’ I, we had bees, 50 colonies o’ bees. Then the boss’s wife went ’n’ gave us some peacocks. We saved the big ones, the males, because they shed them big ol’ long plumes, looked pretty. The hens didn’t look so pretty so we ate them. Ate a lot of ’em. We never did starve.
That’s — that’s survival.
“Like in prison camp — Osaka. I traded. Some o’ the tradin’, I got grasshoppers — ’bout two inches long. We use t’ eat them grasshoppers. They was good stuff. ’Cept the legs bothered me. I had t’ kinda chop ’em up a little bit because they hard on your mouth t’ eat. But I’ve eaten a little bit of ev’rything. Ate whale blubber in prison camp. Oh, you just name it. If it isn’t poison, I’ve ate it.”
Charlie gets quiet, like it’s time for me to leave. I start to get up.
“All three of us brothers was missin’ in action at one time. I was prisoner o’ war; my brother was bombardier, an’ he went down. They run outta fuel. My other brother, when he went down ... he ... they didn’t even find his body. In the Pacific.
That’s where all of us were missing in action at one time.
“I never earned a Purple Heart. Oh, I had a few little scratches ’n’ burns ’n’ too many bombs dropped too close to me. I lost one staff car. Bomb missed the front bumper ’bout three feet, an’ I lost that. It burnt up. I was just 30 feet away, and it didn’t bother me at all. See, I always ran uphill where the soft ground was, never down the road. You on a road, the bomb hits, an’ shrapnel’l git ya. If you’re on soft ground, it goes in the ground ’n’ you don’t get hurt. It’s all tricks o’ the trade of survival.”
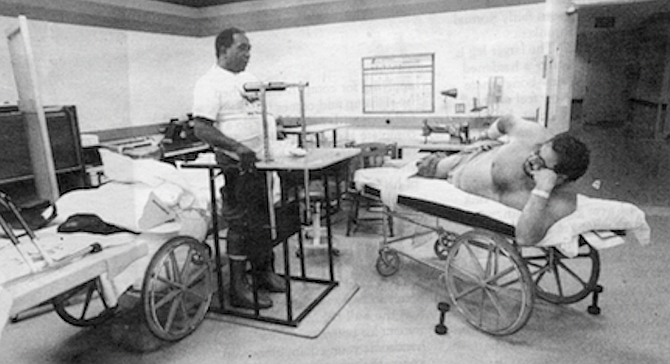
Here, in SCI...”
(Even the acronym feels like an unwashed finger down my throat. Can’t swallow. Sticks in my gullet. Piece of dead meat. Lobby area is twilight dim; refraction of brick and uncarpeted concrete, clean, polished as lacquered bone. Can’t swallow. Flickers of living corpse in forgotten moment. Receiving ward, Guam, 1969: boy on the gurney beside me’s not doin’ so hot. Wound in the back of his neck is small, but he’s paralyzed from there down. Compared to him, I’m fine. Earlier he’d said, “They told me it’s just temporary.” I wonder. Now his guts are cramped, but he can’t do anything. “Doc!” he says — we always call a corpsman Doc — “It hurts!” Corpsman asks him if he wants a “massage.” Boy says he does, “But hurry!” Corpsman’s calm as a clock. Done it before. Room is mostly dark — other gurneys in here, guys quiet in pretend sleep. Doc brings something over that glints in the light from the nurse’s station and starts digging soft and easy-like under the boy’s sheet, lifts him like he’s making a bed, says things like “ ... There we go ... How’s that?... All right!....”)
“Here in SCI...” she came back into view like a sunlit face through a screen door, brown hair and soft features, gentle voice, “ ... I’m responsible for new staff, nursing education, consulting with nurses about problems with the patients that they may not have the expertise to resolve.” Her name is Cathy Dunn, clinical nurse specialist, Spinal Cord Injury Unit. “I do a lot of counseling, particularly sexual counseling, and I do lot of consulting with patients in the main hospital that have rehabilitation needs, but I’m necessarily spinal cord injury patients.”
The SCI unit has been open for just two years, although it had been planned for more than 15. Money — funding approval and a bid within budget — held it up. There are 23 SCI units in the VA system.
I’m curious about her reaction to Oliver Stone’s movie Born on the Fourth of July.
“Some of the things depicted in Fourth of July were fairly accurate in the way that many VA hospitals were in the early ’60s and mid-’70s. Some of the film was exaggerated, because of where Ron was during that time, emotionally. I think that some of his memories of what it was like are a bit exaggerated. And in comparing the book to the film ...” (How many other people, I wonder, read the book for comparison?) "... it’s more exaggerated in the film.
“There are a lot of things that were in the film that are not done that way at all anymore in the VA system. For example, the one scene where they have all the guys in the room together having enemas. That’s something called the blue room that some of the old VA hospitals have.” (I recall an ugly old nurse shoving a tube up my ten-year-old butt.) “We have a blue room. We were made to put one in, but we don’t use it. We have individual bathrooms. Patients have all of their showers and that kind of care in the bathroom in a private area. But we don’t give enemas anymore.”
Not necessary?
“No. In fact, giving enemas over a long term can cause a lot of patients a lot of problems. We’re dealing now with the results of guys who used enemas for 20 years. They do use a technique to empty their bowels on a regular basis so they don’t have bowel accidents, but it does not involve using enemas.”
I tell her about the boy in Guam in ’69.
“That’s called digital stimulation. It’s using a finger to stimulate the rectum to relax and let the stool come out. Most of our patients have no voluntary control, but part of what we do with the patients is set up a program where by using different techniques they have control over when their bowel does empty.”
Do any patients choose to have a colostomy?
“Very rare. That would be in an extreme case, and in fact, the ones that we’re seeing using colostomies now are the guys that used enemas for years and damaged their intestines by doing that.”
How do you handle the despair? “It takes a certain type of person to work on a unit like this. Not everybody’s happy working on an SCI unit. I think that it takes a kind of person who can step back and knows when to push a patient to do as much for themselves as they can and yet be very supportive about it. You have to be able to switch your approach for the individual, because they’re not all the same. Not every SCI patient has the same personality or interacts with people in the same way. You have to interact with them as a person first. You kind of have to be a combination of a cheerleader and a whip cracker.”
(I remember a “whip cracker” and a guy across the aisle on the eye/amputee ward in Guam. He looked like someone who once was president of his high school’s science club. Every 15 minutes or so, he’d start babbling like a baby, disturbing everyone else. Pretty soon this nurse — who I later read about in Reader’s Digest — would storm over, tell him to knock it off, tell him to grow up, tell him to quit feeling sorry for himself. Both his legs had been blown off, his right arm at the elbow, and his left hand. And, like me, he’d been blinded in one eye.)
That paralyzed boy in Guam, I reminded her. He said they told him it’d only be temporary. Could they have known that?
Cathy looks at me straight and says, “They shouldn’t have said that.”
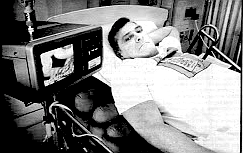
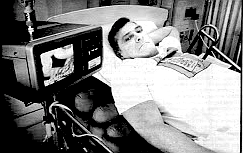
"I’m a lover, not a fighter,” quips a man prepared for the inevitable reference to the long-dead pugilist. Yet the way he’d sat up in his wheelchair and proudly articulated his name, “John C. Sullivan,” told me something. Sullivan may indeed be a lover, but he sure as hell is a fighter. His resemblance to John Wayne is almost scary. If he could stand, he’d tower over me; his neck descends from the ears; his lips press together stoically; his square jaw and Corps-cut hair mark the quintessential face of everything that’s not wrong with America. So, I wonder, what’s an old jarhead like him think about today’s Marines?
“You have to realize,” he says, turning and rubbing his clean-shaved jaw, “the difference in central values. I think today’s Marines are just as good, if not better than when I came in. All the troops I worked with were fantastic. I came in in 1956 as an infantryman, made the Lebanon landing in ’58, was in Santo Domingo in ’64-’65. Then I figured out it was easier to fly over mountains than walk over ’em. So I re-enlisted for aviation. Was in ’Nam in ’70-’71; rather, we were in country — but we weren’t. I was with electronic warfare craft, so we was back an’ forth from Japan and Danang. Nixon was pulling everybody out, and theoretically we weren’t supposed to be there. At the time, I was an ejection seat mechanic and anything else regarding pilots’ life-support systems.”
Ironically, Sullivan’s paralysis occurred as an indirect result of his military expertise. “I retired in May of ’85, and I took a job with a civilian corporation that had a contract with the Navy. Basically, I was to do the same kind of work I’d done in the Marine Corps. This was at Kingsville, Texas, where they train naval pilots.
"These young pilots had just , gotten their wings, and we were at a buffet party-type thing, and I was swimming laps in the pool. Two of the young guys picked up one of their buddies and threw him into the pool, and he landed on my back.”
Under normal circumstances, the blow should’ve resulted in little more than a temporary loss of air (and a few words). The circumstances, however, were not normal. “I’d had symptoms for almost two years, but the doctors kept telling me it was muscle strain.”
What symptoms?
“Sudden loss of bowel and bladder control, difficulty in going from a prone position to sitting, getting out of bed, off the couch, and tingling in my hands.
“I’m not downing the quality of the medical facilities, but all they had there was a clinic. And these people were just general MDs, mostly. They didn’t really investigate my problems as thoroughly as they should have. It wasn’t until after the accident that they discovered I had a cancerous tumor. What the tumor had done was it had crystalized my spine in the upper thoracic region. You know how flexible a bone is in your spine — the tumor had made it very brittle. When the guy hit me, the bone just shattered like glass. It drove a perfect piece of bone right through my spinal column.
"Severed it. I’m paralyzed just below the shoulders, right at the armpit level. And, due to other complications, my injury is going higher. I’m losing control of one arm and probably will lose control of the other.”
Is the cancer gone?
“They’ve got to wait five years to declare me completely cured, but I’m confident. I’ve had three operations, first when they went in to remove the piece of bone from my spinal column. That’s when they discovered the tumor. And two more since. I’ve had radiology, then a year and a half of chemotherapy. Off and on, I’ve been using this facility since July.”
You’ve been in other facilities?
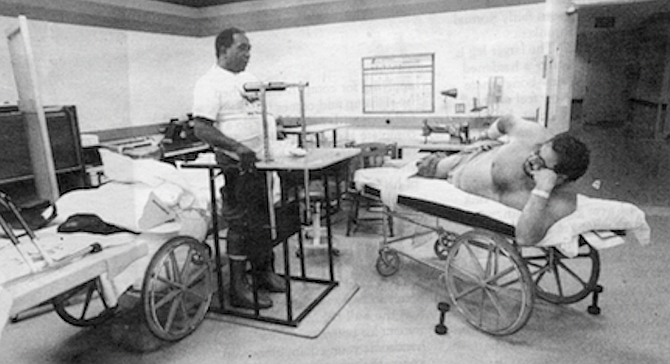
“I’ve been in Houston, Tuscon, Phoenix — those are the three VA facilities I’ve been in. I’ve been in various other civilian hospitals. The SCI unit here, this is probably the best I’ve been in for acute spinal-cord injuries. The only problem I think they have here is not enough money, not enough space, and not enough staff for what they’d like to be able to do. Don’t get me wrong, for what they’re able to do here they do it quickly, efficiently, and the care is outstanding. I was thinking more on the rehabilitation side. For instance, if you would go to a civilian center like Sharp — now I’ve never been there, so I can’t really evaluate the facility — but from what I’ve heard, they have a larger therapy staff over there, and they teach guys how to go over curbs, up and down stairs, how to overcome barriers — surviving techniques. See, they don’t have those facilities here. They don’t have the space, they don’t have the time, they don’t have the money. This place could be so outstanding if — Have you ever been downstairs?”
Sullivan’s hands, like the hands of all the SCI “chairs” in this unit, are dressed in fingerless, leather-palmed black gloves. I follow behind, his adapted hands thrusting in unison against the friction of wheels, across the lobby. He presses a low button, and the steel doors of a freight elevator open. Inside, his voice resonates.
“They got equipment stacked outside — Nautilus machines, all kinds of things, brand new, wrapped in plastic, ’cause there isn’t any room inside to put it.” The steel doors open after an imperceptible stop. We move down a wide hallway past an unfinished addition.
“They run out of money,” John says.
Farther, on the right, I see through glass onto the patio where large plastic-wrapped shapes sit. On the left, doors with narrow windows. I peek like a voyeur into a room secluded from the able-bodied and try to imagine what happens in there. From the walls hang gothic straps in assorted man-sizes and vapid colors. Then, in a cavity to the side, there rises from the floor a bedlike thing of stainless glimmer — a limbed, robotic skeleton. (Silently, I feel shame as the room conjures up images of Milk of Magnesia and — ugly old nurses.)
We move farther down the hall, and I peek again into a much broader room of assorted pieces of exercise equipment. Nearest the window are what look like blue tumbling mats, elevated three feet off the floor, each with the flat dimensions of two king-sized mattresses. “You can do a number of things on those mats,” John says. “You can roll, learn how to sit up, turn over.” He sees in my face what I’m wondering:-self-deprecating joke? “No, really,” he says, then pauses. He squirms, pushes up from his elbows, grunts softly, readjusts, an unconscious routine he does often, like a person who tosses in bed.
“You have to realize,” he continues, “I have no muscles ... How can I put this?” Then he sits back and lifts his arms slowly, pointing his fingers to his armpits. “Like from here, everything down is dead meat. It’s dead. Now you think about that. Think about trying to turn yourself over. I can’t turn over. Oh, I can maybe after 15, 20 minutes of trying. There are techniques where you can roll over. You have no balance whatsoever. The higher your injury, the less the balance you have.
“I mean, it’s pretty hard for an able-bodied person to relate to someone in a chair. I couldn’t when I was on my feet. Never gave it a second thought. We tend to talk among ourselves about these things. I mean, we can relate to those things, where possibly you couldn’t. You’re a ‘spinal cord’; well, people here have more or less the same problems: pressure sores, muscle spasms, things like this. Just like it is between Marines. You’re a band of brothers, no matter if you’re a clerk, a baker, an infantryman, a tank driver, no matter what, you are still a Marine. You’ve had the same training.”
My next question was stupidly “able bodied”: Do you have any long-term goal or aspirations?
“You have to realize that I retired from the military and I’m service-connected, and I’m on Social Security now. I have no desire to go back to work. Right now I want to get healthy. I’ve got a lot of health problems. And that’s my goal right now. People don’t realize what happens till it happens. Being paralyzed is indescribably traumatic, to family, to your friends, you know; your previous friends just don’t know how to approach it. They can’t visualize — most of ’em just go away. When you get out in the community, there’s a lot of prejudice against people in a chair. When the average person sees someone in a chair and an able-bodied person is with them, they tend to talk to the able-bodied person and not to the person in the chair. You find this in restaurants quite a bit, when the waiter or waitress will come up and they will take my order from my wife. I’m not brain dead, you know.”
I can see the effect of “no muscles” on the shape of John’s lower trunk, where, with nothing resilient to hold in the insides, his abdominal wall bulges like a ubiquitous rupture; I notice — and am surprised — that he is not strapped in.
“There’s a reason I’m not. Normally I would be, but because of health reasons I’m not. I’ve got what they call heterotopic ossification of bone. What it is is my body thinks my bones are broken. To understand that, take yourself, say you break a bone, your body manufactures calcium and sends the calcium down to the broken spot to heal the bone. Well, HTO, which is common in quadriplegics and paraplegics, okay — about 50 percent of ’em get it within a 50-month period after injury. My body thinks every bone in my body’s been broken, so it’s trying to make new bone all over my body. Look at my knees.”
I note one appears fairly normal size, the other shrunken.
“Feel this one.” The larger leg is not flesh. It feels like a hardened cast. “That’s all new bone where it shouldn’t be. Now feel my hip.” He adjusts with a grunt. I touch the bulged area near the hip. It is solid and grotesque in size. “Now, push here.” He points to the opposite hip. I touch with hesitancy. “Push.” My fingers sink in as if I were gutting a fish.
“That’s what I’m here for now, waiting to see if they’re going to operate and remove my hips so I can set — ” he adjusts, grunts — “so I can set right.”
Later, I would talk to an orthopedic surgeon who would explain to me, in graphic terms, the procedure: “You just go in there and start sawing. I was involved in one once, and by the time it was over the room smelled like a barbecue pit.” He also explained the seriousness of the result. “A wheelchair patient really needs his legs and hips, for support, even if he can’t use them. The surgery is done with reluctance. The result is that the torso must be placed in a molded bucket in order for the patient to sit.”
One last able-bodied question to John: Did you see Born on the Fourth of July ?
“No, but I’ll tell you what. Kovic, to me, is nothin’ but a wimp. That’s all he is, he’s a wimp. First of all, no one pressured him to join the Marine Corps. And I can tell you, as a 17-, 18-year-old kid, he was probably chompin’ at the bit to get to Vietnam. So now he cries about it. It was everybody’s fault but his.”
They dumped the stuff out of the sky and onto the jungle like it was a great weed patch — and I was one of the ants....
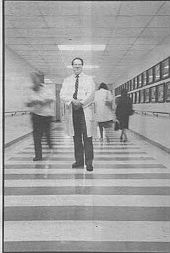
“Mention Agent Orange,” says Dr. Arnold Gass, “and I’m the one who examines you. No one else examines for Agent Orange.” Gass is San Diego-VAMC’s appointed environmental physician. There is one in each of the VA’s 172 medical centers. The responsibilities of EPs are to oversee not just Agent Orange-related issues but also those dealing with people’s exposure to nuclear radiation (atomic bomb testing or actually having been in Hiroshima or Nagasaki). Public awareness, however, is centered on the herbicide.
“What I do explicitly is, if a veteran wants to be assessed for his general health or for a specific problem that he thinks might relate to Agent Orange or is applying for compensation, then he signs up and comes in for a full hour with me, and we do a complete history and physical and laboratory tests, X-rays, and then I give him my personal assessment of his health.”
Dr. Gass appears to be in his late 40s, sports a casual dress shirt with bolo tie (clasp decorated in Southwest Indian motif), and seems absolutely at ease about his job. “What I do is not any hidden secret in any way, shape, or form.” (On the wall behind him hang watercolor portraits, one, a handsome young man, elbows on knees; the other, an evocative image of a thin girl dressed in little more than nylons, hand draped over raised knee, other hand grasping a phallus-shaped object.)
I tell Dr. Gass that every civilian doctor with whom I’ve discussed Agent Orange has conveyed to me his unwavering conviction that the entire AO issue is a bunch of shit.
“They have to be very careful, because we have an aphorism in medicine: ‘Never say never; never say always.’ Okay? So, absolutes can’t hold water in medicine, and that’s true in this case as well. There are people who got sick from having herbicides sprayed on them in Vietnam. The only illness that we know of in man that is definitely linked uniquely to Agent Orange is linked to the dioxin, which is the contaminant in one of the two chemicals that is used to make the compound. And that illness is a skin rash due to the chlorine. Therefore, it’s called chlorine-acne or chloracne. The Germans [in the 1950s] demonstrated that you could cause chloracne by painting increasing concentrations of the dioxin on people’s skin.”
What exactly is chloracne?
“Chloracne is a rash that looks just like bad adolescent acne. It has some unique qualities related to the density of the lesions and where they’re distributed on the body. And it’s known to be caused by exposure to the dioxin part of this contaminant in Agent Orange. But the question is, what about all of the animal experiments in which dioxin has been given to various species of animals and they’ve gotten all of these horrible things that are always listed in the articles?
“The answer to that is that the thing we know about dioxin is it’s very species-specific, that it causes different things in different species. And the only way you can actually answer the question in men is to actually have exposures in men. And those exposures have occurred, either accidentally or deliberately.
“And it’s happened industrially. The most notable accident happened in Italy when a chemical plant exploded one Saturday afternoon. A plume of smoke went right down the valley, and it contained this dioxin. So epidemiologists went in and studied people using mathematical models along the cone of this cloud. In theory, the people closer to the factory should have had more disease. They didn’t discover much of anything — except an increase in skin irritation.”
Having actually been a grunt (sleeping, eating, living) in the jungles along the DMZ of Vietnam when defoliation operations were being conducted heavily, should someone like me ask to be examined?
“I’ll be going against the party line, but I’ll say no. Because, ultimately, when you were done with the screening, I’d probably not say it wasn’t worth your time to come in here, but I would probably say that there’s nothing you really need to worry about.
“But the Marines had nothing to do with Agent Orange directly. It’s possible that some Marine groups were out on patrol or in the field, and a spray plane might have flown over, and they could have accidentally been doused with some of this spray. If they were, the chances are virtually nothing that they would have gotten sick from it, acutely or chronically. So my advice to you, personally, and to people like you, would be that it’s not necessary to come in.
“The biggest thing about Agent Orange that ever happened was that it destroyed the countryside in Vietnam. And the second thing is that it’s hard to know what it might have done to the Vietnamese people who are still there, particularly women of childbearing age. But that kind of information is hard to come by with any kind of the scientific rigor that we demand of our own studies in this country.”
I ask Dr. Gass to comment on the growing anger among veterans and veteran’s organizations who believe that the VA is stonewalling. He at first offers to provide me with copies of “official VA positions.” For a brief while, we discuss a few asides. Then, “As far as stonewalling, you have to understand, and this may sound brutal or standard party line, but it’s the truth. The federal government, through its division of veteran’s benefits, is very willing to compensate anyone who has honest diseases, honest conditions. The law says we must, and — provided you identify yourself to us and we agree with you — we do. The Agent Orange story, though, was very different. It’s one thing to have an eye injury in Vietnam, and, uh — ” (his eyes pause on mine) — “it’s pretty obvious. It’s another thing to say, ‘Well, I was exposed to this substance about which nothing is known, and I’m gonna blame every little thing that’s happened to me, both psychological and physical, on this substance.’
“Now, the VA’s tradition has always been to compensate based on scientific information. So what it did, when it created its regulations to compensate for Agent Orange, it said if a condition is proven, we will pay for it. And if it’s not, we won’t. Well, the Vietnam veterans took them to court, and the VA lost — two years ago in San Francisco. The court said the regulations are too restrictive, based on the law. What we’re going to require you to do is to revise your regulations and to compensate based on statistical associations for likelihood — not iron-clad, absolute scientific proof. The new secretary of the VA didn’t even bother to argue that. One of his first decisions when he got into office was to say, ‘I’m not immune to make that decision; we will comply fully with the law.’
“And so, they’ve been re-writing these regulations. Well, during the period of re-writing, no one’s getting any compensation at all, because they don’t know what they’re going to be regulating. So as soon as this is all done, they’re going to have to look at all 30,000 back-cases, plus all the other cases that have come up. That takes time, there are fewer people around to do it than ever before, but it will eventually get done.^*
"You talking about heavy W/M care?” asks Bob, head tilted.
I reiterate that I’m talking about “vegetables.”
“I’ve been here 19 years,” he then continues, “and in the nursing home program, we’ve only had one which we consider to be comatose, vegetative state, that I can recall. We might have had one other. One visibly stands out who was in long-term care; but actually, we don’t have any who are in the hospital right now.” Suzanne speaks: “There might be a few out there. There’s a gentleman now, for example, who’s on the psychiatric ward.
"He’s a Vietnam veteran, I think. He’s, like, an old head injury from 20 years ago, from shrapnel. He’s somebody who lived at home with his father, and now he’s gotten more agitated and more upset lately, and so he was run into a medical service, then transferred over to psychiatry. And we’re trying to get him out to a brain injury center in the community. Because usually, when people have been brain injured, the rehab period that’s most effective is right after the injury. It’s hard to make a change 20 years after a head injury. But there’s some reason to think that he could benefit from a few months of treatment in a brain injury program in the community. We’re probably going to be sending him out at VA expense.” Suzanne Demong is the VAMC’s chief of social work service. Bob Carney is supervisor/coordinator of community care programs. I had come to Suzanne’s office still curious about the fate of Johnny Got His Gun-types who return from wars decerebrated (or thought to be) and must be littered throughout the country — somewhere.
Bob continues, “Either they die fairly rapidly or they improve and become people like the man we were just talking about. Well, now there’s one nursing home which we have not made placement in for that purpose. It does have quite a few young, total-care [VA] patients. We use it for ‘locked’ and we use it for ‘regular skilled.’ But [the homes] get paid by the state, somewhere in the neighborhood of $250 a day to $300 for this type of patient.” Locked?
“Psychiatric-type. Now, we have some veterans in there that are mostly older, that are demented, although there are few maybe younger.”
“The reason being that,” Suzanne explains, “if you’ve had a severe brain injury, sometimes you tend to wander.”
Bob continues, “We have some young veterans, they’re 100 percent service-connected, like one, a tire blew up and damaged his head. We have another man who’s been in the nursing home about 17 years. He can’t talk, he has no control over his eyelids, things like that. He’s very incapacitated. And there might be a Vietnam veteran among them too. We don’t have a lot of them. Residential care is where you’re likely to find most of them.”
The difference?
“That’s where they’re living in someone else’s home that’s a licensed facility. Anywhere from 6 to maybe 150 who can get through the day but need to make sure they take medication, to prepare meals. It’s kind of a caretaker thing. Those would be veterans who have no family or maybe had some behavior that could not be tolerated in a family situation. Most of those with families are probably living at home.”
This is a large hospital, with a large bed capacity, yet I get the impression that outpatients constitute the greatest proportion of veterans dealt with here.
“I know,” says Bob. “A tremendous outpatient load. And of course, in general, medical care is moving this way. I mean, we’re kind of in the mainstream of how hospitalization or medical care in the country is going. ’Cause, actually, hospitals are paid, even as we are, on turning over, not keeping people. I know, historically, we [were] famous for keeping people.
“We used to offer any veteran coming into this hospital who needed skilled care a six months’ VA contract. That means six months the VA covered care. That’s now down to three months. And even that, even now, if a veteran can go another way, like MediCare, they will go that way.”
Rita C. Monteiro received her Ph.D. in clinical psychology from Wayne State University in Detroit. She wears a gray blazer (padded shoulders) over a floral-print blouse and conducts herself in composed, businesslike fashion. Monteiro is chief of the alcohol-and drug-treatment program, a significant slice of the psychiatric section in the VAMC. (According to Bob Stevens, the center is “pretty evenly divided, between medicine, surgery, and psychiatry,” an interesting aside regarding the demographics of today’s veteran population.)
Walking through the waiting areas of the ADTP is reminiscent of a stroll through a Greyhound bus depot. Most patients appear impoverished. Why?
Monteiro explains, “Because of the eligibility criteria. Basically, people who earn over a certain amount are not eligible to receive services here. It is a problem, because now insurance [companies] are cutting back on substance-abuse treatment. There are a lot of veterans who, while they may have jobs and earn too much money to qualify for [VA] services, don’t have the insurance to pay for their own service. There’s a large population of veterans out there who really don’t have anywhere to go. We’re concerned about that population. As it is now, the person has to wait until they’re almost destitute before they can qualify for service.”
And yet veterans can be rich and still qualify for VA treatment if they have a service-connected disability. “Yes. We do get those occasionally. And that’s good to have a mix of patients too, so that people who are destitute can see people who are doing a little bit better and that gives them more hope.”
How does an eligible veteran get involved?
“They come in for an initial evaluation in the outpatient program. They see internists, a physician who specializes in working with substance abusers, and receive a physical. Then we do outpatient detoxification; we don’t do inpatient detox. They receive a medication to help them, and then we send them home. They return every day during detox to see a physician and go to evaluation group.”
I ask about the danger of heroin addicts going home alone to try to detox themselves.
“Actually, alcohol detox is the most dangerous, along with all the other minor depressants. Depressants, period, are more dangerous than all the other drugs. Heroin detox, the person feels worse than they might with other drugs, but there’s no real danger of them dying. Alcohol detox — we have to be very careful, because they can have seizures or convulsions from the withdrawal. Typically, our physicians use a Librium-taper detox protocol. They give them a decreasing amount of Librium each day. It’s a minor tranquilizer. The medication helps them gradually withdraw, rather than all at once.
“They go to evaluation group, they see two therapists who talk to them every day about what’s going on and try to determine what type of treatment they need. One good thing about having the outpatient detox is it does help to prevent people who are not motivated to really stay drug free from abusing the services, if they just want a bed to sleep in and not really want to stay drug free. You have to be fairly motivated to continue.”
Many repeats?
“The government allows you only two admissions to inpatient treatment; outpatient treatment — as often as you like.”
I ask Dr. Monteiro to explain the inpatient program.
“Once they finish the evaluation group, and [if doctors] decide it’s inpatient treatment that’s indicated, then they actually get admitted to the hospital'. They stay 28 days, and it’s a very intense, active program. That’s why we have them detox first, because when they come in the program they need to be alert and coherent and willing to participate. There are education sections, group-therapy sessions, skill training sessions, all day, every day.
“They learn about alcohol and drug abuse, its effects on you. Psychological and physical effects. We have people from psychology, people from social work, people from the community who come in and speak; we also do some movies. Vocational Rehab does a lecture on vocational resources. In therapy group, they talk more intensely about their own substance problem, every day.
"They have relaxation training sessions; they have a leisure skills utilization group done by rec therapy, telling them how to do things that are fun and enjoyable without getting high. And they have outings. ’Cause typically, these are people who, everything they do is associated with getting high. We have community college instructors. One does a communications course, one does what’s called ‘personal growth,’ but actually, it’s assertiveness training. And one does a sexuality course.”
What percentage of the patients are women?
“Very small. It’s about two and a half percent. We expect that will increase, because now there are many more women in the service. It seems like it’s already starting to increase a little bit. Already this fiscal year we’ve had as many as we had the fiscal year before. But a lot of women don’t even know, for some reason, that they can use the A. I don’t know why, but they say, ‘Oh, we can come there? Oh, I didn’t know I could come here!’ ”
Hell was less a place than a vortex, undulating, thrumming, the eternal disintegration of my being into conscious atoms. Think the shrinks call it “disassociation.” Wouldn’t know, though. Never been to one. Tried once (last year of college) when I used to drive around with a loaded deer rifle in the trunk of my Mustang. Dialed the VA and said, “Got a problem.” They said, “Oh, what?” And I told ’em. They treated me like there was something wrong with me. So I said screw it and never went. Didn’t matter. I figured out later (years later) it all has to do with power — like God’s. Today they call it post-traumatic something or other. But that’s for people who haven’t figured out the power.
Like when my best civilian friend got killed driving my car for something I got him into.
After it happened, I drank for two weeks straight, then jumped a plane for Dallas and the only buddy I know is still alive from my old platoon. (He was with me the night I got wounded; was the only one who’d crawl out in the dark to get my sorry ass.) So I went to Dallas. We took rifles and drove into the desert and shot lizards and horny toads. He was married with two kids. But we both agreed it felt good.
Then, years after that, I’m a respectable person, got a good teaching job, coach football. It’s homecoming. We’re winning, fans are cheering, wind is blowing, and the moon ... the fuckin’ moon ... is as big and round and ugly as a dead man’s mouth. Keith Jewett — two days past 18 years old. I’d recruited him when he was in junior high. Had to do a lot of talking too, ’cause his mother was a nurse, and she was afraid he’d get hurt. “Don’t worry,” I told her. With 7 minutes and 35 seconds to go in the game, he dropped dead. Like any coach worth a damn, I loved the boy. And all I could do was stand and watch this mother give mouth-to-mouth to her son while a doctor slowly shook his head. Next morning I load my rifle. Think about it — but don’t do it. Just hold it and feel better in the knowledge that once upon a time I’d played God and taken human lives without any thought whatsoever and, if ever I want, can do it again. That’s the power.
I think about this sitting in the “nut ward,” waiting to interview some Ph.D. about post-traumatic something or other. Most of the people here look as normal as any other unemployed person (basically, tired and poorly dressed), but there’s a couple looney toons around here. And I think about the smell of this place (that hospital smell) and my vision of hell at the age of ten.
Fifth-grade recess: Me an’ the guys have taken over the swings from the girls, not to swing (hell no!) but to jump. Whoever jumps the farthest has the biggest balls. I’m pretty much the champ at this event (largely because I’m no good at baseball), and I have that swing swooshing as high as the crossbar. The trick, see, is to jump on the way up (so you sail out), but I hesitate — and drop like a B-52. Mrs. Moen thinks I’m laughing (until she sees my hand where my elbow should be). By the time Mr. Bashaw gets me into his station wagon and to the hospital (arm splinted with the halves of a broken yardstick), I am delirious. They give me a shot and wheel me under a lamp big as the sun. They place something on my face and begin dripping ether.
The first few inhalati'ons are like sniffing rubbing alcohol.
Then the droning begins: consciousness alters and darkens, like being drunk while someone bricks you in. Each breath sends a surge of prickles from head to toe, then evolves into slithering buzz (like worms crawling in your mouth) until it becomes you, disemboweled, disembodied, exploding into infinite atoms — orange, black, spinning, buzzing — whirlpooling into a writhing esophagus with no entrance, no escape, unending, a sinuous tube of eternity, consciousness of the damned, satanic chant... TOO late, TOO late, TOO late, TOO late....
"Have you had mental help from the VA?”
What?
“I know it’s a personal question, but — ”
No.
Jeffrey Matloff looks like a young Al Pacino playing the role of a clinical psychologist in a movie called Flashback and Bad Dreams; instead, he really does have a Ph.D., and clinical psychologist is his real job.
“You’ve had some exposure,” he says, “just sitting in the waiting room and seeing the kind of population we get. It varies quite a bit. You have people with drug or alcohol problems coming through here, people with acute psychiatric emergencies, people who are just part of the normal client-mode. What would you like to know?”
About post-traumatic, uh....
“Post-traumatic stress disorder, PTSD.”
I ask him to explain it.
“PTSD developed basically with the recognition of the Vietnam combat veterans, in addition to other groups, who have gone through a horrific experience recognized by all as being outside the realm of normal human experience. For instance, concentration camp survivors from World War II also were a group prone to experience these so-called PTSD kinds of problems. Certainly being interned in a prisoner-of-war camp might be another. It carries several different types of physiological and behavioral responses. Some of the symptoms are nightmares, kinds of intrusive thoughts — flashbacks, if you will — from some of the events. This can happen months, even years after the initial event was experienced. Basically it’s considered ‘shorthand’ — the normal reaction to abnormal events in one’s life.”
Normal?
“Certainly. Painful war memories and dreams, even long after a war, are normal. The big thing you want to look at is how is it impacting this person. I mean, there are guys from World War II, for instance, who may very well have symptoms of PTSD but who cope pretty well. I think if we look cross-culturally, warriors, in whatever culture, many of them probably have symptoms. What we oftentimes see is a kind of numbing, a turning off, withdrawing, not wanting to get involved with people. Sometimes you’ll see an inability to hold jobs, interpersonal relationships will be greatly affected. I think the big difference with what happened in Vietnam, compared with what happened in other conflicts, was the homecoming our warriors received.”
Dr. Matloff openly admits (to his patients and to me) his role during the Vietnam war. “The guys you read about, in the streets, protesting, that’s where I was. And, let’s face it, the homecoming for you guys was really not very good. Basically, society has learned that this is not the way we should treat our warriors, the people who put their asses on the line.”
What happens when a patient brings up something he did that was criminal, like, maybe, he fragged somebody? That ever come up?
“Uh, not frequently.”
Or he accidentally killed a buddy? Or is it, as they say, doctor, just the experience of combat itself, the overpowering magnitude of war and the inability to assimilate the experience into daily life? That it?
“It’s some of that. Oftentimes, though, it gets down to very personal vignettes. Could be things like somebody who talks about not being able to save a buddy and harboring that kind of guilt; listening to their buddies scream and falling asleep with that kind of thing at night, you know — things. Intrusive kinds of things. Or.maybe coming across a civilian who they thought may have been a VC — something like that.”
(I remember once trailing two Vietnamese males, early 20s, smokers, waist-long hair, sneering and muttering in gook, around a Safeway store, me whispering to ’em bu'koo DOW! bu'koo DOW! and hoping they’d shit their pants — something like that.)
“Or maybe having to shoot somebody who was, yes, ‘unfriendly,’ but conceivably, you know ... you remember from your training you weren’t trained necessarily to shoot women and children and things like that.”
(Not necessarily, correct.)
“The thing to remember is that the dreams and the flashbacks, to some extent, are normal. It’s when they start impacting one’s life in terms of, you know, causing problems in relationships. One of the things we see in Vietnam veterans is that many of them have relationships that are strained or nonexistent. Where they’ve had multiple relationships, generally very shortlived. That’s typically one of the problems for folks that start experiencing problems with PTSD.”
Why does it happen? Is it the inability to communicate about something impossible to communicate?
“Yeah, there’s certainly that. And the whole thing about getting close to somebody and then losing them. Abandonment. You’ve gotten close to people in the past who are no longer around. And, you know, those kinds of feelings of loss tend to keep somebody pulled back in. Plus, ‘Who could ever understand the kinds of experiences I’ve been through,’ and ‘If I start to tell people, I’ll blow them away with the kinds of experiences I’ve had.’ ”
So how does somebody end up in your office?
“Generally by the time somebody sees us, we’re pretty clear that they have been exposed to combat, because that’s fairly easy to detect from their discharge, their DD214. As for how physically they get here, sometimes they come in by themselves. Oftentimes they’re dragged in by a spouse, if they’re married, or a girlfriend or a family member who might say, ‘This person’s not communicating’ or ‘He lost another job,’ things like this. Then again, maybe they got referred from some other department. They may have another problem but not admit, if you will, to having this particular problem.”
Do you have a “typical” patient?
“I can’t really talk about specific patients, but generally, what I see with a lot of folks, the folks who may actually have PTSD, is there’s a reluctance to admit to having it.”

It dominates the hill like some neo-Roman rebuild of an ancient Greek acropolis, covers it, a dozen crossed layers of cream-colored cake and tinted glass. Across a spreading slope below, spangles of sunlight bounce through a ripple of breeze-blown trees in a lake of parked cars. Nearest the building, empty buses idle.

Walking from a far corner of the visitors’ lot, I approach the main entrance to the Veterans Administration Medical Center, San Diego. It overlooks La Jolla Village Drive and a long stretch of I-5.
Strangely, it looks less hospital than computer plant. A few old men sit at the steps, waiting, their faces frozen, deeply creased, like living gargoyles.
Passing the old men (their eyes as silent as their mouths), I come to sliding glass doors — opening, closing, opening, like heart valves — and slip inside. First sensation is smell; then a sickly memory that always follows. (This time, I think of being ten years old, receiving the only enema in my life.)
A 50-ish man of 300-plus pounds exits the building in an electric wheelchair. He resembles Jabba the Hut and sports a black cap with “Old Fart” emblazoned in bright orange. A scarved woman of equal weight but considerably less height escorts him out the door.
In a cubbyhole office, a black security guard sits studying his hands. At a silent signal, his eyes lift and pause with suspicion on mine. I move away from his gaze and stand in front of a portable bulletin board announcing classes on proper nutrition.
Across the lobby, clustered by a semienclosure of tables, four elderly men laugh. I approach the one sitting sideways behind the front table; his right arm rests on the tabletop. Scars reveal that the hand had once been butchered and later sewn together into three grotesque fingers. White letters on a shiny-black tag declare his name — JIM. Jim looks up and smiles at me with the honest sincerity of my father.
“Yes, sir. Can I help you?” he says.
Public relations isn’t my normal duty,” explains Bob Stevens, whose title — administrative assistant to the medical center director — is as broad as his job. “I provide administrative support to the director on any and everything he has to do, all the reports and contracts, I run the medical staff office, and then I do facility planning, coordinating all the movement, projects, things like that. Our public relations person is out on maternity leave. I’m just covering that while she’s gone.”
Slight of build and soft-spoken, Stevens handles himself with an air of adroitness. Everything about him is conservative: knit V-neck vest, cotton shirt, dull-blue striped tie, wire-framed glasses, mustache that’s scarcely visible, and hair (receding, thinning, graying) parted on his left. Number-three man on the administrative side of the house, Stevens is fairly high up this “corporate” ladder. (His office has a window — with a view.)
Overall, however, he’s a small part of an incomprehensibly complex bureaucratic machine. The Veterans Administration is the second largest federal agency and employs one of every eight fulltime government workers. San Diego’s VAMC is just one of 172 such medical centers.
I’d come to his office to arrange a quick tour and set up some interviews. But I also came as a veteran. A combat veteran 60 percent disabled in an ambush 22 years ago. I have been to the Wall (Vietnam Veteran’s Memorial in Washington, D.C.) and read the names of those I knew would be chiseled in. And I found the names of others I didn’t know would be chiseled in. But more startling, there were guys I’d seen horribly wounded whose names I’d expected to be there — that weren’t. No doubt, some of those boys returned home, healed, and today are just another middle-aged Joe on the job. But what about guys like my platoon sergeant, Staff Sergeant Blankenbaker — who got most of his head blown away by a mortar round? His name’s not on the Wall. Where do they keep the vegetables?
Stevens looks at me benignly. “Before I came here I was at Fort Lyons. It was strictly long term. And there are others in the A system that specialize strictly in the long-term care. In Colorado we had a unit that was totally, you know, what you call vegetable-type patients that have been there for 10 or 15 years. They’re totally fed by a tube. They’re just — they’re vegetables. In a layman’s term, that’s all they are. And they’ll be there till they die.”
Vietnam wounded?
“Yes.”
Head wounds, mostly?
“Yeah, mostly.”
I’m the chief of voluntary service. That’s my title,” says John Stewart, a big, broad-faced man with a thick swoop of dark hair, a rapid-fire manner of speech and a physical demeanor that suggests the street-tough loyalty of a Sicilian bodyguard. High on the wall behind his desk, prominently displayed away from an adjoining wall covered with plaques and certificates, hangs an autographed picture of George Allen.
“I’m a native Californian, and when the Rams fired Allen, it made me mad. So when he moved to Washington, I started following the Redskins. And then by fluke accident I got transferred to Washington, D.C. — in fact, that’s where I trained to be a voluntary-service chief. George used to bring Sonny Jurgensen and Billy Kilmer to the hospital every year to visit the patients.”
I ask Bob if he is a veteran.
“I’m a Vietnam-era veteran; I was in during Laos and stuff like that, and I was in the Air Force, so I’m not one of these guys going on the front lines getting shot at. There’s a lot of difference between getting shot at and sayin’ you were in the war.
“You'll probably find a rule, it’s kind of an unwritten rule. The people that bitch the most probably deserve the least, and the people who bitch the least — probably we owe ’em everything. Just like some of my volunteers are also patients, outpatients, and they represent various wars. There’s a guy sitting out here at the front desk that’s a leg amputee, a World War II pilot. His name’s Jim.
“Another guy, this guy’s a Congressional Medal of Honor recipient — means he did something. It’s the highest award the country gives. And here he’s over in Vietnam, and he was a sergeant, and supposedly he literally went back and forth carrying his men one at a time off this hill where they were surrounded and being shot at by the Vietnamese, and he got shot himself. He did this, comes home and gets the highest award, and then he rolls in here and his diabetes causes him trouble, and they’re deciding to amputate his leg. Well, he was always in here happy, and flirtin’ with my secretary a little bit, and kiddin’ me a little bit, you know. And he coaches football out here at one of the high schools. And he’s in a wheelchair, then all of a sudden he’s walking — he’s on crutches but he’s just gettin’ where he’s off the crutches and he’s starting to walk on his own a little bit. And he’s always been so upbeat. He’s just the nicest man in the world.
“Then you have somebody else, say they were in basic training, had a nervous breakdown, and they come through the door and say, ‘I’m a vet’ran. You owe me!’ Or somebody gets on drugs, wants to blame the military ’cause they got on drugs. Well, you know — there’s no comparison.”
Lot of people try to milk the system?
“That’s true. I’d been a therapist before I got into this job. I’ve been in the A over 20 years. And I told my dad one time, ‘I’d like to have a job where I just went from hospital to hospital acting like a patient and uncover the people that are milking the system.’ He says, ‘Yeah, and you’d wake up in the alley with your neck slit sometime.’ And he’s probably right. But how many times do the government and the taxpayers owe a person to go through the detox program? One time? Twice? Ten times?
“I worked in Danville VA hospital as a recreation therapist, and one of the guys I had there as a patient — nice guy, don’t get me wrong — was in and out of that place for alcoholism. Not once, not twice, maybe three times. Then I left there and went to Washington, D.C. Then I went to Omaha, Nebraska, and then to Westside Chicago. My first day at work at Westside, I walk in and I hear this guy say, ‘Hey, Stew!’ And I turn around and here’s this same guy. Later on I transferred across town to Hines — here’s the same guy. So that means that this guy’s been in three of the hospitals that I’ve been in, see, and treated in every one of them for alcoholism. I think he’s probably dead by now. Probably drunk himself to death. He was a nice guy, but how many times do the taxpayers owe a guy like that?”
Charlie, an ex-Marine, looks dead on the narrow bed; long forearms and liver-spotted hands limp upon his chest, old fingers intertwined. The sleeves of his dark-crimson pajamas are shoved to the elbows — like a man unafraid of work. Top’s unbuttoned, splayed to the sides, and a still-strapping torso breathes silently in a white T-shirt. I touch his forearm.
“Mr. Deasher?”
His eyes open slightly. He shows no alarm. No concern.
“Remember me?”
“Who?” he says, unblinking.
“I met you at the front desk. You said I could interview you.” “Oh. Okay.” He closes his eyes and swallows. “Okay.”
His front teeth are gone, the gums purple. I start lightly: Tell me about yourself.
“I’m legally blind.” (His eyes remain closed.) “My job as a volunteer now is I work at the front desk, and tell people as they come in how to get to different wards, like to X-ray and eye clinic, and where to check in, ‘I’ve never been here before....’ Things like that.”
What’s your surgery for tomorrow?
“Routine eye surgery, which is number 13 eye surgery. Damage from the war and the atomic bomb.”
You saw Nagasaki when you were a POW?
“Yeah.”
Would you tell me about it?
“In the first place, I was too tall to work in the coal mines. I couldn’t walk through the tunnels. So I tell ’em, ‘Me farmer boy — cut weeds!’ Damn if I didn’t get a job cuttin’ weeds. The hell, it’s hard work though. And this particular day I was cuttin’ the weeds, and the guard was up there with me, and I noticed a lot of American planes, carrier planes, to the south of us. And about that time, the civilian guard decided he had no place to be up there on that hill. He bugged out. So I sat down and watched the airplanes. He left his lunch pail with little rice balls with the special insides in it, which was not too bad. And so I was sittin’ there just watchin’, and then I saw the blast.
“It was just like the picture shows. When it went up it was brown, and up like that,” he separates his fingers and gestures with his hands, “and mushroomed, then come back down.”
When I ask him about being taken prisoner, his eyes open, and he lifts his head.
“The United States Government knew many, many weeks before the war started, before Pearl Harbor got hit, that the Japs was gonna come.” He lays his head back. Closes his eyes.
“When they hit the Philippines Navy yard, they killed 2500 civilians out of 7000 civilians, and one Marine, and 130 service that I know of, plus all the ships that went down, and all the men that went down with the ships, which we’ll never know how many men it was.”
How old were you then?
“About 30 years old.”
How old are you now?
“I'm about 78. I’ll be 79 in November.”
Were you in the Death March?
“I didn’t make the Death March. I was on Bataan when Pearl Harbor got hit. I come back to Clark when it got blowed off the map. And then the colonel called. See, I had the motor pool, I was in charge — corporal. The colonel had me go to the Navy yard to assess the damage. Why, then I come back with a pickup truck and hauled the injured.
"This ensign took ’n’ helped me with the injured and put ’em in the truck, and we took ’em back an’ forth to the hospital three miles away. That was a bad mess. The town and everything was all ruined. There was so many dead and everything. Then we went all the way up to Bataan for some time before we went over to Corregidor for beach defense.”
How were you taken prisoner? “Capitulation. We stood by, and [the Japanese] brought soldiers up, destroyed our weapons, an marched us to an enclosure, what they called 92nd Garage. A very infested hellhole. They had dug holes with tractors for defecation. It was really a bad situation.
"There was malaria and pneumonia and everything like that. I was put on a workin' party, and I had to go out in the water an’ pull in the dead Japanese soldiers — the ones that had the sabers and leather belts and stuff — to pull ’em in on the dry land, and then I had to strip ’em, strip the leather goods an’ all that stuff off the dead Japs.
“And then they set us underneath the tree there t’ take a break. And ’course I knew the island perfect, and I went over the top of the hill. We went an’ hid out in some caves I knew was over there. And then when it started t’get little toward evening, I went up by the water where I found me a bucket and got a pail o’ water ’n’ come back t’ the [POW] camp through the gate an’ back in the enclosure where it’s safe. It’s all tricks o’ the trade o’ survival.
“Then they took us to Manila, put us in cattle boats, stuff they put horses in, things like that, and then dumped us out — some places in three-foot water and some places over your head. We swam to shore, an’ then parade us up ’n’ down the streets of Manila. They put us in prison overnight, then moved us on next day. That group I was in stayed in the Philippines six months, then we disbanded and they shipped us to Japan.
“They kept us in the holds. Too many people. Most of the ships was torpedoed by the American torpedoes — submarines — because none of ’em was marked with ‘Prisoners of War,’ an’ that’s where a lot of our prisoners was killed. They wouldn’t let us come out an’ be identified, an’ they lowered buckets down to put our — what ya call — bathroom facilities, an’ they pulled it out an’ dumped it over the sides, an’ then run it back down to us again. They spilled it on us ’n’ made a hell of a mess of it. Very unsanitary.”
I notice that the tips of most of his left fingers are missing. How?
“Well, I was just an on’ry old sonofagun, a farm boy — five’n’half years old. And I just took a dynamite cap over at grandmother’s place. I took ’n’ hit it with a hammer, an’ the damn thing blew up. We was right there on the edge of the desert, an’ we used to chase jackrabbits, an’ play with the snakes, catch monkey-faced owls and give some o’ the stuff t’ the San Diego Zoo. Then later I was a lineman, worked for the power company, climb poles up to 55 feet, stringin’ wires an’ stuff like that. Learned all kinds of tricks ’n’ trades. Bailed hay. Pitched watermelons. I’d work with the green-card workers’n Imperial Valley there, side by side with ’em. Thinnin’ lettuce, 17 cents an hour. But we didn’t starve.
“Depression in the ’30s, we had a big ol’ garden. We sold about 1500 rabbits a year. And my brother an’ I, we had bees, 50 colonies o’ bees. Then the boss’s wife went ’n’ gave us some peacocks. We saved the big ones, the males, because they shed them big ol’ long plumes, looked pretty. The hens didn’t look so pretty so we ate them. Ate a lot of ’em. We never did starve.
That’s — that’s survival.
“Like in prison camp — Osaka. I traded. Some o’ the tradin’, I got grasshoppers — ’bout two inches long. We use t’ eat them grasshoppers. They was good stuff. ’Cept the legs bothered me. I had t’ kinda chop ’em up a little bit because they hard on your mouth t’ eat. But I’ve eaten a little bit of ev’rything. Ate whale blubber in prison camp. Oh, you just name it. If it isn’t poison, I’ve ate it.”
Charlie gets quiet, like it’s time for me to leave. I start to get up.
“All three of us brothers was missin’ in action at one time. I was prisoner o’ war; my brother was bombardier, an’ he went down. They run outta fuel. My other brother, when he went down ... he ... they didn’t even find his body. In the Pacific.
That’s where all of us were missing in action at one time.
“I never earned a Purple Heart. Oh, I had a few little scratches ’n’ burns ’n’ too many bombs dropped too close to me. I lost one staff car. Bomb missed the front bumper ’bout three feet, an’ I lost that. It burnt up. I was just 30 feet away, and it didn’t bother me at all. See, I always ran uphill where the soft ground was, never down the road. You on a road, the bomb hits, an’ shrapnel’l git ya. If you’re on soft ground, it goes in the ground ’n’ you don’t get hurt. It’s all tricks o’ the trade of survival.”
Here, in SCI...”
(Even the acronym feels like an unwashed finger down my throat. Can’t swallow. Sticks in my gullet. Piece of dead meat. Lobby area is twilight dim; refraction of brick and uncarpeted concrete, clean, polished as lacquered bone. Can’t swallow. Flickers of living corpse in forgotten moment. Receiving ward, Guam, 1969: boy on the gurney beside me’s not doin’ so hot. Wound in the back of his neck is small, but he’s paralyzed from there down. Compared to him, I’m fine. Earlier he’d said, “They told me it’s just temporary.” I wonder. Now his guts are cramped, but he can’t do anything. “Doc!” he says — we always call a corpsman Doc — “It hurts!” Corpsman asks him if he wants a “massage.” Boy says he does, “But hurry!” Corpsman’s calm as a clock. Done it before. Room is mostly dark — other gurneys in here, guys quiet in pretend sleep. Doc brings something over that glints in the light from the nurse’s station and starts digging soft and easy-like under the boy’s sheet, lifts him like he’s making a bed, says things like “ ... There we go ... How’s that?... All right!....”)
“Here in SCI...” she came back into view like a sunlit face through a screen door, brown hair and soft features, gentle voice, “ ... I’m responsible for new staff, nursing education, consulting with nurses about problems with the patients that they may not have the expertise to resolve.” Her name is Cathy Dunn, clinical nurse specialist, Spinal Cord Injury Unit. “I do a lot of counseling, particularly sexual counseling, and I do lot of consulting with patients in the main hospital that have rehabilitation needs, but I’m necessarily spinal cord injury patients.”
The SCI unit has been open for just two years, although it had been planned for more than 15. Money — funding approval and a bid within budget — held it up. There are 23 SCI units in the VA system.
I’m curious about her reaction to Oliver Stone’s movie Born on the Fourth of July.
“Some of the things depicted in Fourth of July were fairly accurate in the way that many VA hospitals were in the early ’60s and mid-’70s. Some of the film was exaggerated, because of where Ron was during that time, emotionally. I think that some of his memories of what it was like are a bit exaggerated. And in comparing the book to the film ...” (How many other people, I wonder, read the book for comparison?) "... it’s more exaggerated in the film.
“There are a lot of things that were in the film that are not done that way at all anymore in the VA system. For example, the one scene where they have all the guys in the room together having enemas. That’s something called the blue room that some of the old VA hospitals have.” (I recall an ugly old nurse shoving a tube up my ten-year-old butt.) “We have a blue room. We were made to put one in, but we don’t use it. We have individual bathrooms. Patients have all of their showers and that kind of care in the bathroom in a private area. But we don’t give enemas anymore.”
Not necessary?
“No. In fact, giving enemas over a long term can cause a lot of patients a lot of problems. We’re dealing now with the results of guys who used enemas for 20 years. They do use a technique to empty their bowels on a regular basis so they don’t have bowel accidents, but it does not involve using enemas.”
I tell her about the boy in Guam in ’69.
“That’s called digital stimulation. It’s using a finger to stimulate the rectum to relax and let the stool come out. Most of our patients have no voluntary control, but part of what we do with the patients is set up a program where by using different techniques they have control over when their bowel does empty.”
Do any patients choose to have a colostomy?
“Very rare. That would be in an extreme case, and in fact, the ones that we’re seeing using colostomies now are the guys that used enemas for years and damaged their intestines by doing that.”
How do you handle the despair? “It takes a certain type of person to work on a unit like this. Not everybody’s happy working on an SCI unit. I think that it takes a kind of person who can step back and knows when to push a patient to do as much for themselves as they can and yet be very supportive about it. You have to be able to switch your approach for the individual, because they’re not all the same. Not every SCI patient has the same personality or interacts with people in the same way. You have to interact with them as a person first. You kind of have to be a combination of a cheerleader and a whip cracker.”
(I remember a “whip cracker” and a guy across the aisle on the eye/amputee ward in Guam. He looked like someone who once was president of his high school’s science club. Every 15 minutes or so, he’d start babbling like a baby, disturbing everyone else. Pretty soon this nurse — who I later read about in Reader’s Digest — would storm over, tell him to knock it off, tell him to grow up, tell him to quit feeling sorry for himself. Both his legs had been blown off, his right arm at the elbow, and his left hand. And, like me, he’d been blinded in one eye.)
That paralyzed boy in Guam, I reminded her. He said they told him it’d only be temporary. Could they have known that?
Cathy looks at me straight and says, “They shouldn’t have said that.”
"I’m a lover, not a fighter,” quips a man prepared for the inevitable reference to the long-dead pugilist. Yet the way he’d sat up in his wheelchair and proudly articulated his name, “John C. Sullivan,” told me something. Sullivan may indeed be a lover, but he sure as hell is a fighter. His resemblance to John Wayne is almost scary. If he could stand, he’d tower over me; his neck descends from the ears; his lips press together stoically; his square jaw and Corps-cut hair mark the quintessential face of everything that’s not wrong with America. So, I wonder, what’s an old jarhead like him think about today’s Marines?
“You have to realize,” he says, turning and rubbing his clean-shaved jaw, “the difference in central values. I think today’s Marines are just as good, if not better than when I came in. All the troops I worked with were fantastic. I came in in 1956 as an infantryman, made the Lebanon landing in ’58, was in Santo Domingo in ’64-’65. Then I figured out it was easier to fly over mountains than walk over ’em. So I re-enlisted for aviation. Was in ’Nam in ’70-’71; rather, we were in country — but we weren’t. I was with electronic warfare craft, so we was back an’ forth from Japan and Danang. Nixon was pulling everybody out, and theoretically we weren’t supposed to be there. At the time, I was an ejection seat mechanic and anything else regarding pilots’ life-support systems.”
Ironically, Sullivan’s paralysis occurred as an indirect result of his military expertise. “I retired in May of ’85, and I took a job with a civilian corporation that had a contract with the Navy. Basically, I was to do the same kind of work I’d done in the Marine Corps. This was at Kingsville, Texas, where they train naval pilots.
"These young pilots had just , gotten their wings, and we were at a buffet party-type thing, and I was swimming laps in the pool. Two of the young guys picked up one of their buddies and threw him into the pool, and he landed on my back.”
Under normal circumstances, the blow should’ve resulted in little more than a temporary loss of air (and a few words). The circumstances, however, were not normal. “I’d had symptoms for almost two years, but the doctors kept telling me it was muscle strain.”
What symptoms?
“Sudden loss of bowel and bladder control, difficulty in going from a prone position to sitting, getting out of bed, off the couch, and tingling in my hands.
“I’m not downing the quality of the medical facilities, but all they had there was a clinic. And these people were just general MDs, mostly. They didn’t really investigate my problems as thoroughly as they should have. It wasn’t until after the accident that they discovered I had a cancerous tumor. What the tumor had done was it had crystalized my spine in the upper thoracic region. You know how flexible a bone is in your spine — the tumor had made it very brittle. When the guy hit me, the bone just shattered like glass. It drove a perfect piece of bone right through my spinal column.
"Severed it. I’m paralyzed just below the shoulders, right at the armpit level. And, due to other complications, my injury is going higher. I’m losing control of one arm and probably will lose control of the other.”
Is the cancer gone?
“They’ve got to wait five years to declare me completely cured, but I’m confident. I’ve had three operations, first when they went in to remove the piece of bone from my spinal column. That’s when they discovered the tumor. And two more since. I’ve had radiology, then a year and a half of chemotherapy. Off and on, I’ve been using this facility since July.”
You’ve been in other facilities?
“I’ve been in Houston, Tuscon, Phoenix — those are the three VA facilities I’ve been in. I’ve been in various other civilian hospitals. The SCI unit here, this is probably the best I’ve been in for acute spinal-cord injuries. The only problem I think they have here is not enough money, not enough space, and not enough staff for what they’d like to be able to do. Don’t get me wrong, for what they’re able to do here they do it quickly, efficiently, and the care is outstanding. I was thinking more on the rehabilitation side. For instance, if you would go to a civilian center like Sharp — now I’ve never been there, so I can’t really evaluate the facility — but from what I’ve heard, they have a larger therapy staff over there, and they teach guys how to go over curbs, up and down stairs, how to overcome barriers — surviving techniques. See, they don’t have those facilities here. They don’t have the space, they don’t have the time, they don’t have the money. This place could be so outstanding if — Have you ever been downstairs?”
Sullivan’s hands, like the hands of all the SCI “chairs” in this unit, are dressed in fingerless, leather-palmed black gloves. I follow behind, his adapted hands thrusting in unison against the friction of wheels, across the lobby. He presses a low button, and the steel doors of a freight elevator open. Inside, his voice resonates.
“They got equipment stacked outside — Nautilus machines, all kinds of things, brand new, wrapped in plastic, ’cause there isn’t any room inside to put it.” The steel doors open after an imperceptible stop. We move down a wide hallway past an unfinished addition.
“They run out of money,” John says.
Farther, on the right, I see through glass onto the patio where large plastic-wrapped shapes sit. On the left, doors with narrow windows. I peek like a voyeur into a room secluded from the able-bodied and try to imagine what happens in there. From the walls hang gothic straps in assorted man-sizes and vapid colors. Then, in a cavity to the side, there rises from the floor a bedlike thing of stainless glimmer — a limbed, robotic skeleton. (Silently, I feel shame as the room conjures up images of Milk of Magnesia and — ugly old nurses.)
We move farther down the hall, and I peek again into a much broader room of assorted pieces of exercise equipment. Nearest the window are what look like blue tumbling mats, elevated three feet off the floor, each with the flat dimensions of two king-sized mattresses. “You can do a number of things on those mats,” John says. “You can roll, learn how to sit up, turn over.” He sees in my face what I’m wondering:-self-deprecating joke? “No, really,” he says, then pauses. He squirms, pushes up from his elbows, grunts softly, readjusts, an unconscious routine he does often, like a person who tosses in bed.
“You have to realize,” he continues, “I have no muscles ... How can I put this?” Then he sits back and lifts his arms slowly, pointing his fingers to his armpits. “Like from here, everything down is dead meat. It’s dead. Now you think about that. Think about trying to turn yourself over. I can’t turn over. Oh, I can maybe after 15, 20 minutes of trying. There are techniques where you can roll over. You have no balance whatsoever. The higher your injury, the less the balance you have.
“I mean, it’s pretty hard for an able-bodied person to relate to someone in a chair. I couldn’t when I was on my feet. Never gave it a second thought. We tend to talk among ourselves about these things. I mean, we can relate to those things, where possibly you couldn’t. You’re a ‘spinal cord’; well, people here have more or less the same problems: pressure sores, muscle spasms, things like this. Just like it is between Marines. You’re a band of brothers, no matter if you’re a clerk, a baker, an infantryman, a tank driver, no matter what, you are still a Marine. You’ve had the same training.”
My next question was stupidly “able bodied”: Do you have any long-term goal or aspirations?
“You have to realize that I retired from the military and I’m service-connected, and I’m on Social Security now. I have no desire to go back to work. Right now I want to get healthy. I’ve got a lot of health problems. And that’s my goal right now. People don’t realize what happens till it happens. Being paralyzed is indescribably traumatic, to family, to your friends, you know; your previous friends just don’t know how to approach it. They can’t visualize — most of ’em just go away. When you get out in the community, there’s a lot of prejudice against people in a chair. When the average person sees someone in a chair and an able-bodied person is with them, they tend to talk to the able-bodied person and not to the person in the chair. You find this in restaurants quite a bit, when the waiter or waitress will come up and they will take my order from my wife. I’m not brain dead, you know.”
I can see the effect of “no muscles” on the shape of John’s lower trunk, where, with nothing resilient to hold in the insides, his abdominal wall bulges like a ubiquitous rupture; I notice — and am surprised — that he is not strapped in.
“There’s a reason I’m not. Normally I would be, but because of health reasons I’m not. I’ve got what they call heterotopic ossification of bone. What it is is my body thinks my bones are broken. To understand that, take yourself, say you break a bone, your body manufactures calcium and sends the calcium down to the broken spot to heal the bone. Well, HTO, which is common in quadriplegics and paraplegics, okay — about 50 percent of ’em get it within a 50-month period after injury. My body thinks every bone in my body’s been broken, so it’s trying to make new bone all over my body. Look at my knees.”
I note one appears fairly normal size, the other shrunken.
“Feel this one.” The larger leg is not flesh. It feels like a hardened cast. “That’s all new bone where it shouldn’t be. Now feel my hip.” He adjusts with a grunt. I touch the bulged area near the hip. It is solid and grotesque in size. “Now, push here.” He points to the opposite hip. I touch with hesitancy. “Push.” My fingers sink in as if I were gutting a fish.
“That’s what I’m here for now, waiting to see if they’re going to operate and remove my hips so I can set — ” he adjusts, grunts — “so I can set right.”
Later, I would talk to an orthopedic surgeon who would explain to me, in graphic terms, the procedure: “You just go in there and start sawing. I was involved in one once, and by the time it was over the room smelled like a barbecue pit.” He also explained the seriousness of the result. “A wheelchair patient really needs his legs and hips, for support, even if he can’t use them. The surgery is done with reluctance. The result is that the torso must be placed in a molded bucket in order for the patient to sit.”
One last able-bodied question to John: Did you see Born on the Fourth of July ?
“No, but I’ll tell you what. Kovic, to me, is nothin’ but a wimp. That’s all he is, he’s a wimp. First of all, no one pressured him to join the Marine Corps. And I can tell you, as a 17-, 18-year-old kid, he was probably chompin’ at the bit to get to Vietnam. So now he cries about it. It was everybody’s fault but his.”
They dumped the stuff out of the sky and onto the jungle like it was a great weed patch — and I was one of the ants....
“Mention Agent Orange,” says Dr. Arnold Gass, “and I’m the one who examines you. No one else examines for Agent Orange.” Gass is San Diego-VAMC’s appointed environmental physician. There is one in each of the VA’s 172 medical centers. The responsibilities of EPs are to oversee not just Agent Orange-related issues but also those dealing with people’s exposure to nuclear radiation (atomic bomb testing or actually having been in Hiroshima or Nagasaki). Public awareness, however, is centered on the herbicide.
“What I do explicitly is, if a veteran wants to be assessed for his general health or for a specific problem that he thinks might relate to Agent Orange or is applying for compensation, then he signs up and comes in for a full hour with me, and we do a complete history and physical and laboratory tests, X-rays, and then I give him my personal assessment of his health.”
Dr. Gass appears to be in his late 40s, sports a casual dress shirt with bolo tie (clasp decorated in Southwest Indian motif), and seems absolutely at ease about his job. “What I do is not any hidden secret in any way, shape, or form.” (On the wall behind him hang watercolor portraits, one, a handsome young man, elbows on knees; the other, an evocative image of a thin girl dressed in little more than nylons, hand draped over raised knee, other hand grasping a phallus-shaped object.)
I tell Dr. Gass that every civilian doctor with whom I’ve discussed Agent Orange has conveyed to me his unwavering conviction that the entire AO issue is a bunch of shit.
“They have to be very careful, because we have an aphorism in medicine: ‘Never say never; never say always.’ Okay? So, absolutes can’t hold water in medicine, and that’s true in this case as well. There are people who got sick from having herbicides sprayed on them in Vietnam. The only illness that we know of in man that is definitely linked uniquely to Agent Orange is linked to the dioxin, which is the contaminant in one of the two chemicals that is used to make the compound. And that illness is a skin rash due to the chlorine. Therefore, it’s called chlorine-acne or chloracne. The Germans [in the 1950s] demonstrated that you could cause chloracne by painting increasing concentrations of the dioxin on people’s skin.”
What exactly is chloracne?
“Chloracne is a rash that looks just like bad adolescent acne. It has some unique qualities related to the density of the lesions and where they’re distributed on the body. And it’s known to be caused by exposure to the dioxin part of this contaminant in Agent Orange. But the question is, what about all of the animal experiments in which dioxin has been given to various species of animals and they’ve gotten all of these horrible things that are always listed in the articles?
“The answer to that is that the thing we know about dioxin is it’s very species-specific, that it causes different things in different species. And the only way you can actually answer the question in men is to actually have exposures in men. And those exposures have occurred, either accidentally or deliberately.
“And it’s happened industrially. The most notable accident happened in Italy when a chemical plant exploded one Saturday afternoon. A plume of smoke went right down the valley, and it contained this dioxin. So epidemiologists went in and studied people using mathematical models along the cone of this cloud. In theory, the people closer to the factory should have had more disease. They didn’t discover much of anything — except an increase in skin irritation.”
Having actually been a grunt (sleeping, eating, living) in the jungles along the DMZ of Vietnam when defoliation operations were being conducted heavily, should someone like me ask to be examined?
“I’ll be going against the party line, but I’ll say no. Because, ultimately, when you were done with the screening, I’d probably not say it wasn’t worth your time to come in here, but I would probably say that there’s nothing you really need to worry about.
“But the Marines had nothing to do with Agent Orange directly. It’s possible that some Marine groups were out on patrol or in the field, and a spray plane might have flown over, and they could have accidentally been doused with some of this spray. If they were, the chances are virtually nothing that they would have gotten sick from it, acutely or chronically. So my advice to you, personally, and to people like you, would be that it’s not necessary to come in.
“The biggest thing about Agent Orange that ever happened was that it destroyed the countryside in Vietnam. And the second thing is that it’s hard to know what it might have done to the Vietnamese people who are still there, particularly women of childbearing age. But that kind of information is hard to come by with any kind of the scientific rigor that we demand of our own studies in this country.”
I ask Dr. Gass to comment on the growing anger among veterans and veteran’s organizations who believe that the VA is stonewalling. He at first offers to provide me with copies of “official VA positions.” For a brief while, we discuss a few asides. Then, “As far as stonewalling, you have to understand, and this may sound brutal or standard party line, but it’s the truth. The federal government, through its division of veteran’s benefits, is very willing to compensate anyone who has honest diseases, honest conditions. The law says we must, and — provided you identify yourself to us and we agree with you — we do. The Agent Orange story, though, was very different. It’s one thing to have an eye injury in Vietnam, and, uh — ” (his eyes pause on mine) — “it’s pretty obvious. It’s another thing to say, ‘Well, I was exposed to this substance about which nothing is known, and I’m gonna blame every little thing that’s happened to me, both psychological and physical, on this substance.’
“Now, the VA’s tradition has always been to compensate based on scientific information. So what it did, when it created its regulations to compensate for Agent Orange, it said if a condition is proven, we will pay for it. And if it’s not, we won’t. Well, the Vietnam veterans took them to court, and the VA lost — two years ago in San Francisco. The court said the regulations are too restrictive, based on the law. What we’re going to require you to do is to revise your regulations and to compensate based on statistical associations for likelihood — not iron-clad, absolute scientific proof. The new secretary of the VA didn’t even bother to argue that. One of his first decisions when he got into office was to say, ‘I’m not immune to make that decision; we will comply fully with the law.’
“And so, they’ve been re-writing these regulations. Well, during the period of re-writing, no one’s getting any compensation at all, because they don’t know what they’re going to be regulating. So as soon as this is all done, they’re going to have to look at all 30,000 back-cases, plus all the other cases that have come up. That takes time, there are fewer people around to do it than ever before, but it will eventually get done.^*
"You talking about heavy W/M care?” asks Bob, head tilted.
I reiterate that I’m talking about “vegetables.”
“I’ve been here 19 years,” he then continues, “and in the nursing home program, we’ve only had one which we consider to be comatose, vegetative state, that I can recall. We might have had one other. One visibly stands out who was in long-term care; but actually, we don’t have any who are in the hospital right now.” Suzanne speaks: “There might be a few out there. There’s a gentleman now, for example, who’s on the psychiatric ward.
"He’s a Vietnam veteran, I think. He’s, like, an old head injury from 20 years ago, from shrapnel. He’s somebody who lived at home with his father, and now he’s gotten more agitated and more upset lately, and so he was run into a medical service, then transferred over to psychiatry. And we’re trying to get him out to a brain injury center in the community. Because usually, when people have been brain injured, the rehab period that’s most effective is right after the injury. It’s hard to make a change 20 years after a head injury. But there’s some reason to think that he could benefit from a few months of treatment in a brain injury program in the community. We’re probably going to be sending him out at VA expense.” Suzanne Demong is the VAMC’s chief of social work service. Bob Carney is supervisor/coordinator of community care programs. I had come to Suzanne’s office still curious about the fate of Johnny Got His Gun-types who return from wars decerebrated (or thought to be) and must be littered throughout the country — somewhere.
Bob continues, “Either they die fairly rapidly or they improve and become people like the man we were just talking about. Well, now there’s one nursing home which we have not made placement in for that purpose. It does have quite a few young, total-care [VA] patients. We use it for ‘locked’ and we use it for ‘regular skilled.’ But [the homes] get paid by the state, somewhere in the neighborhood of $250 a day to $300 for this type of patient.” Locked?
“Psychiatric-type. Now, we have some veterans in there that are mostly older, that are demented, although there are few maybe younger.”
“The reason being that,” Suzanne explains, “if you’ve had a severe brain injury, sometimes you tend to wander.”
Bob continues, “We have some young veterans, they’re 100 percent service-connected, like one, a tire blew up and damaged his head. We have another man who’s been in the nursing home about 17 years. He can’t talk, he has no control over his eyelids, things like that. He’s very incapacitated. And there might be a Vietnam veteran among them too. We don’t have a lot of them. Residential care is where you’re likely to find most of them.”
The difference?
“That’s where they’re living in someone else’s home that’s a licensed facility. Anywhere from 6 to maybe 150 who can get through the day but need to make sure they take medication, to prepare meals. It’s kind of a caretaker thing. Those would be veterans who have no family or maybe had some behavior that could not be tolerated in a family situation. Most of those with families are probably living at home.”
This is a large hospital, with a large bed capacity, yet I get the impression that outpatients constitute the greatest proportion of veterans dealt with here.
“I know,” says Bob. “A tremendous outpatient load. And of course, in general, medical care is moving this way. I mean, we’re kind of in the mainstream of how hospitalization or medical care in the country is going. ’Cause, actually, hospitals are paid, even as we are, on turning over, not keeping people. I know, historically, we [were] famous for keeping people.
“We used to offer any veteran coming into this hospital who needed skilled care a six months’ VA contract. That means six months the VA covered care. That’s now down to three months. And even that, even now, if a veteran can go another way, like MediCare, they will go that way.”
Rita C. Monteiro received her Ph.D. in clinical psychology from Wayne State University in Detroit. She wears a gray blazer (padded shoulders) over a floral-print blouse and conducts herself in composed, businesslike fashion. Monteiro is chief of the alcohol-and drug-treatment program, a significant slice of the psychiatric section in the VAMC. (According to Bob Stevens, the center is “pretty evenly divided, between medicine, surgery, and psychiatry,” an interesting aside regarding the demographics of today’s veteran population.)
Walking through the waiting areas of the ADTP is reminiscent of a stroll through a Greyhound bus depot. Most patients appear impoverished. Why?
Monteiro explains, “Because of the eligibility criteria. Basically, people who earn over a certain amount are not eligible to receive services here. It is a problem, because now insurance [companies] are cutting back on substance-abuse treatment. There are a lot of veterans who, while they may have jobs and earn too much money to qualify for [VA] services, don’t have the insurance to pay for their own service. There’s a large population of veterans out there who really don’t have anywhere to go. We’re concerned about that population. As it is now, the person has to wait until they’re almost destitute before they can qualify for service.”
And yet veterans can be rich and still qualify for VA treatment if they have a service-connected disability. “Yes. We do get those occasionally. And that’s good to have a mix of patients too, so that people who are destitute can see people who are doing a little bit better and that gives them more hope.”
How does an eligible veteran get involved?
“They come in for an initial evaluation in the outpatient program. They see internists, a physician who specializes in working with substance abusers, and receive a physical. Then we do outpatient detoxification; we don’t do inpatient detox. They receive a medication to help them, and then we send them home. They return every day during detox to see a physician and go to evaluation group.”
I ask about the danger of heroin addicts going home alone to try to detox themselves.
“Actually, alcohol detox is the most dangerous, along with all the other minor depressants. Depressants, period, are more dangerous than all the other drugs. Heroin detox, the person feels worse than they might with other drugs, but there’s no real danger of them dying. Alcohol detox — we have to be very careful, because they can have seizures or convulsions from the withdrawal. Typically, our physicians use a Librium-taper detox protocol. They give them a decreasing amount of Librium each day. It’s a minor tranquilizer. The medication helps them gradually withdraw, rather than all at once.
“They go to evaluation group, they see two therapists who talk to them every day about what’s going on and try to determine what type of treatment they need. One good thing about having the outpatient detox is it does help to prevent people who are not motivated to really stay drug free from abusing the services, if they just want a bed to sleep in and not really want to stay drug free. You have to be fairly motivated to continue.”
Many repeats?
“The government allows you only two admissions to inpatient treatment; outpatient treatment — as often as you like.”
I ask Dr. Monteiro to explain the inpatient program.
“Once they finish the evaluation group, and [if doctors] decide it’s inpatient treatment that’s indicated, then they actually get admitted to the hospital'. They stay 28 days, and it’s a very intense, active program. That’s why we have them detox first, because when they come in the program they need to be alert and coherent and willing to participate. There are education sections, group-therapy sessions, skill training sessions, all day, every day.
“They learn about alcohol and drug abuse, its effects on you. Psychological and physical effects. We have people from psychology, people from social work, people from the community who come in and speak; we also do some movies. Vocational Rehab does a lecture on vocational resources. In therapy group, they talk more intensely about their own substance problem, every day.
"They have relaxation training sessions; they have a leisure skills utilization group done by rec therapy, telling them how to do things that are fun and enjoyable without getting high. And they have outings. ’Cause typically, these are people who, everything they do is associated with getting high. We have community college instructors. One does a communications course, one does what’s called ‘personal growth,’ but actually, it’s assertiveness training. And one does a sexuality course.”
What percentage of the patients are women?
“Very small. It’s about two and a half percent. We expect that will increase, because now there are many more women in the service. It seems like it’s already starting to increase a little bit. Already this fiscal year we’ve had as many as we had the fiscal year before. But a lot of women don’t even know, for some reason, that they can use the A. I don’t know why, but they say, ‘Oh, we can come there? Oh, I didn’t know I could come here!’ ”
Hell was less a place than a vortex, undulating, thrumming, the eternal disintegration of my being into conscious atoms. Think the shrinks call it “disassociation.” Wouldn’t know, though. Never been to one. Tried once (last year of college) when I used to drive around with a loaded deer rifle in the trunk of my Mustang. Dialed the VA and said, “Got a problem.” They said, “Oh, what?” And I told ’em. They treated me like there was something wrong with me. So I said screw it and never went. Didn’t matter. I figured out later (years later) it all has to do with power — like God’s. Today they call it post-traumatic something or other. But that’s for people who haven’t figured out the power.
Like when my best civilian friend got killed driving my car for something I got him into.
After it happened, I drank for two weeks straight, then jumped a plane for Dallas and the only buddy I know is still alive from my old platoon. (He was with me the night I got wounded; was the only one who’d crawl out in the dark to get my sorry ass.) So I went to Dallas. We took rifles and drove into the desert and shot lizards and horny toads. He was married with two kids. But we both agreed it felt good.
Then, years after that, I’m a respectable person, got a good teaching job, coach football. It’s homecoming. We’re winning, fans are cheering, wind is blowing, and the moon ... the fuckin’ moon ... is as big and round and ugly as a dead man’s mouth. Keith Jewett — two days past 18 years old. I’d recruited him when he was in junior high. Had to do a lot of talking too, ’cause his mother was a nurse, and she was afraid he’d get hurt. “Don’t worry,” I told her. With 7 minutes and 35 seconds to go in the game, he dropped dead. Like any coach worth a damn, I loved the boy. And all I could do was stand and watch this mother give mouth-to-mouth to her son while a doctor slowly shook his head. Next morning I load my rifle. Think about it — but don’t do it. Just hold it and feel better in the knowledge that once upon a time I’d played God and taken human lives without any thought whatsoever and, if ever I want, can do it again. That’s the power.
I think about this sitting in the “nut ward,” waiting to interview some Ph.D. about post-traumatic something or other. Most of the people here look as normal as any other unemployed person (basically, tired and poorly dressed), but there’s a couple looney toons around here. And I think about the smell of this place (that hospital smell) and my vision of hell at the age of ten.
Fifth-grade recess: Me an’ the guys have taken over the swings from the girls, not to swing (hell no!) but to jump. Whoever jumps the farthest has the biggest balls. I’m pretty much the champ at this event (largely because I’m no good at baseball), and I have that swing swooshing as high as the crossbar. The trick, see, is to jump on the way up (so you sail out), but I hesitate — and drop like a B-52. Mrs. Moen thinks I’m laughing (until she sees my hand where my elbow should be). By the time Mr. Bashaw gets me into his station wagon and to the hospital (arm splinted with the halves of a broken yardstick), I am delirious. They give me a shot and wheel me under a lamp big as the sun. They place something on my face and begin dripping ether.
The first few inhalati'ons are like sniffing rubbing alcohol.
Then the droning begins: consciousness alters and darkens, like being drunk while someone bricks you in. Each breath sends a surge of prickles from head to toe, then evolves into slithering buzz (like worms crawling in your mouth) until it becomes you, disemboweled, disembodied, exploding into infinite atoms — orange, black, spinning, buzzing — whirlpooling into a writhing esophagus with no entrance, no escape, unending, a sinuous tube of eternity, consciousness of the damned, satanic chant... TOO late, TOO late, TOO late, TOO late....
"Have you had mental help from the VA?”
What?
“I know it’s a personal question, but — ”
No.
Jeffrey Matloff looks like a young Al Pacino playing the role of a clinical psychologist in a movie called Flashback and Bad Dreams; instead, he really does have a Ph.D., and clinical psychologist is his real job.
“You’ve had some exposure,” he says, “just sitting in the waiting room and seeing the kind of population we get. It varies quite a bit. You have people with drug or alcohol problems coming through here, people with acute psychiatric emergencies, people who are just part of the normal client-mode. What would you like to know?”
About post-traumatic, uh....
“Post-traumatic stress disorder, PTSD.”
I ask him to explain it.
“PTSD developed basically with the recognition of the Vietnam combat veterans, in addition to other groups, who have gone through a horrific experience recognized by all as being outside the realm of normal human experience. For instance, concentration camp survivors from World War II also were a group prone to experience these so-called PTSD kinds of problems. Certainly being interned in a prisoner-of-war camp might be another. It carries several different types of physiological and behavioral responses. Some of the symptoms are nightmares, kinds of intrusive thoughts — flashbacks, if you will — from some of the events. This can happen months, even years after the initial event was experienced. Basically it’s considered ‘shorthand’ — the normal reaction to abnormal events in one’s life.”
Normal?
“Certainly. Painful war memories and dreams, even long after a war, are normal. The big thing you want to look at is how is it impacting this person. I mean, there are guys from World War II, for instance, who may very well have symptoms of PTSD but who cope pretty well. I think if we look cross-culturally, warriors, in whatever culture, many of them probably have symptoms. What we oftentimes see is a kind of numbing, a turning off, withdrawing, not wanting to get involved with people. Sometimes you’ll see an inability to hold jobs, interpersonal relationships will be greatly affected. I think the big difference with what happened in Vietnam, compared with what happened in other conflicts, was the homecoming our warriors received.”
Dr. Matloff openly admits (to his patients and to me) his role during the Vietnam war. “The guys you read about, in the streets, protesting, that’s where I was. And, let’s face it, the homecoming for you guys was really not very good. Basically, society has learned that this is not the way we should treat our warriors, the people who put their asses on the line.”
What happens when a patient brings up something he did that was criminal, like, maybe, he fragged somebody? That ever come up?
“Uh, not frequently.”
Or he accidentally killed a buddy? Or is it, as they say, doctor, just the experience of combat itself, the overpowering magnitude of war and the inability to assimilate the experience into daily life? That it?
“It’s some of that. Oftentimes, though, it gets down to very personal vignettes. Could be things like somebody who talks about not being able to save a buddy and harboring that kind of guilt; listening to their buddies scream and falling asleep with that kind of thing at night, you know — things. Intrusive kinds of things. Or.maybe coming across a civilian who they thought may have been a VC — something like that.”
(I remember once trailing two Vietnamese males, early 20s, smokers, waist-long hair, sneering and muttering in gook, around a Safeway store, me whispering to ’em bu'koo DOW! bu'koo DOW! and hoping they’d shit their pants — something like that.)
“Or maybe having to shoot somebody who was, yes, ‘unfriendly,’ but conceivably, you know ... you remember from your training you weren’t trained necessarily to shoot women and children and things like that.”
(Not necessarily, correct.)
“The thing to remember is that the dreams and the flashbacks, to some extent, are normal. It’s when they start impacting one’s life in terms of, you know, causing problems in relationships. One of the things we see in Vietnam veterans is that many of them have relationships that are strained or nonexistent. Where they’ve had multiple relationships, generally very shortlived. That’s typically one of the problems for folks that start experiencing problems with PTSD.”
Why does it happen? Is it the inability to communicate about something impossible to communicate?
“Yeah, there’s certainly that. And the whole thing about getting close to somebody and then losing them. Abandonment. You’ve gotten close to people in the past who are no longer around. And, you know, those kinds of feelings of loss tend to keep somebody pulled back in. Plus, ‘Who could ever understand the kinds of experiences I’ve been through,’ and ‘If I start to tell people, I’ll blow them away with the kinds of experiences I’ve had.’ ”
So how does somebody end up in your office?
“Generally by the time somebody sees us, we’re pretty clear that they have been exposed to combat, because that’s fairly easy to detect from their discharge, their DD214. As for how physically they get here, sometimes they come in by themselves. Oftentimes they’re dragged in by a spouse, if they’re married, or a girlfriend or a family member who might say, ‘This person’s not communicating’ or ‘He lost another job,’ things like this. Then again, maybe they got referred from some other department. They may have another problem but not admit, if you will, to having this particular problem.”
Do you have a “typical” patient?
“I can’t really talk about specific patients, but generally, what I see with a lot of folks, the folks who may actually have PTSD, is there’s a reluctance to admit to having it.”
Comments