 Facebook
Facebook
 X
X
 Instagram
Instagram
 TikTok
TikTok
 Youtube
Youtube

"What makes this court unique is that were dealing with people who haven't committed crimes, they're ill, ” said Paul Parris, acting that day as bailiff for mental health court, held in Department 14 in the downtown county courthouse. “When these people run, we call them ‘elopers,’ not ‘escapees.’ With an eloper, when I call for assistance, I will say, ‘Don’t come in with guns drawn. If they run, you don’t tackle them and crank on them like you would an escaping felon. These are sick people, citizens.’ ”
Outside Department 14 is not the ordinary courthouse crowd. Certainly some clothing selections are peculiar — a blue-and-red Madras plaid shirt, for instance, worn with green and gold and tan plaid trousers, and a woman in her late 30s with a bulky muumuu falling down over her body, and a big girlish bow stuck incongruously at one side of her head, and thin lips over which lipstick is smeared as if a child had colored in a coloring book and gone over the lines. Gestures are odd — exaggerated, even operatic in some cases, and in others, jerky and repetitive. Eyes wander, then fix on empty space as if the eyes see something or someone. Many talk to themselves. And perhaps as many hunker silently, as if in the grip of terrible lethargy.
Seated on one of the wooden benches that line the hall, under windows that look out onto the jail, a pretty young woman wearing a sleeveless blouse lifts her right arm, carefully sniffs her armpit, then lifts her left arm, sniffs that armpit, frowns. She repeats this sniffing, first one armpit, then the other. She breathes in her odor so deeply that the sound of her breathing in is audible. A man with a laminated photo ID clipped to his shirt stands near her, at the bench’s end. She stops sniffing, presses her arms tightly against her sides, and with eyes suddenly wide open, as if in fright or shock, she asks the ID-clipped man if she may use the bathroom. He says yes, and when she rises to her sandaled feet and in a shuffling, irregular gait walks toward the women’s room, the man is right behind her.
Nearby, on another bench, a plump redheaded male wriggles restlessly. He mumbles into his lap, scratches at his trousered legs, grins into the vacant middle distance. His fingernails are chewed to the quick, and the cuticle on each of his fingers is lined with a thin margin of dried blood. Up close he has a sickish, lone, and breakable look. He seems to speak to someone standing before him on the hallway’s brown tiles. No one, of course, is there. After a moment’s fierce staring and a quiet babble that is a cataract of vowels — ooooh and aaaah and oh — he turns, asks querulously of the woman next to him, “Can I have a cigarette now?” She says no, he can’t, he will have to wait until after he talks to the judge. He asks again. She says no. He returns to his intense gaze at emptiness and to his ooohs and aaaahs and ohs.
The young woman, someone tells me, is schizophrenic, with a symptomatology that ranges from command auditory hallucinations to covert feces-eating. The man following behind her is a psych tech from the hospital in whose closed, locked ward the woman has been kept, against her will, for the past three weeks. The redheaded male is manic-depressive; he lives in a locked facility. He and the armpitsniffing young woman, heading back now from the bathroom to her bench, have been brought here, I'm told, for conservatorship hearings.
Tuesday and Thursday mornings, Department 14 is reserved for conservatorship hearings. In 1968, California’s Lanterman-Petris-Short Act (called the LPS by lawyers and mental health professionals) changed the law under which mentally ill persons could be committed to institutions. Before 1968, a document submitted to Superior Court by a psychiatrist, indicating that a person was mentally ill and required hospitalization in a state or private mental hospital, could be enough to put that person away for life.
Mental hospitals were warehouses for the mentally ill, many of whom never left. And once in the hospital, the mentally ill had few legal rights.
LPS tightened standards for committal, set limits on how long a person can be held without court hearings, required that treatment take place in the least restrictive setting closest to the person’s home, and increased in scope and number legal rights left to persons diagnosed as impaired by mental disorder or chronic alcoholism.
LPS conservatorship replaces pre-1968 civil committal. In simplest terms, it gives decisions regarding a person’s care to someone other than that person. Approximately 2200 people in San Diego County are LPS conservatees. Of that number, some 100 are in state hospital beds.
The rest live in the county, either independently or in board-and-care facilities or in one of 22 local hospitals that provide treatment for mental disorders.
A person will not be placed under a conservator’s care simply because he is diagnosed as suffering mental disorder or chronic alcoholism. The Superior Court must also find such a person so gravely disabled as to be unable to provide for his food, clothing, and shelter. And the court must find that no one else is able and willing to meet those needs£ As one psychiatrist explained it, “You can be as nutty as a fruitcake, but if you can provide food, clothing, and shelter for yourself, you don’t have to accept treatment for your disorder, and you can come and go as you please.”
Inside Department 14, the spectator section is divided into three rows, each with a dozen seats. This morning, perhaps half these seats are taken. I count half a dozen persons who are subjects of these hearings, including the pretty young woman, seated now in the first row; she continues, although more furtively, sniffing her armpits. Also present are psych techs, assigned to watch those who are here from hospitals, and county transport aides who’ve driven people to court from board-and-care facilities. Psychiatrists are here to testify as to why a person resident in their hospital should be placed on or kept under conservatorship. A psychologist and a psychiatrist are here from County Mental Health’s forensic unit to testify as to the condition of persons already on conservatorship who wish it to be ended or its conditions amended.
Behind the bar sits County Counsel Janice Ingold. County counsel represents the Superior Court’s Counselor in Mental Health, the agency that initiates LPS conservatorships, and the Department of Social and Health Services’ conservators’ unit, whose social workers act as public conservators for the gravely disabled. (Of the approximately 2200 people currently living under LPS conservatorships established in San Diego County, some 500 have private conservators. The other 1700 have public conservators.)
At what would be the defense table in a criminal trial sit members of the office of public defenders’ five-member mental health team. Then there are court clerks, a court reporter, a bailiff.
Superior Court Judge Laura Palmer Hammes addresses those present for conservatorship hearings. She begins by reviewing procedure. “I will listen to the doctor’s testimony, I will read reports in your case, I will listen to what you have to say and to any witnesses brought on your behalf. Then I will make a determination as to whether, by reason of mental disorder, you need a conservator to assist you with the daily function of life, that is, food, clothing, and shelter.”
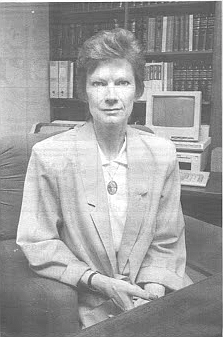
A tall, slender redhead with a china doll complexion and delicately modeled features, Judge Hammes was a deputy district attorney in San Diego County from 1972 to 1984. She was appointed to the Municipal Court bench in 1985, to the Superior Court in 1986, and to mental health court in January of 1991. A judge will generally serve one year in this venue.
Judge Hammes leans forward on the bench, speaks conversationally. “If I determine that is the case, then I would appoint a conservator to assist you. The conservator could either be the public conservator or a private conservator — that is, a friend or family member who would assist you with these functions.
“Then I would decide least restrictive placement for your living — that is, the type of living arrangement, not the specific place where you live. That is determined between you and your conservator. That could be anywhere from independent living (that is, living out on your own) all the way up to a closed, locked treatment facility or a state hospital level.
“I then must determine what rights may have to be restricted in your case — that is, whether or not you should have the right to possess a firearm, to vote, to contract, to make medical decisions that are related or unrelated to your mental disorder.
“You have certain important rights with respect to this morning’s hearing. You have the right to contest conservatorship, to say, ‘I don’t think I need this,’ and tell the court why. You have the right to the assistance of an attorney. If you cannot afford an attorney, then the public defender, who is very skilled in this area, will assist you. If you can afford an attorney and wish to bring in your own private attorney, you may do that as well. You also have the right to a jury trial. After this hearing is over, you may request a jury trial in this matter.
“It’s important to know that if the conservatorship is established, it will last for only one year and that it must terminate after that one year, unless it is reestablished by another court hearing.”
Wang’s case is called first.
(Although conservatorship hearings are open to the public and a matter of public record, all names of conservatees or potential conservatees have been changed, as have some details such as physical traits, to disguise identity.)
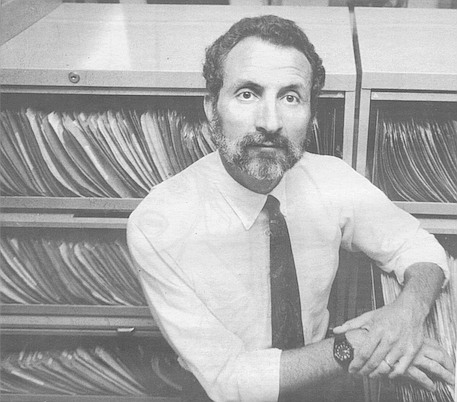
Gregg A. Michel, Ph.D., a member of County Mental Health’s forensic unit and a psychologist in private practice, is called to the stand to testify in behalf of the county.
Mr. Wang — stooped and somewhat wan, wearing dark trousers, white polo shirt, and beige cardigan — has waited outside in the hall. He is brought in by the bailiff and directed to the defense table, where he’s greeted by his attorney, Steve Binder, a member of the public defender’s mental health team. In front of Binder on the table are stacked pale blue case files in which clients’ records are kept.
Binder several weeks earlier visited the board-and-care in which Mr. Wang lives and talked with him about his reestablishment hearing. Mr. Wang had asked that Binder get him removed from conservatorship.
Like all judicial proceedings, these hearings follow a course. Testimony drawn out by county counsel, asking either for conservatorship or re-establishment of conservatorship currently in force, is designed to elucidate the person’s status as gravely disabled. The defender has the burden of proof. It is his job to show the person not gravely disabled.
County counsel opens by questioning the psychologist or psychiatrist who has evaluated the conservatee.
Seated in the witness box, Gregg Michel (pronounced “Mitchell”), a dark-haired, clean-shaven man in his 40s, is sworn in by the clerk.
County counsel begins, “Doctor, have you had an opportunity to examine Mr. Wang?”
Michel answers in clear, strong tones. “Yes, I did. I saw him here in the courthouse in the forensic evaluation unit....”
“Have you formed a diagnosis as to his mental condition?”
“Yes, his current diagnosis consists of what is called schizophrenic disorder. In the past, he’s been diagnosed as suffering from schizophrenia and later with ‘bipolar’ — what used to be called manic-depressive illness. His current treating physician feels that schizophrenic disorder is the most appropriate diagnosis, and I concurred with that assessment.”
“As a result of this mental disorder, is it your opinion that he’s unable to provide for his own food or clothing or shelter without assistance?”
“Yes, it is.”
“What about Mr. Wang’s functioning led you to believe that he is unable to provide for his basic needs?”
“The essential situation with this patient is that he tends to decompensate and require acute hospitalizations. When given appropriate medications, he then responds well and stabilizes. There has been a repeated cycle of this occurring.
“The current problems really have to do with his needing more insight into his own needs for treatment.... He evidenced some symptomatology that was relatively passive — illogical and psychotic thinking, difficulty in sequencing thoughts, some relatively mild depression.”
Mr. Wang, says Michel, is “ambivalent about taking medications and hopeful he may not need them in the future.” Further, says Michel, “He indicated that sometime in 1990 he had gone off medication because he didn’t like his previous board-and-care. He didn’t see judgment problems inherent in that.”
Michel notes that Mr. Wang is 38 years old, that he was first diagnosed at 19 as having a mental illness, that he has lived in a series of board-and-care facilities, and that in the past four years he has been hospitalized several times in an acute-care facility. Mr. Wang’s ceasing to take medication and subsequent decompensation was a pattern that, according to Michel, is not uncommon. “Patients stabilize and do relatively well and then begin thinking that they can do without medications. When they try to go off them, then you see the cycle continue.”
Then begins the litany of questions always asked by county counsel. “Is he capable of operating a motor vehicle?” “Of entering into a contract?” “Making medical decisions unrelated to his mental disorder?” “Completing of a voter registration form?” “Might he be a danger to others in possession of a firearm?”
Michel considers Mr. Wang capable only of making medical decisions unrelated to his mental disorder and filling out a voter registration form. Michel believes Mr. Wang would be a danger to others were he in possession of a firearm “because he does have a history of acting out, of being impulsive. That is a continuing problem, according to board-and-care staff.”
County counsel asks Michel, “In your opinion, at this time what is the least restrictive level of placement for him?”
“At present, my opinion is that a board-and-care facility is appropriate, because he still requires prompting to eat, to take medications, to go to treatment. I think, though, that the goal for him in the very near future should be independent living.” Public defender Binder begins questioning Michel. “You noted that he ceased medications in 1990 in order to get out of the board-and-care in which he was living?”
“Well, he said his reasons for ceasing medications there were because he didn’t like the board-and-care.”
“He did specifically state that it was dirty and he didn’t like being there?”
“Yes.”
“Have you been to that particular board-and-care?”
County counsel objects. Judge Hammes overrules the objection, directs Michel to answer. “No,” Michel states, “I haven’t.”
Binder queries Michel about Mr. Wang’s recent compliance with taking medication and attending day treatment. Michel notes that Mr. Wang has, with prompting, taken medication, attended treatment.
After more questions from Binder to Michel, questions intended to permit Mr. Wang to establish his ability to live without conservator’s supervision, Mr. Wang is sworn. Binder asks his client,
“You understand the doctor’s concern that off conservatorship you may cease to take your medications?”
“I would like to explain to the judge that this has occurred in the past, but my mind has stabilized to a point where I am more coherent within myself and in my surroundings. So I am willing to take medication at all costs.”
Judge Hammes asks, “What are the costs?”
“I don’t know the costs, but at all costs. I mean, it’s really destroying your life if you are not taking medication if needed.”
Judge Hammes asks, “What do the medications do for you?”
“I am not sure. I know my thinking is not as clear as it used to be, Your Honor. And it seems like maybe the doctor right now has doses a little bit high, but I will continue taking my medication, because life is very precious and, you know, I don’t have 35 years left on this earth. I want to get a job. I want to work. I have two years of college. There is a lot of free time when you are on disability and it’s no fun. I would rather be industrious and do what I have to do and contribute to life.”
“What happens,” the judge asks, “if you cease your medications?”
“Well, at present, I think it would be unfeasible. I think I have a good relationship with the doctor. I think he knows me better than myself at times. He’s a good doctor. I want to stick to him. But I don’t have enough time to talk to him. He’s a real fast-acting doctor. I tell him I want to tell him something, but everybody crowds around and starts talking and I can’t get through the right amount.” Mr. Wang goes on to say that he would like to request a new social worker “because this one doesn’t help me out, doesn’t even talk to me sometimes.”
Binder asks Mr. Wang, “Why did you cease taking medications?”
“Because I was scared. It’s bad — the neighborhood isn’t as good as it was — and it’s like a dungeon where I slept. The lady is okay, but the environment is dark all the time, and it scared me, you know.”
County counsel questions Mr. Wang, “Do you have many friends at the board-and-care or in your day treatment?”
“No,” Mr. Wang answers, expression hangdog. “That is the problem, how I couldn’t resolve the schizophrenia because I don’t want to fool around with those people. I mean, you know, it’s a bad influence. That is why I ran away from the other board-and-care, because it’s a bad influence. I am not comfortable. I run to the doctor. But they should have the board-and-care where I am now checked out because there is no hot water there, and I am scared, Your Honor.” County counsel has no further questions. The judge speaks, notes that based on Michel’s testimony, observing Mr. Wang, and reading the report, she believes conservatorship should be re-established. She adds that she thinks Mr. Wang has “legitimate concerns about medication,” that “without any question, there needs to be more dialogue about medication between Mr. Wang and his treating physician.”
Judge Hammes looks directly at Mr. Wang, whose mouth has turned petulant. “I understand what you are saying. I understand that you are saying, ‘I don’t like the side effects of these medications.’ At the same time, the history says that when you are taking medications, you don’t engage in behaviors that end up getting you picked up by police and brought back to the hospital. I think you know that too, so it’s a matter of getting it worked out. You have to live with some unpleasant side effects in order to stop those bad behaviors.
And apparently Dr. Michel thinks that you are very close to getting it worked out, and he thinks in a few more months of getting stabilized, you should be okay for independent living. So I think there is good hope for you.” Judge Hammes wishes Mr. Wang luck and turns then to county counsel, suggesting a note be made in Mr. Wang’s file that he would like to have further talk with the social worker.
This morning, some 20 uncontested I nonappearances are on calendar.
Judge Hammes wishes, before she proceeds with other cases, to run quickly through these. Jeff Elias, the tall, rangy, fast-talking attorney who heads the county’s public defender’s mental health law team, begins. “I saw Mr. Jones at Edgemoor. He was able to respond. Unfortunately, he rambled. He actually refused to discuss why I was there or what was being proposed. I am sure that he heard me. Either he was unwilling or unable to cooperate. When I asked if he wanted to attend court and contest or be involved in the procedure, he became very agitated and told me to leave.”
Judge Hammes glances up from papers spread open before her, asks, “You do not believe it would be in his interest to be in court?”
“No, Your Honor. He’s blind. He’s not ambulatory, very thin and frail, and I think he can become very agitated.”
Other uncontested nonappearance stories are similar. One person is “of limited intelligence” with “limited understanding” of her situation. Another “did not have capacity to understand what was being proposed and did not participate in the conversation.” Another made only “mumbling sounds.” A patient resident at Metropolitan State Hospital indicated he was happy to stay in conservatorship and “very much did not want to come to court.”
Uncontested non-appearances checked. Miss Preston, a tall, thin black woman, straightened hair pulled back into a stubby ponytail, comes to sit next to Public Defender Susan Daley.
The psychiatrist at Alpine, where Miss Preston is a patient, takes the stand. His diagnosis: paranoid schizophrenia. The story, as it emerges, is that Miss Preston, 35, some six weeks ago presented herself at Alvarado Parkway Institute’s emergency room. She was, says the psychiatrist, “conversing with astronauts” and “felt that astronauts were in her head and gnawing away at her stomach, that she had worms in her and that there were snot rags lying all around the place.” She was emaciated, “simply not eating and taking any liquid at all. She felt food was poisoned and beverages were poisoned.” Although Miss Preston claimed she had been staying in a hotel room, hospital staff insisted she was homeless.
Because Miss Preston wishes to be returned to her family in Arkansas, Alpine staff has attempted to locate her relatives there. Says the psychiatrist, “Those people who know her refused to take her in.”
While Miss Preston mutters, “No, no,” he goes on. He believes Miss Preston has no insight into her condition, and, were she discharged, she would refuse medication. However, shortly after her admission to Alpine, she did begin eating — or as the psychiatrist described, “She became compliant with food and fluid intake very rapidly.” And “she has been participating in the program at Alpine with good attendance.”
Daley leads her client through questions designed to show lack of grave disability. Asked where she is residing. Miss Preston says, “I was staying back in Arkansas. First I chose California because of surgery that I have, and I have been trying to find someone to help me with my surgery that I have so I can get my job.”
Asked how she would get to Arkansas, Miss Preston says, “On the Greyhound bus.” And how much, she’s asked, would it cost to ride the bus home to Arkansas? “A hundred eighty-one dollars. Special is $68.” Daley asks about the astronauts. “Did the astronauts ever tell you to do anything wrong or bad?”
“No. They are not bad astronauts.”
“They are good astronauts?”
“Yes.”
Daley argues against establishment of conservatorship. Miss Preston was not homeless — “has, in fact, never been on the street, she stayed in a hotel and with friends.” Miss Preston’s weight has stabilized, she now denies feeling food is poisoned, she recognizes she must take her medication.
Although Daley pleads her client’s case passionately, it seems clear that Miss Preston will not be released. And indeed she’s not. “Delusion in and of itself would not be dispositive of the court’s decision,” says Judge Hammes, “but the fact is that when she came into the hospital she was emaciated. While she’s on medication she seems to be doing all right....
“My problem is, I feel that I would be turning out a child without assistance if I were to say she’s okay to go out on her own. We feel she does need service of a public conservator. All disabilities imposed except the right to vote. A closed, locked facility is the least restrictive facility.”
Miss Preston, tears running down her cheeks, bolts out the courtroom door.
Before the door closes, she looks across the courtroom and up toward the bench, mutters, “I feel tricked.” The psych tech who brought her to court is right behind her.
Mr. Guston — late 20s, longish I blond hair, blond mustache, wrinkled cotton sports shirt, jeans — walks stiffly to the defense table, sits next to public defender Barbara Gerrard. She explains that Mr. Guston will not be contesting conservatorship reestablishment but that he does wish to request a change of placement.
County counsel introduces the medical declaration for re-establishment of conservatorship, which indicates that Mr. Guston suffers from schizophrenia, paranoid type. A closed, locked treatment facility is the least restrictive placement recommended. Counsel calls Dr. Bernard F. Hansen, the only full-time staff psychiatrist at the County Mental Health forensic unit, to testify.
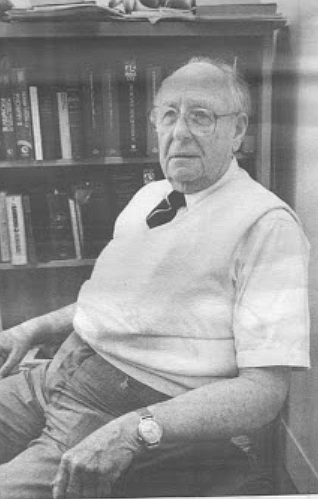
Dr. Hansen — mid-60s, garbed in tie, sweater vest, tweed jacket, slacks — had earlier interviewed Mr. Guston and declares that he suffers “from a schizophrenia of a paranoid type, chronic in nature,” that he remains gravely disabled, that he should continue in a locked, closed facility.
Dr. Hansen lifts his eyebrows, adds, “Which of course he objects to very much.”
From the defense table, Mr. Guston leans forward, pins Dr. Hansen in a fierce gaze. Mr. Guston’s jaw rapidly twitches, and his hands are fists.
Dr. Hansen continues, “I questioned him about statements in the memoranda [prepared for the forensics unit by the conservator], and he claims that he is not angry, not violent. He claims that staff ‘shanked him in the ass’ and set up some sort of electrical shock thing to use on him.
“He claims his doctor is, I think,” Dr. Hansen pauses, studies an open file folder, “a torturer and a sadist because he changed him from Haldol to Thorazine. As well, he accused staff of using cocaine at the hospital. He said they were using ether-based cocaine, and he claimed that he could smell the ether.
“In his examination of mental status, he did not perform at all well. Certainly he has no insight. He feels at the age of 20 he may have been mentally ill, but not now. Testing for retention, he can retain and recall properly only three digits forward and three back, and his memory is impaired. His abstract thinking is way off. He’s disoriented. I asked the date. He said he couldn’t give it, and I said, ‘Well, start with the year. That makes it a little easier.’ He knew it was 1991. He was not able to tell me which month this is.” Dr. Hansen again studies his folder. “And he does believe in telekinesis — that is, he thinks he can pick up paranoid ideas from others, and he tries to talk to them about these ideas and they walk the other way.
“He denies any delusions and hallucinations. [At the facility where he’s resident], I think the major problem has been behavior.... He’s a very angry person.”
Indeed, jaw twitching, eyes narrowed, Mr. Guston appears angry. The bailiff, from his desk some five feet away, keeps his gaze turned steadily toward him.
County counsel asks if Dr. Hansen had looked at Mr. Guston’s placement history in less restrictive facilities, such as board-and-care homes. Hansen has. These placements were not successful. He has been at his present facility for one year, but in the two previous years, he had been in nine different placements, spending 20 percent of that time in hospitals in acute settings.
Guston’s defender, Barbara Gerrard, questions Dr. Hansen. What evidence, she asks, did Dr. Hansen have of attacks on others that her client has made? Hansen admits he has no evidence. She then asks what problems Hansen would foresee were her client placed in an unlocked facility.
“I would certainly feel that what they described as outbursts in the reports and descriptions of being agitated and impulsive, I think these would be a problem.”
“What does ‘outbursts’ mean?”
“Outbursts? I guess, anger. They say that he should remain in a locked, closed facility until his outbursts diminish to a safe level. He is very angry, and I felt uncomfortable talking to him, although he did not express any anger at me”
Gerrard continues. She asks if Dr. Hansen has any evidence of his having been aggressively hostile to hospital staff.
He responds, “All I can say is what they said. ‘Aggressive outbursts, labile in mood, agitated.’ ”
Gerrard pushes. “I guess aggressive outbursts is a bit vague, and I wonder what he might do, what you have any evidence of his having done.”
Dr. Hansen, seeming peeved, answers, “I would say that this would probably put staff and other patients under considerable pressure, at least.”
Gerrard lets it drop. Her client is sworn. Gerrard addresses his desire for a new placement. He wishes to be put in an unlocked facility in San Bernardino.
Gerrard asks, “Why do you not want to live in San Diego?”
“It’s too closed in. I do not appreciate the city anymore. I need the countryside. That is why I asked to move up north.”
County counsel questions Mr. Guston, who admits that his conservator had offered him a placement in an El Cajon board-and-care facility, but he turned that down. “I do not wish to live in San Diego anymore. I have had nothing but trouble from the people. The city is not my lifestyle.”
County counsel asks, “When you have been in board-and-care settings in the past, the doctor’s information was that you were unable to get along and were asked to leave. Do you recall...”
Mr. Guston’s tone takes on ferocity, “Well, in one board-and-care I was thrown on the ground and almost broke my collarbone by a 210-pound black man, not to tell you he was black but that he weighed 210 pounds. He ran the board-and-care. He threatened that he would hit me, and I pulled my arm away from him because he had ahold of me. He slammed my arm in the dresser. I got stabbed in the chin in another board-and-care where I was attacked by a man who was sent to CMH and returned to the same board-and-care, and I was kicked out. He drew blood from my finger, slammed it in the chair and cut it open, and I had to have stitches.”
“Do you think that in any of these circumstances that your behaviors were part of the problem?”
“No,” says Mr. Guston, “l am very low-keyed. ’ ’
“Do you know you have been described as having angry outbursts?”
Belligerent now, he answers, “I tell the truth, nothing but the truth, so help me God.”
“What kind of truth-telling is it that people would describe as an angry outburst? What kind of situation?”
“I don’t lie for no reason, for no one.” “Can you tell us what kind of situation occurred that you felt you had to be honest about that got you in trouble?”
“I had an upset stomach. I was sick, and I asked for a 7-Up, and I was denied a 7-Up, and I told her that she was taking my privileges as an American away from me as well as my civil rights, and she told me I could not go to the canteen furthermore, so I cursed at her, and she took my walk pass away, my other civil right. Now I don’t have a walk pass that everyone else does have....”
“So you did better for a while, then you had these setbacks?”
“No, I have done well all the way.”
Mr. Guston goes on to say that he participates in his group, that he showers and shaves daily.
After more questions from county counsel. Judge Hammes rules. “Based upon the evidence that I have heard, I believe the present closed, locked facility is the most appropriate.”
The judge pauses, gazing down at Mr. Guston, studying him. “As I can see, you are very angry, and it was evident even when you were getting sworn in by the clerk.”
Mr. Guston leans forward, jaw working faster, “You look with your eyes. It’s not with your spirit.”
Frown lines crease Judge Hammes’s forehead. She says, “Well, you looked very, very angry at the clerk, even when she was swearing you in, and I think you might scare people...”
Mr Guston’s mouth is tightly set, his jaw works furiously. When he speaks, he seems ready to spit. “The truth,” he says, standing up from his chair, ‘ ‘is very scary, I must admit, as one telling the truth.”
The bailiff rises, moves toward Mr. Guston, says, “That will be all, sir.
You can go.” Mr. Guston turns his eyes to the bailiff, seems ready to strike him, then pivots, strides out the courtroom door.
This morning, the matter of Dario Gonzalez, a rangy 15-year-old in red T-shirt and jeans, is also heard. Dario was named a ward of the court at the age of four. He has been in the mental health system since he was nine because of uncontrollable violent behavior. For the past two years, he has lived in the state mental hospital at Cabrillo, in a unit set aside for minors. He has asked to be returned to his home in San Diego, to live with his father, brother, and sister. He pleads with particular urgency to be allowed to leave the hospital and to go home. He notes that on his visits home there has been no trouble, he has done as he’s been told, has created no disturbances. Judge Hammes listens carefully, then asks that his case be carried over to give her time to talk with Dario’s family and doctors.
The young woman — Miss Anders — who had sniffed at her armpits continued to do so until she went to sit next to the public defender assigned her case. Questioning reveals that she has recently made another in a series of suicide attempts, that this was not her first hospitalization. Twenty-eight now, she has never held a job and, except for periods of hospitalization, has lived with her parents. Although anti-psychotic medications relieve her more severe symptoms and quiet the voices she hears, she remains depressed and anxious. She often “cheeks her meds” to avoid taking them, and when she goes off medication, she “cuts herself to the bone” on arms and legs. She wishes to be returned to her parents’ home, but they refuse to take her back; they want her placed under conservatorship and to remain hospitalized.
Called to testify. Miss Anders speaks in a tiny, clear voice. She promises, if returned home, she will take her medication, she will see her doctor. After further questioning, during which Miss Anders begins to ramble, Judge Hammes rules that she be placed in conservatorship, with a closed, locked facility as the least restrictive setting.
And there is the woman in her late 30s who wears the bulky muumuu and girlish bow — Miss Tarrington. She sits next to her defender, she hunches her shoulders, huddles in on herself as against some internal chill. County counsel asks the psychiatrist from the hospital in which the woman is resident, “Is it correct that at the time of her admittance there was some concern about her wandering in traffic and that she was saying she was on a journey?” “Yes,” he answers, his voice as matter-of-fact as if he were discussing an oil change for his car. “Originally when she came in, she was markedly disheveled, wandering the streets. When the police picked her up, she said she was Jesus going to Jerusalem.” Miss Tarrington is placed under conservatorship, with level of placement a closed, locked facility. “Good luck to you, Miss Tarrington,” the judge says.
It is almost noon. The spectator seats are empty. Judge Hammes turns to county counsel, asks, “Is that it?”
County counsel nods, says, “That does it.”
Jeff Elias stands from the defense table, begins gathering up the pale blue case files, smiles, says, “That’s a wrap.”
I went to see Jeff Elias, the public defender’s mental health team leader, at his llth-floor office in the City Centre building. His desk was stacked with the pale blue files that held patients’ records, with legal books. DSM-III-R, the Diagnostic and Statistical Manual of Mental Disorders, lay on one corner of his desk, and on the top shelf of a bookcase was a photograph of Elias’s son and daughter. It was early afternoon, and warm. Elias had tossed his jacket on a chair, loosened his tie.
He said he had come to this office three years ago, after serving as a public defender in L.A. for 11 years. “It’s something you have to like. Nobody does this kind of law unless they want to do it. It’s very specialized. It requires a strong advocate but a person who can be compassionate yet not so sensitive as to be crushed by what you hear day in and day out.
“Most of our clients are appreciative, as opposed to many criminal clients. We get cards and calls. Many of our clients need friends, and very often we are the only people they come into contact with who aren’t giving them a hard time. So you find yourself spending time with clients who just want to talk and talk.
“What makes it easier is we are not the treating doctors, not social workers, we are not there to try to dislodge a delusion, we are there to be an advocate for their legal rights, to counsel them to the extent they are willing to be counseled.”
I noted that many of his group’s clients will at first sound rational and then begin to speak near-gibberish. He agreed. “You will hear a person talk for a few minutes and they’ll sound fine, but as they talk longer, you will discover they are delusional, their thinking is not orderly.
“Usually, people who first enter into the hospital exhibit more acute symptoms than what you see once they are ready for a conservatorship hearing. If you went onto an emergency unit, you would see things you won’t see in court. Most people you see in court have been medicated.”
The medication, Elias said, often causes stiffness, shaking, dry mouth, restlessness.
“Many people will have trouble talking because of the medications. They know what they want to say, but they can’t say it. You have to get judges accustomed to these side effects of medication.”
I had heard that at the moment there were three conservatees with jury trials on calendar. Were there many jury trials? “No. We don’t get many. In part, most people don’t seem to be litigious enough to follow through or to fight what’s happening. Some can’t and others are intimidated by the system even though it is fairly informal. We try to comfort people, assure them there’s nothing to be fearftil of. But it’s embarrassing for many people. Imagine, coming to court and having people testify as to all these bizarre things about you. Most clients really don’t put up the fight to which they’re legally entitled.”
I’d seen psychiatrists and psychologists become testy under questioning by Elias’s team. One psychiatrist had told me that he felt Elias got some people off conservatorship who should have remained.
Responded Elias, “A lot of times doctors will accuse us of rabble-rousing among the patients, persuading them to fight and contest. But that’s far from what we do. There is some resistance on the part of many of the medical profession against our giving legal advice. They view LPS as interfering with their treatment. They resent having to justify this, to document that. There are some doctors who are even hostile to us.”
Because conservatorships must be reestablished annually, Elias and his staff see everyone on conservatorship at least once each year. Elias added, “Many of them we see more often than that. Many of them you receive calls from weekly, sometimes almost daily.” He went on to explain that he and his team spent afternoons visiting clients in local hospitals and in the board-and-care facilities. I asked about the latter facilities.
“There are hundreds of these. These are homes, licensed perhaps to house six people. Some are geared to geriatric patients, others to a younger clientele. The people are provided food, medications are dispensed. Staff isn’t necessarily trained to provide medical or psychiatric assistance, but staff members are there to notice if people are taking medications or if they are beginning to deteriorate in their conduct. If that happens, they can contact a conservator or doctor or they can take a person to a hospital.
“You will have people in board-and-care who go to day treatment programs. It fills their day. These programs, ideally, are providing lessons of insight, how to deal with mental illness, understand medication, develop living skills that can be applied to independent living. But the complaint we hear from our clients is that many of these programs are just busy work. Some people are happy with that and some aren’t.
“But it is a hard existence. There is not much to do around the board-and-care during the day. Some want you out after breakfast and not back before dinnertime. You don’t have much money. Most of the money you receive goes toward rent. If you smoke, what extra money you have to do anything is extremely limited. Most people get around $700; most board-and-care facilities get $500 or a little more. There’s no money to waste. It’s a real tight budget. A great deal of monotony is associated with that.”
Had Elias ever seen a case in which he believed a person who was not severely mentally ill was railroaded?
“No. I cannot even think of one case where we thought that or observed that. There are enough checks and balances in the system to keep that from happening.
“There are sick people who are cut loose much more readily in the system than are probably kept. You can honestly and accurately say that there are few people now who have been scooped up by the system who probably don’t deserve to be. Certain ones beat the system, get off conservatorships, and we never hear from them again. But many more come back into the system.”
The hope, he said, with LPS conservatorships was that the mentally ill would be taken from mental hospitals and brought back to the community and put into a setting where they could live a more normal life. “What happened was, yes, the liberties .and protections did, in fact, occur. The unfortunate thing is the community programs that were to be put in place never, in fact, were. It never got done in the community right; if it had been, there would be many people out there doing better than they are now.”
Almost every Tuesday and Thursday morning for four weeks, at about 8:30, I made my way through downtown streets, headed for the courthouse to attend conservatorship hearings. Always, before I arrived at the courthouse’s entrance on Broadway, I would pass men and women clothed in layers of garments, waking up from the broken-down cardboard boxes and ragged blankets on which they slept. Often they were deep in monologue, lips moving rapidly, hands fretting with dirty sleeves and rubbing dirt farther into creases of deeply tanned skin.
On Union Street, between Broadway and B Street, I would sometimes be greeted by a tall, spindly black male who pushed a shopping cart. Inevitably, he was wearing a woman’s blond wig set askew on his head, several dresses, a skirt. His feet would be pushed into women’s high-heeled shoes, from which several inches of his own bare brown heels protruded. He would lurch toward me, pushing his cart before him like a battering ram and demand that I give him money for breakfast.
Farther down the block, there’s a bus bench at Union and B streets, protected from weather by a second-story corridor that runs from courthouse to jail. Some mornings a middle-aged woman, tousle-haired, with large, sentimental eyes that she rubbed with knotted fists as if she were recently awakened from sleep, would be sitting on that bench, her filthy dress hiked well above her knees. She would be raving to herself in a staccato demi-English. As one after another person passed by her, she would halt her rant and ask for money.
Once inside the courthouse, waiting in the hall by the door into Department 14’s courtroom and then observing what went on in that courtroom on Tuesday and Thursday mornings, it was impossible not to see and hear likenesses between many people living on the streets and people appearing in mental health court.
Late one morning, a man in his early 20s had been brought from a hospital to the courthouse because he had requested a writ hearing to protest his hospitalization and demand his release. Four male attendants accompanied him. He was seated on one of the wooden benches in the hallway, an attendant on either side of him, two standing in front of him. He was slight in build, young, surely not more than 22, cleanly and even elegantly dressed in silky black turtleneck and beige trousers; he was dark-haired and handsome. Every few seconds he would lunge forward, teeth bared, and bite at his attendants. They would grab at him, hold him down. He would buck, growl, lunge. People walking by moved quickly and looked away.
I began to feel how difficult it is for those of us who have little contact with the mentally ill not to feel uneasy in their midst. Our own stability often feels so tenuous. Several mornings when I went to court, I’d not slept well, I was tired; the air was hot and muggy, and the streets around the courthouse seemed an obstacle course of need and craziness. I would begin to feel ill myself, shaky and strained. I’d feel my own often fragile psyche, my dubious hold on things, threatened simply by the presence around me of what felt to be an abnormal subjectivity or so many and such varied aberrant subjectivities.
And on those mornings, when I felt weary and plagued by a certain dis-ease, what seemed my usual point of view took on an odd slant, a queer bias. Then, the obviously mad people living on the streets and men and women babbling on benches outside Department 14 would feel to me to be carriers, not of physical illness, but of some virus that broke down the psyche’s linkages to a here-and-now in which two plus two always equaled four.
Tuesday and Thursday mornings, psychiatrists milled about in the hall, waiting to testily as to why patients incarcerated in their facilities should or should not be released. Most dressed conservatively, in well-tailored suits. There was one man, bear-like and gray-bearded, who eschewed suits and wore rumpled wash pants and sport shirts. He had been pointed out to me as a psychiatrist. His name, I was told, was Yaroslav Kushnir.
One morning, in the hall, I approached Dr. Kushnir. He spoke an accented English. He said that his practice was made up principally of acute and chronic patients, many of whom were on conservatorship. I asked if he thought the LPS conservatorship system was better than the old civil committal system. He said, about the LPS system, “It’s like communism. It works great on paper.”
I said it would seem that horrible things must have happened to some of these people when they were children. Kushnir nodded. “Some of them do have terrible histories, that’s true. But that’s not enough. Chronic schizophrenics, they often come from good homes. Schizophrenia,” he said gruffly, “it’s like a cancer of the mind, once you get it... ” And then his beeper went off, and he excused himself.
The morning on which Mr. Wang, Mr. Guston, Miss Preston, Miss Anders were in court was certainly a very average morning of conservancy hearings. As I sat through many more mornings of these hearings, I became increasingly impressed by how so many of these men and women, diagnosed as suffering mental disorder, courageously managed to keep themselves going. And I came quickly to understand a comment by Judge Hammes. So many cases she hears, she said, left her feeling emotionally drained.
There was the woman in her mid-30s, carefully dressed, blonde, her brightly rouged face oddly ageless, who had been a conservatee for ten years. She was in court because she wished to be taken off conservatorship. According to the report submitted by county counsel, she was kept on conservatorship because, from time to time, she ceased taking her medication and had to be hospitalized. But she was able to live independently in a studio in one of the downtown hotels and explained, proudly, that her studio had a refrigerator, a microwave, a television set. Her rent, she said, was $312 per month.
The public defender asked the series of questions designed to show that her client was not so gravely disabled as to be unable to care for food, clothing, and shelter. She asked, “Who pays the rent?”
“I pay it.”
“Do you get a check every month?”
“Yes.”
“And how much is that check?”
“Seven hundred and twelve dollars.”
“And out of that you have to pay your rent and handle all your other affairs?”
“Yes.”
“How do you handle your budgeting?”
“I budget until I have so much money for food, and I don’t overspend on anything.
And by the way, last month I saved $300.” All at once, the woman sped up, saying, “And I am not hungry and I am not starving and I have clean clothes and I have a nice clean room and by the way,” she stopped, looked about the courtroom, smiled, “I am really a sweet girl.”
I thought, at that juncture, “What a terrible moment for an attorney,” as the public defender continued, asking, “You were hospitalized in December of last year. Did you take yourself to the hospital for medication?”
“Yes.”
“You were suffering from depression?” But it was all over. The woman had begun what psychiatrists describe as decompensation. She had made the leap from the here-and-now into delusion. “Over my children. That was caused because I had a daughter. I was having trouble with the baby in my body, in other words, I was pregnant.” She added, with great innocence, “I can explain how it happened.” And then she went on to say, “I plan about three years more in this county because I want to get a degree. I am in college right now. I am studying international relations, dance, and chemical dependency.”
Many mornings in conservatorship, I would see and hear that decompensation. There was the woman in her early 40s, diagnosed as schizophrenic, who had been brought, completely naked, by the police into Harborview’s emergency room, where, according to Harborview staff, she behaved violently. Previously, she had been in the state hospital at Camarillo and currently was in a closed, locked ward of a local hospital.
She wept, telling the judge her husband had left her, then, when she became ill, she lost custody of her children. She said she had been in and out of hospitals but had continued to be able to visit with her children on holidays and in the summer. Her children were scheduled to visit her soon. She begged the judge not to institute the conservatorship. She said, “I have always conducted myself as a lady. I have always slept alone.” And then apologizing for being “so emotional,” she sobbed, “I am forced to take medicine not made for me.” Then she pulled at her aqua blouse, which barely buttoned across her broad bosom, said, “and these are state clothes.”
A stocky man with close-cropped hair standing stiffly across his broad skull had been brought from Patton State Hospital for a re-establishment hearing. The psychologist whom I sat next to that morning told me that this man had suffered brain damage from sniffing glue. The man’s head twitched frequently, and his dark eyes, when he turned them toward us, looked as if acetylene sparks could shoot from them. An odd smile regularly fluttered over his lips. “He’s hallucinating,” the psychologist told me, “hearing voices.” Questioned by county counsel, the man spoke not one understandable word but seemed rather to detonate a series of husky gutturals, dream cries, gleeful bursts, murmurs. Judge Hammes ruled that his conservatorship be re-established, with the state hospital to remain as the least restrictive setting.
Conservatorship hearings in which family members address the court can be particularly heartbreaking. Miss Adams, a stylishly dressed, heavyset woman in her 30s, sat in the second row, next to a woman whose 20 additional years and similar features made it obvious she was Miss Adams’s mother. When Miss Adams’s case was called, she went to sit next to Steve Binder. Miss Adams had several months earlier attempted suicide. It was not her first attempt. She had recently been transferred from the hospital to which she was taken after her suicide attempt to a second hospital, where she was being held on an open ward. She was asking the court that she not be placed under conservatorship and be permitted to live with her mother.
Miss Adams listened intently as the psychiatrist from the hospital to which she was first admitted testified as to her condition. She was diagnosed as suffering a major and recurring depression. “During her entire hospitalization with us, which was approximately 55 days, she expressed almost daily that she was feeling suicidal, feeling very hopeless and helpless. Frequently she mentioned that, if she had the opportunity, she would kill herself.”
Miss Adams was sworn. In a strong voice, she said, “I am not gravely disabled. I can take care of myself as I have in the past. I just need to get myself together. I lost my twins, and I just lost it.”
Judge Hammes leaned forward on the bench, asked, “When did you lose your twins?”
“At about five months. And after that was when I came to the hospital. I brought myself to the hospital this last time, so I am able to seek help. I do take my medication, I do believe I should take it.” Miss Adams, with Judge Hammes’s prompting, went on to explain that six months ago, when five months into a pregnancy in which she was carrying twins, she miscarried. The twins were born dead. It was after that she made her suicide attempts. She hoped now, she said, to return to her job as an aide in a nursing home and to live with her mother until she got herself together.
Miss Adams’s testimony completed, Judge Hammes said, “I think her mother would like to speak; I have a little note from the bailiff.” Mrs. Adams walked to the witness stand and was sworn.
Mrs. Adams stated that she was not willing at this time for her daughter — Dorothy — to live with her. “I really don’t think Dorothy is as well as she thinks she is. It hurts me to say that. She is safe at the hospital. There is not anything there to put stress in her life. She knows her job is destructive. She works at a convalescent home, and in that job she sees death and dying, depression. It depresses her.
“She is more than welcome at my home but not if it is simply going to be a turnaround and in three weeks she is depressed and at the point of death again. If you let her go now, she is going to be where she was three weeks ago. She wants out. But I want her healthy, and she is not going to be healthy if she comes home now. She is not over all that she has gone through. And as I sat here I knew I had to say something. I know to her it is a horrible thing, but I know it is the only thing I can say.”
Judge Hammes asked, “Is it hard to testify in this way?”
“No, because it’s something that I feel it’s right. I am worried for her safety. I am worried for her life from now on, not only her safety for three months, but for the rest of her life.”
Judge Hammes ruled that Miss Adams remain in a conservatorship in her present facility. Outside in the hallway, the mother and daughter came face to face. The psych tech accompanying the daughter moved aside to let them say their good-byes. The daughter sobbed. Tears rolled down her cheeks. The mother stood dry-eyed, arms at her sides. She opened her mouth as if to speak, then said nothing, turned and headed toward the elevator.
Mr. O’Toole, a broad-shouldered six-footer in his late 30s, looking uncannily like Burt Lancaster in his title role in Elmer Gantry, wore a navy-blue suit, pale-blue shirt, rep tie, Cuban-heeled black boots. He strode with great bustling confidence from his seat among spectators and took his place next to Steve Binder, the public defender representing him. Mr. O’Toole seemed more like a successful political candidate about to receive the homage of a grateful party than a petitioner come to court to plead for disestablishment of a mental health conservatorship. Psychologist Gregg Michel, who had interviewed Mr. O’Toole earlier that morning, was sworn.
Questioned by county counsel, Michel noted that Mr. O’Toole “suffers from what we used to call manic depression, now labeled as ‘bipolar disorder.’ ” Mr. O’Toole, Michel went on to say, had been diagnosed as “manic with psychotic features.”
“At this time, in your opinion,” county counsel asked, “does he continue to be gravely disabled?”
“Yes, in my opinion, he is gravely disabled. During the first 30 minutes that I spent with the patient today, he had some passive signs of his illness. He became pretty agitated. He was fairly intact, except for orientation. He believed that the year was 1981.”
Mr. O’Toole, starting to rise from his chair, shouted out, “I didn’t say that. I knew that it is 1991.”
Michel ignored the outburst, continued. “After approximately 20 to 30 minutes into the interview, he began having more and more difficulty focusing and had to be refocused constantly and became very concerned about the outcome of the exam to the point that it was difficult to conduct it. He has trouble with his attention, concentration. [At the hospital where he lives] he is a management problem. He wishes to sleep in. He looks better than he is. He is not accepting treatment. He doesn’t like it.
“In the summer of 1990, when he arrived in San Diego, he was extremely decompensated, disheveled, and quite psychotic and required acute hospitalization. He can seem to behave very appropriately, but the psychotic process does come out with this patient to a great degree.
“He shows a lack of insight. He was not aware of budgetary need. I could not get him to give me a rational plan as to how he would care for himself, except to say that he might live in cheap hotels, use his SSI, and whatever money he had left over, for food. And then he started talking about how he would enjoy eating in very nice, very expensive restaurants like Tony Roma’s.”
Mr. O’Toole stood to be sworn. When he raised his right hand, his suit jacket lifted, revealing that his black belt had not been threaded through the belt loops at the back of his trousers.
County counsel asked, “What do you suffer from?”
“Bipolar. But it really is not so much a matter of suffering, is it? It is this matter of always being treated.”
County counsel asked how Mr. O’Toole came to be hospitalized. He explained he had come to San Diego seeking work, run out of money, lived on the street, was picked up by police and taken to Harborview. “At Harborview, they asked me, did I want a conservatorship? And I said, ‘Why not, I’ve never tried one.’ ”
He went on to say that he was taking Prolixin, lithium, and “a little blue pill.”
He added, “I feel totally compliant about medication.” He assured the court he felt far more in control than in November. “I feel able to be a total member of society. I have bought clothes. I am able to dress nicely, I go to high-class singles’ events. At the place where I am staying, I have made friends. The ambience there,” he fluttered his hand in the air, shrugged, “is not that unbearable.”
County counsel asked where Mr. O’Toole would live were he permitted to leave the hospital.
“I have a degree in hotel management. I know the whole motel and hotel scene like the back of my hand. All this talk about shelter, I ask you,” Mr. O’Toole seemed exhilarated, “how many places can one person stay? Food and shelter in the past has not been for me a problem. By September of last year, because I had been living on the street, I had simply become unkempt. This,” Mr. O’Toole gestured contemptuously toward county counsel, toward Michel, “is just a little song and dance I do when I run out of money.” Binder pleaded, “Mr. O’Toole, however awkward, is able to use community resources. Whether for shelter or the need for a restaurant. He was able to get clothing and food for himself, able to commit himself.”
But it was no go for Mr. O’Toole. Judge Hammes, noting that Mr. O’Toole “does make a rather good presentation,” went on to refuse to end his conservatorship. Her refusal appeared to do little to thwart Mr. O’Toole’s elation. Psych tech right on his Cuban heels, Mr. O’Toole left the courtroom as would someone who had just received a standing ovation.
Outside Department 14, Mr. Jernigan had towered over the psych tech who accompanied him to his re-establishment hearing.
Mr. Jernigan was in his mid-50s, dangerously thin, and his skin had a blue pallor, the bloodless cast that skin will take on when someone sits in a darkened room watching a television on whose screen some black-and-white movie is showing. He moved restlessly up and down a small patch in the hall and pulled at the sleeves of his hooded sweatshirt. Once in the courtroom, seated next to his attorney, Patricia Rosenberg, Mr. Jernigan put his head down on the table while Dr. Kushnir testified.
“He has come up to staff with his fists and threatened to hit them. They believe he would have struck them if they hadn’t taken action. This is one of a dozen overall admissions for him. He is having a hard time. He was living at an intermediate nursing facility. I believe they are maintaining very well for him. But about a week before his hospitalization, he began to skip on his medicines with the result that his psychosis became aggravated, and he was running down the corridors of the nursing home, bumping into elderly patients, demanding cigarettes, going into other people’s rooms saying he was King Henry and everybody was his subject. He wasn’t sleeping and was very disruptive.” What Mr. Jernigan wanted. Dr. Kushnir said, was to be let out of a locked facility and allowed to live with his brother in North County. Dr. Kushnir said he could recommend only a closed, locked facility for this patient.
His long, scarecrow-thin arm stuck in the air, Mr. Jernigan was sworn. Asked then by Rosenberg about his medication,
Mr. Jernigan groaned, “Oooooh, it’s bad. God, it’s bad. Makes me sleep all the time.”
“But does it also help you?” Rosenberg asked, and Mr. Jernigan lifted his head, grinned idiotically, and nodded in the affirmative. Rosenberg went on, “Did you hear the doctor testify that the staff was frightened sometimes of you?”
Mr. Jernigan said he knew, then added, “They took away my clothes and my wallet.”
“So that made you mad.”
“They took away my social security card.” Mr. Jernigan’s face shifted through expressions from rapture to grief. He began, then, to weep — a moist, noisy sobbing. “My brother has died.” He moaned, then, without any apparent segue, brightened and began to explain that his name was Charles Jacob Tudor, that he was now and had been, he shouted, “the KING OF ENGLAND.” As swiftly as he had brightened, Mr. Jernigan dropped back into weeping. He looked toward the bench, tears streaming, said, “I love you, Judge.”
Judge Hammes, appearing momentarily disconcerted, said to the court reporter,
“Let the record show that Mr. Jernigan alternates between crying and laughter.” Rosenberg plunged on, asked Mr. Jernigan, “Did you hit anybody?” “No.”
“Even though you got mad, you didn’t actually hit anybody?”
“Oh, no.”
“Mr. Jernigan, if you were released from the hospital, where do you want to stay?”
“I want to stay with my brother. In Del Mar. It is so pretty in Del Mar.”
“Do you have social security and SSI?” Rosenberg asked.
Mr. Jernigan muttered a yes. Rosenberg asked, “Do you have someone to manage your money for you?”
Mr. Jernigan laughed happily, burbled, “My brother, my brother.”
Noting that she didn’t often have the king of England in her courtroom. Judge Hammes ordered that Mr. Jernigan’s conservatorship remain in place, with the least restrictive placement to be a closed, locked facility.
Jeff Elias had told me that he and his fellow public defenders had puzzled for months over a question Dr. Hansen put to interview subjects in his mental-status examinations. “How,” he asked, “is an apple like a horse?”
Watching and listening to Dr. Hansen testify in court, at first I’d not much liked him. He seemed, somehow, very stuffy. Then one morning, during questioning about a patient with a history of alcoholism, Dr. Hansen was asked by county counsel if he believed that in the locked facility in which the patient in question was resident, she had been, as reported, consuming “one or two beers a day.” Judge Hammes suddenly leaned forward on the bench, asking Dr. Hansen about the facility, “They don’t provide beer, do they?” And Hansen, smiling wanly, had shot back, “They don’t do that. They are not like the French.” I began, after that, to reassess my opinion.
The offices of the San Diego County Mental Health Service’s forensic unit are packed into a first-floor wing of the county courthouse, with large windows overlooking Union Street. I went one afternoon to Hansen’s office to chat. His office is nothing more than a small cubicle into which are crowded a small bookcase, file cabinet, and three chairs.
He told me that he came to the forensic unit 12 years ago and is the only psychiatrist who works full-time there. In addition to evaluations for re-establishment of conservatorship, he evaluates accused felons. His favorites, he smiled, were “the great malingerers,” accused criminals who pretended to have been insane at the time they committed a crime or who affected being too insane to assist in their defense.
Testifying, Dr. Hansen always noted that he had talked for 45 minutes to an hour to a conservatee before he made his evaluation of that person’s present condition. Before the interview, he will have studied a report prepared by the Department of Social Services’ conservators’ unit, a report that will include information from the conservatee’s residence and treating physician as to progress or lack of same. There will be a medical and psychiatric history. Perhaps educational, work, and family history.
“Most people we see are troubled — depressed, anxious, irritated, confused. That’s what we deal with most of the time. In many cases, their memories aren’t too good; patients don’t always remember their own histories or they don’t want to tell you sometimes.
“A lot of these people never functioned too well before they became ill. It may not have been too obvious. I talked to the family of a young woman on whom I was taking a history. They said, ‘She was doing fine, then suddenly one day she started screaming and walking down the street and taking off her clothes.’ But talking further with them I learned that several years before this incident the young woman had sat in her room for a week and wouldn’t come out and wouldn’t talk to anybody.
Then she passed through that and seemed okay. But then several years down the line, she had this real obvious break that they couldn’t ignore.”
I had heard, I said, many conservatees described as bipolars, manic-depressive.
Dr. Hansen agreed. “A lot of depressives go through that courtroom. One of the most common things, and the tendency seems to increase with age, many of the affective disorders get worse as you get older. And a lot of bipolars, as they get older, get the episodes more frequently and they last longer.
“The manics are interesting. When you deal with a manic, if, in your diagnosis, you rely on him for your history, you should be charged with malpractice. Because with a manic, they feel good!” Hansen clapped his hands, smiled, and then suddenly looked dour, “Unless they are getting into trouble — perhaps swimming in the nude in a public pool.”
I asked Dr. Hansen about a test I’d heard him mention in court. He had asked a patient to name 24 wild and domestic animals in one minute. I had tried this, had asked friends to do it. The best that I or anyone I knew could do was to name 18 animals in one minute. “You’re okay,” Hansen said. “The range is 12 to 24.”
He went on to mention a case on which I’d heard him testify — Mr. Moody. “He told me he just blanked out or spaced out when he tried to do this. He got six, and then he spaced out. It’s a test of memory. First you have to remember it, then you have to retrieve it, and then you have to be able to express it. And some of these people can’t retrieve worth a damn.”
Hansen looked thoughtful. “Some people may be preoccupied with a lot of internal stimuli I can’t see. Sometimes you can’t observe the stimuli. But you can see they won’t be listening to you, they are listening to something,” Dr. Hansen pointed to his head, on which, from the windows, afternoon sunlight fell on the wispy grey hairs and produced a halo effect, “that is coming from up there.”
How did he ask people if they were hearing voices?
“I don’t ask them about voices or hallucinations. That’s one of the last things you ask. You start off by asking about racing of thoughts. There are some people who go through a period of time when their thoughts are racing rapidly through their mind, they can’t keep up, they stop, they go slowly, but their thoughts seem to speed up, keep changing speed. The person can’t keep up, so he gets confused. His thoughts just seem to be doing their own thing.
“The second thing I usually ask is, ‘Have your thoughts ever been so strong you could hear them?’ Then I ask, ‘Have your thoughts ever been so strong that they sound like someone standing near you reading your thoughts aloud or speaking your thoughts?’
“Then I would go to things like thought insertion."
"Thought insertion?
“Yes, thoughts you don’t like, thoughts that feel as if they are not your own. I might ask, ‘Do you feel that these thoughts are being put into your mind from the outside?’
“Or there’s thought extraction. A person may lose his train of thought and start thinking that a thought has been pulled from him from outside. Then you can go on to other things like thought broadcasting. I would ask, ‘Do you believe that your thoughts are broadcast, that people around you, when you walk down the street, are thinking the same thing you are?’ Or, ‘Do you think that you can broadcast your thoughts?’
“Or I might ask, ‘Do thoughts escape from your head, go out in the air? Do you believe people blocks and miles away can pick up those thoughts and know what you are thinking about?’ These are pretty standard things.
“A lot of them will say they don’t hear voices, so I kind of beat around the bush. Then try to zero in.”
I reminded Dr. Hansen of a conservatee whom he had evaluated who told Judge Hammes that he believed voices ascended from the radiators in the dining room in the hospital where he was resident, and therefore he was afraid to go into the dining room. On several occasions, this man had rammed his head into the radiators. What was this about?
“People frequently have a source they believe these voices are coming from. Which is why some people will smash their head on, for instance, the radiators, because they believe the voices come from there.
“I may ask in such a case, ‘Who do you think is doing it? Why?’ They often will tell you that an individual is doing it or a group. If they are paranoid, they may tell you the CIA is doing something to them. Or they tell me it’s electronics.”
Have delusions changed over time?
“The ‘who’ and the method, yes. They do keep up to date. They don’t lag too far behind. In the old days they talked about telegraphs. Today they talk about electronics. They say they are controlled electronically. Or by computers. You will be told, ‘I have a computer in my head, put in there by the CIA.’ ” Hansen laughed, “The KGB is out of business. They do pick up the fears and suspicions of the time that are abroad in the culture.”
I had heard only one person in court claim to be royalty. Did Dr. Hansen hear this claim as often as he did, say, 10 years ago? Or 20? He thought not. People don’t know as much history, he said. “But a lot of these people, they are somebody or they are about to become somebody.”
And people believing they are Jesus?
“I guess he’s the most important fellow in our Christian background, and of course, he’s the Son of God. I think this is a symbol of power and protection. ‘No one can hurt me. I’m such-and-such.’ You look at each one of these persons and try to run it down why they say such a thing. As they get better, they realize it ain’t so.”
One of the rights given to conservatees is the right to make determinations about medical treatment apart from treatment for their mental disorder. What did Hansen ask to establish a person’s ability to make these decisions?
“I usually come up with some symptoms. Say, ‘You got up, you went to the bathroom, you were passing water, you saw some blood in your urine, what would you do?’ If their answer is ‘I don’t know what I would do’ or ‘I would go back to bed,’ such answers would go against them. I also ask about symptoms of botulism, which is a very serious illness — blurred vision, double vision, can’t swallow, paralysis of the nerves. If they don’t say, ‘I would go to the doctor,’ I would say they are not very competent.”
What is it, I asked, this taking off of clothes and going naked down streets that I heard about several times in court?
“Some street drugs like PCP make people very warm. People get a lot of odd somatic symptoms. They seem to seize upon them. They may feel warm, they may feel flushed, they may get overactive, and they’re sweating,” Dr. Hansen smiled, made motions as if he were tearing off his shirt, “and off go the clothes!”
I asked about the number of people I had heard described as scratching themselves, cutting themselves.
“Some of these people have what is called anhedonia. It comes from an old Greek word, anhedonic. These people will take things to give them some feeling, to get sensation. You get some of these people under distress, they may cut on themselves. Some people will say, ‘It felt good, so I did it.’
“So-called borderline personalities, one of the common things they do is cut themselves.” Hansen paused, thinking.
“Very labile, the borderlines. They overvalue you one day and decimate you the next day. Very angry sometimes. They have a hard time getting along in life. A Spanish psychiatrist called the borderline personality disorder ‘the ugly personality.’ Very descriptive, but we wouldn’t dare use it.”
How many people he sees on conservatorship have been drug users?
“It’s hard to guess. And they don’t always tell you. But drugs play a big part. I can remember when in a state hospital, if you saw a drug addict, the person was usually a heroin user. Some sniffed cocaine. Most of the time, people using cocaine didn’t get into too much difficulty. It was quite expensive.” He laughed. “Tallulah Bankhead said, ‘Cocaine addictive? Hell, no; I’ve used it thousands of times myself.’
“A lot of people now who use, use several drugs — speed to get high, barbiturates or heroin to calm down. You keep bouncing around. These are real problems.”
Hallucinogens, he added, are “considered to be bad for schizophrenics. Some people think it may predispose them to cracking up. Many of our schizophrenics are pretty precariously balanced, and it may not take too much to turn them over.”
I asked Dr. Hansen if he thought the LPS conservatorship was an improvement over the pre-1968 civil commitments.
“There were criticisms of the commitment process. Among them, mainly, some felt that the hearings were very short.
I worked at Agnews State Hospital near San Jose, and it wasn’t as the opponents said, but they often did have very short hearings. At Agnews, they used to have a court at the hospital, and the judge would be there. It was efficient. A lot of the attorneys would often handle cases on the morning we went to court and often wouldn’t know very much about the cases or spend much time with the patients. Now you have a group of public defenders whose reputation and livelihood depend on what they’re doing, which makes our work a little harder.” Dr. Hansen paused, pursed his lips, said, “Probably it’s more just.”
No conservatorship hearings' were without drama. But one morning was particularly epic. Judge Hammes, earlier in the month, had ordered that the Dario Gonzalez matter, in which 15-year-old Dario had asked to be allowed to leave Camarillo State Hospital and return home, be carried over until she had time to talk with Dario’s family and doctors. Today she was to announce her decision. Public Defender Patricia Rosenberg, Dario’s attorney, stood in the hall chatting with Dario, Dario’s father and younger brother.
Jeff Elias was there, blue case folders stacked in his arms. I told him I’d been to see Dr. Hansen and had asked the answer to “How is an apple like a horse?” Elias looked so hopeful that I hesitated before I said, apologetically, “They are both living things.” Elias groaned.
During the mornings I’d attended conservatorship hearings. I’d struck an acquaintance with a court-watcher. He directed my attention to a particularly chic and terribly thin woman in her mid-40s — Mrs. Raines. He said he knew this case and that checking the calendar posted next to Department 14’s door, he noted that Mrs. Raines had been brought from a hospital to court for a hearing on establishment of conservatorship.
Mrs. Raines sat on a bench outside Department 14, talking with a handsome, well-barbered, conservatively tailored man who appeared several years her junior. He was, my informant said, her husband. On Mrs. Raines’s other side sat her privately retained attorney. A young woman, whose small mouth, large blue eyes, and taffy-colored hair suggested she was Mrs. Raines’s daughter, stepped off the elevator and walked slowly toward Department 14. The young woman stopped for a moment, said hello to her mother, and went into the courtroom. I noticed that the daughter did not speak to Mr. Raines, that she, in fact, studiously avoided his glance.
Shortly before ten, Judge Hammes requested that county counsel, the Gonzalez family, Dario’s lawyer, and several doctors meet in her chambers. Minutes passed.
Mrs. Raines became increasingly nervous, restless. A psychiatrist from the hospital in which she lived was present, pacing the hall. Mr. Raines stood, went to him, introduced himself. They talked quietly.
My informant explained to me that this was the second time this spring Mrs. Raines had appeared in court. Several months before, she had been hospitalized as an involuntary patient and had sought a writ hearing. At that time, her daughter had testified she believed her mother able to care for herself, and Judge Hammes had ordered Mrs. Raines released. Recently, against her wishes, Mrs. Raines had again been hospitalized. Mr. Raines, I was told, was Mrs. Raines’s second husband and not the father of her two children. Further, I was told, the Raineses were separated. I suggested that they seemed quite friendly today, and my informant agreed. When Mr. Raines returned to sit by his wife, he pecked her cheek, patted her arm.
An hour had gone by when Judge Hammes’s bailiff called court back into session. At the defense table, Dario Gonzalez sat next to Patricia Rosenberg. Dario’s father and brother sat among spectators in the first row. Judge Hammes, with great solemnity, announced she had decided Dario could leave Camarillo to go home to live with his family. She added that she had given Dario and his father her phone number, at home and at the court, and urged them, should they have any problems or questions, to call her, day or night. She looked, for a long moment, into Dario’s eyes, then said, “Good luck.”
The Raines matter was called. The psychiatrist from the hospital in which Mrs. Raines was resident came to the stand and was sworn. County counsel asked, about Mrs. Raines, “Have you formed a diagnosis as to her mental condition?”
“Yes, I have. She has a bipolar mood disorder, manic phase.” The psychiatrist went on to say that, in his opinion, Mrs. Raines was so gravely disabled as to be unable to provide for her food, clothing, and shelter.
He continued, “After her release from the hospital after a writ hearing, my understanding is that after she returned home, she continued to manifest the severe symptoms of her psychiatric illness. I understand she resided or remained in her bathroom, a small bathroom in the home, for much of the time because she feared allergens in the air were affecting her. I understand she ate very poorly while at home.”
Questioned further, the psychiatrist testified he believed Mrs. Raines showed no insight into her illness, indeed she believed she had no psychiatric illness or disorder.
He said that although she had initially refused medications, she had recently agreed to take them, but only under duress. He was concerned that were she to be released, she would discontinue medications, and her symptoms “would again worsen or at least continue.”
Mrs. Raines’s attorney began his questioning of the doctor. The attorney explained that his client wished to be released to her husband. What was the doctor’s opinion about such an arrangement?
“She has a history of a very difficult relationship with her husband, and in fact, there is a divorce pending. They have been separated, I believe, at least for a year, if not a year and a half.
“Precipitant to one of her first admissions to the hospital was a belief that her husband was trying to harm her in some way or that he was releasing laser beams or laser beam holograms on a closet in which she was hiding. She has a history of being very fearful of him and that relationship. So I am concerned that would not be, at least at this point, a proper placement for her.”
Further, the doctor believed that were Mrs. Raines to be released to her husband that Mr. Raines would not be able to convince her to take medication.
Mrs. Raines was then sworn. Asked if she would take her medication, she spoke in a voice like that of a young girl and nodded obediently. “Yes, I definitely believe I need to take that medication.” She added that she thought the psychiatrist was under the impression that she and her husband were being divorced when, in fact, they were reconciled. “And,” she said, “we are going to stay married, and I would very much like to live with my husband.”
Mrs. Raines’s testimony ended. Judge Hammes noted that Mrs. Raines’s daughter Tiffany had asked to testify. The young woman, seeming entirely self-possessed, strode to the stand and was sworn.
As Tiffany spoke, no one in the courtroom moved, and all eyes, including those of Mrs. Raines, were on the young woman. Her story poured from her. She began at the point her mother had last been discharged from the hospital. “I took her home. I showed her a bill; we had a stack like that.” Tiffany held one hand up to indicate a stack perhaps a foot high. “I said, ‘Mom, what should we do?’ And she ignored it. Right away when she came home, she turned on her radio. Like, before she went into the hospital the first time, that was her big thing; all she would do was listen to the radio and dance around.
“The second day, she started locking herself in the bathroom. She did that for five days. From ten in the morning, and each day it got longer and longer. I’d get really worried. The bathroom is small; you can’t even lie down in it, there’s just a toilet, the window has a curtain on it, and there’s no light.
“The second day she got home, our car was supposed to be repossessed. When I told her about that, she didn’t care; she said, ‘Oh, well, we’ll have to do something.’ But she didn’t want to talk about it.... So I ended up hiding the car. I thought, ‘God, we have to have a car.’
“And then the food situation got really low. I purposely didn’t buy any because I wanted to see what she would do. I told her, ‘We still have the car. You can go get yourself some food.’ The last day she was there we had condiments, like, mustard and ketchup, and three cans of soup.
“The last day, she was in the bathroom from four in the afternoon until the next morning. I was so scared. She was so skinny she could die without more food. So I called the ambulance, and when they came she was still locked in the bathroom.”
“Your testimony,” Judge Hammes said, pleasantly, “is somewhat changed from before.”
Tiffany nodded, quick little up-and-down bobbings of her head. “That’s actually what I wanted to say. When I visited her at the hospital — because my stepdad had, like, actually physically and verbally abused her and because she was scared of him, physically.” Tiffany paused, looked into her lap, “and in the hospital, she said, ‘Tiffany, I am getting worse and worse.’
“So when I was here the last time, I didn’t really say what she was doing at home. I would like to say some of that stuff now.
“In January when I left for school after Christmas vacation, she was fine. We would talk on the phone, like, every night. And things she said started getting really weird.
“She said people were coming to our house in the middle of the night and during the day, and she didn’t know who they were. And she said my stepdad [Mark] was trying to kill her, and I guess she thought my sister was in on it with him too.
“She was sleeping in the closet then. She said my stepdad came to the door with a turban wrapped around his head and nails strapped to his fingers, and he was motioning like this,” Tiffany crooked her index finger, wriggled the finger beckoningly, “that he was going to hurt her, and she said she actually saw this, which really scared me.
“She said another time that she heard my stepdad, I guess having sex on her bed with my sister, and she told them to leave, and I guess they continued, and I said, ‘Well, Mom, did you see this?’ And she said yes.
“She said she got out of the closet and went and looked, and the two were hunched over the bed, and the girl had a gun. That freaked me out. So I called my sister; she was at school. She wasn’t at home.
“Another time, my mom said a helicopter landed in our back yard and the people came inside and were walking around.
“All along, though, she said she was being protected. I said, ‘Well, Mom, what are you talking about?’ And she said that her lawyer had contacted the FBI and that the FBI men were living in our house, and they were living in the attic and under our floor, and we don’t even have a basement, so I don’t know where they’d be living.
“She said they were waiting there until Mark came there and tried to kill her. She kept calling it a sting operation, that they had to witness him trying to kill her before they could arrest him. So she said that was what they were waiting for, and I said I was getting really scared, and she kept saying, ‘Trust me. Trust Randy.’ Randy’s her divorce lawyer.
“Then she said she started watching holograms in her closet, and Mark was good at computers and that he had put them there. She said they were movies, and she would sit there and watch them, and most of them were, like, her being tortured. One she said was my stepdad and my sister and they were, like, shoving animals up her, and she said she watched these for hours.
“I was getting really scared, I said, ‘Well, Mom, when you are watching these movies, are you eating?’ And she said, ‘Oh, sometimes the movies are really good so I don’t want to leave, and when I ask the movies to stop, they don’t, so sometimes I don’t end up eating.’ So that really scared me too.
“I called her one time and she started talking to people in the same room. I’d be crying and sobbing and saying, ‘Mommy, I don’t believe you,’ and she’d be laughing.
“All along it would be, like, the opposite of what it should be. All these months I never cried so much in all my life, and every time I cried, she kinda smiles, like, ‘Oh, life is great.’
“So I was talking to her on the telephone, and she started talking to other people in the same room. ‘Mom,’ I said, ‘who are you talking to?’ ” Tiffany lowered her voice, imitating her mother, “ ‘Oh, it’s Randy and the FBI men.’
“And I said, ‘Mom, will you please put one of them on the phone for me?’ And then she said, ‘Yeah, hold on.’ I could hear her go down the hallway and call, ‘Randy, Randy, will you please come here? Tiffany doesn’t believe that you’re here. Will you please come to the phone?’
“And then she came back, laughing. ‘Oh, it was bad timing, Tiffany, they just left!’ And I go, ‘Oh, my God.’
“So then I came home from school the next day. She was in the closet lying there. And I put my arm around her, and first she kind of responded, and then I let my arm go and she got really cold and, I don’t know, that night was probably the worst night in my life. She was just,” Tiffany narrowed her eyes, stared off into the courtroom as if remembering, “like, the whole time she, like, looked at me, and I will never forget how she looked, like she was possessed or something.
“She thought, I guess, that I was trying to kill her too. I said, ‘Mom, I was not trying to hurt you, you know. How could you think I was trying to hurt you?’ It was awful. During the night, she would say, ‘Do you hear that?’ and I would say, ‘No.’ And I told her I would stay up all night to make sure that no one comes here and hurts you.” Judge Hammes leaned toward Tiffany. “Can I interrupt you? You can’t help your mom right now. It’s beyond your help.” “Well, I don’t know. I’m afraid of my stepdad. If she goes to live with him, he could like ... I don’t know, I mean. I think in the hospital at least they give her medicine. I don’t know what to do. I don’t know.”
Judge Hammes again interrupted Tiffany, “I think that she needs medicine. I don’t know what else to do. Tiffany, thank you so much.”
The judge’s face was somber as she ordered that Mrs. Raines be placed under conservatorship and remain in her present hospital setting.
In the late afternoon I visited with Judge Hammes in her chambers. She had just returned from meeting with two psychiatrists about an 11-year-old boy in an LPS conservatorship. “Articulate, bright, looks you right in the eye, and then you read about his background, and you just have to cry. Too horrible to believe! Wandering around the streets at the age of seven because he hadn’t had anything to eat for three days. Didn’t know where his mother was. Scars all over his body. Placed in a foster home. Brother makes it, he doesn’t. He’s acting out.
“Of course, a child who reacts in a hostile fashion to abuse and abandonment and neglect can’t make it in a foster home, so what happens? The only way that they can get help sometimes is to get into a state mental hospital. It’s so sad it’s beyond words. It’s just awful.”
Judge Hammes said that she’d posed a hypothetical question to the psychiatrists. She’d asked, “What if a child came to you, and the evidence was he had a conduct disorder, and you said, ‘That’s not a mental disorder causing a grave disability.’ What could be done?
“They said that would be horrible, because then you wouldn’t have a place for this kid. He would run away from a foster home, destroy a foster home, he would end up on the street, end up as a prostitute somewhere because you didn’t bring them into the system where they can get help. “Well, those are our choices? Pathetic.” Before Judge Hammes took over the mental health court in January, did she have any idea the magnitude of problems that would come before her?
"No. I had talked to some of the judges who had done this, and they had let me know there would be a lot of stress in this department. I was not aware that juveniles would be involved. I thought it would be only adults. And it’s always the kids who get you. Adults, you figure, ‘Well, by this time there’s not much you can do.’ You feel bad, but it’s not like a child.
“You know what I’m shocked to find out? I worked in juvenile court for two years, early on in my career, and I did a lot of child-dependency and sexual-abuse cases. I worked back in the early ’70s, before the real tide had come in of a big concerted effort to combat child abuse and neglect. Back then, sexually abused children were basically treated as a non-victim. It was like, they’re so young, they’ll be fine.
“In these cases of sexually abused children, however, it’s not like you pulled out a gun and shot someone and you can see the blood. We can’t see it; and six months from now, they have a hard time describing it; ipso facto, there’s no victim. Well, that is simply not the fact.
“Now l am seeing it here, and I am shocked; I am reliving all this earlier stuff, because many of these reports coming across my desk show that these schizophrenic women were sexually abused as youngsters, and schizophrenia took hold shortly after that abuse, and now they are mental patients.”
Traditionally, in San Diego, the mental health court is a five-day-a-week, mornings-only court. In the afternoon, the judge who sits on the mental health bench handles criminal law and motion matters. Judge Hammes said that when she asked to be assigned to mental health court, she did so because she was interested in the criminal law and motion calendar. About the mental health half of her job, she said, “I really didn’t know what I was biting off. Had I known!”
The mental health calendar, she suggested, deserves more time. “Basically, these people are being detained in lockup facilities, and when you consider how many and how fast these decisions are being made, it’s really something else.”
And preparation is time consuming. “Making sure you get everything read! Every time I jump off the bench, I am back in my office, reading.”
Mental health court, she said, is much like small-claims court. “More informal. Lots of hearsay evidence comes in — not at all like the criminal field. And I like this. I think this is closer to pure justice. Actually, I’ve often thought that small claims is the real, pure justice, because both sides can talk. They are, of course, going to offer you some irrelevant material, but in this often spontaneous way, real important stuff gets told to you that might not get told when somebody’s trying to hone to rules. So in a much shorter time, you can get a clearer picture than you can when everyone travels these narrow lanes. It’s much easier, frankly, to get at the truth.
“It is hearsay. But it’s permitted by statute. I am so schooled in criminal law that I still look askance at hearsay, I still go at this hearsay with a little question mark in my brain, and I ask myself, ‘Did this really happen?’
“Things that are important to me are ‘How many hospitalizations?’ That’s usually a verifiable fact. And ‘Has this person a long history of hospitalizations?’ And ‘When they were brought into the hospital, were they brought in by a friend, or by police?’ And ‘Did the police report they were wandering in traffic?’ Because, usually, to get a police officer to pick you up, you have to be doing something pretty extraordinary. Those are the kind of hard facts that tend to be most impressive to me.
“ ‘What is a person’s right to be on the streets?’ is another issue that comes into these hearings. You see people who come in here and who want to live on the streets and do not want a conservator, and you are forcing them to live in a home where there’s a bed. People from liberal and conservative backgrounds cross in this area. And when I had to sit down and think about it, I came in my own mind to the feeling that I don’t personally think that a person should have either the right or the misfortune to be living on the street, full of lice, without health care, without proper nutrition. So that I don’t agree with the side that says if they choose that, they should have it. I don’t think that’s a human, rational choice. Even if they can sound pretty rational and tell you they would prefer that to some other thing, I don’t think they should have that right, if that’s what they want to call it.
“I consider all of it a misfortune. I suppose there are some cases where you might call it a choice, but I still have such a hard time dealing with that. I don’t think you should have it as a right, and if nothing else, from a cold perspective, I don’t think that you do have a right to make it so that when I walk down the street with my kid that I have to explain this horrible situation to my children. I don’t think they should see human beings living like that. I think it’s such a terrible thing that you just can’t do that. You have to find a way to help these people, and if they don’t want the help, then you make them. That’s what I think.”
Did she believe her months on the mental health bench would change her? “It certainly is an eye-opener. You see how vulnerable life makes you. Everybody, all of us. You feel empathy for the people on the other side of that bench, because they could be you or your family member. You feel a little less secure.”
So many cases she hears, she said, left her feeling emotionally drained. “You take them home. You can’t get them out of your head.”


"What makes this court unique is that were dealing with people who haven't committed crimes, they're ill, ” said Paul Parris, acting that day as bailiff for mental health court, held in Department 14 in the downtown county courthouse. “When these people run, we call them ‘elopers,’ not ‘escapees.’ With an eloper, when I call for assistance, I will say, ‘Don’t come in with guns drawn. If they run, you don’t tackle them and crank on them like you would an escaping felon. These are sick people, citizens.’ ”
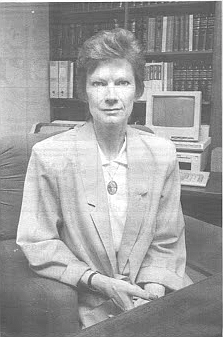
Outside Department 14 is not the ordinary courthouse crowd. Certainly some clothing selections are peculiar — a blue-and-red Madras plaid shirt, for instance, worn with green and gold and tan plaid trousers, and a woman in her late 30s with a bulky muumuu falling down over her body, and a big girlish bow stuck incongruously at one side of her head, and thin lips over which lipstick is smeared as if a child had colored in a coloring book and gone over the lines. Gestures are odd — exaggerated, even operatic in some cases, and in others, jerky and repetitive. Eyes wander, then fix on empty space as if the eyes see something or someone. Many talk to themselves. And perhaps as many hunker silently, as if in the grip of terrible lethargy.
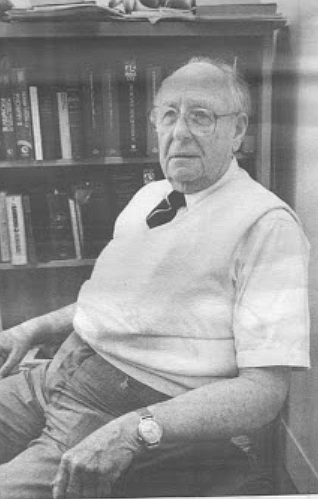
Seated on one of the wooden benches that line the hall, under windows that look out onto the jail, a pretty young woman wearing a sleeveless blouse lifts her right arm, carefully sniffs her armpit, then lifts her left arm, sniffs that armpit, frowns. She repeats this sniffing, first one armpit, then the other. She breathes in her odor so deeply that the sound of her breathing in is audible. A man with a laminated photo ID clipped to his shirt stands near her, at the bench’s end. She stops sniffing, presses her arms tightly against her sides, and with eyes suddenly wide open, as if in fright or shock, she asks the ID-clipped man if she may use the bathroom. He says yes, and when she rises to her sandaled feet and in a shuffling, irregular gait walks toward the women’s room, the man is right behind her.
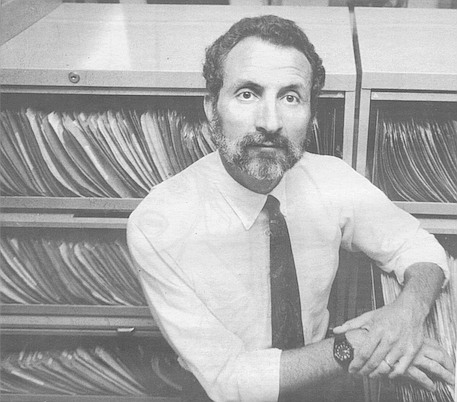
Nearby, on another bench, a plump redheaded male wriggles restlessly. He mumbles into his lap, scratches at his trousered legs, grins into the vacant middle distance. His fingernails are chewed to the quick, and the cuticle on each of his fingers is lined with a thin margin of dried blood. Up close he has a sickish, lone, and breakable look. He seems to speak to someone standing before him on the hallway’s brown tiles. No one, of course, is there. After a moment’s fierce staring and a quiet babble that is a cataract of vowels — ooooh and aaaah and oh — he turns, asks querulously of the woman next to him, “Can I have a cigarette now?” She says no, he can’t, he will have to wait until after he talks to the judge. He asks again. She says no. He returns to his intense gaze at emptiness and to his ooohs and aaaahs and ohs.
The young woman, someone tells me, is schizophrenic, with a symptomatology that ranges from command auditory hallucinations to covert feces-eating. The man following behind her is a psych tech from the hospital in whose closed, locked ward the woman has been kept, against her will, for the past three weeks. The redheaded male is manic-depressive; he lives in a locked facility. He and the armpitsniffing young woman, heading back now from the bathroom to her bench, have been brought here, I'm told, for conservatorship hearings.
Tuesday and Thursday mornings, Department 14 is reserved for conservatorship hearings. In 1968, California’s Lanterman-Petris-Short Act (called the LPS by lawyers and mental health professionals) changed the law under which mentally ill persons could be committed to institutions. Before 1968, a document submitted to Superior Court by a psychiatrist, indicating that a person was mentally ill and required hospitalization in a state or private mental hospital, could be enough to put that person away for life.
Mental hospitals were warehouses for the mentally ill, many of whom never left. And once in the hospital, the mentally ill had few legal rights.
LPS tightened standards for committal, set limits on how long a person can be held without court hearings, required that treatment take place in the least restrictive setting closest to the person’s home, and increased in scope and number legal rights left to persons diagnosed as impaired by mental disorder or chronic alcoholism.
LPS conservatorship replaces pre-1968 civil committal. In simplest terms, it gives decisions regarding a person’s care to someone other than that person. Approximately 2200 people in San Diego County are LPS conservatees. Of that number, some 100 are in state hospital beds.
The rest live in the county, either independently or in board-and-care facilities or in one of 22 local hospitals that provide treatment for mental disorders.
A person will not be placed under a conservator’s care simply because he is diagnosed as suffering mental disorder or chronic alcoholism. The Superior Court must also find such a person so gravely disabled as to be unable to provide for his food, clothing, and shelter. And the court must find that no one else is able and willing to meet those needs£ As one psychiatrist explained it, “You can be as nutty as a fruitcake, but if you can provide food, clothing, and shelter for yourself, you don’t have to accept treatment for your disorder, and you can come and go as you please.”
Inside Department 14, the spectator section is divided into three rows, each with a dozen seats. This morning, perhaps half these seats are taken. I count half a dozen persons who are subjects of these hearings, including the pretty young woman, seated now in the first row; she continues, although more furtively, sniffing her armpits. Also present are psych techs, assigned to watch those who are here from hospitals, and county transport aides who’ve driven people to court from board-and-care facilities. Psychiatrists are here to testify as to why a person resident in their hospital should be placed on or kept under conservatorship. A psychologist and a psychiatrist are here from County Mental Health’s forensic unit to testify as to the condition of persons already on conservatorship who wish it to be ended or its conditions amended.
Behind the bar sits County Counsel Janice Ingold. County counsel represents the Superior Court’s Counselor in Mental Health, the agency that initiates LPS conservatorships, and the Department of Social and Health Services’ conservators’ unit, whose social workers act as public conservators for the gravely disabled. (Of the approximately 2200 people currently living under LPS conservatorships established in San Diego County, some 500 have private conservators. The other 1700 have public conservators.)
At what would be the defense table in a criminal trial sit members of the office of public defenders’ five-member mental health team. Then there are court clerks, a court reporter, a bailiff.
Superior Court Judge Laura Palmer Hammes addresses those present for conservatorship hearings. She begins by reviewing procedure. “I will listen to the doctor’s testimony, I will read reports in your case, I will listen to what you have to say and to any witnesses brought on your behalf. Then I will make a determination as to whether, by reason of mental disorder, you need a conservator to assist you with the daily function of life, that is, food, clothing, and shelter.”
A tall, slender redhead with a china doll complexion and delicately modeled features, Judge Hammes was a deputy district attorney in San Diego County from 1972 to 1984. She was appointed to the Municipal Court bench in 1985, to the Superior Court in 1986, and to mental health court in January of 1991. A judge will generally serve one year in this venue.
Judge Hammes leans forward on the bench, speaks conversationally. “If I determine that is the case, then I would appoint a conservator to assist you. The conservator could either be the public conservator or a private conservator — that is, a friend or family member who would assist you with these functions.
“Then I would decide least restrictive placement for your living — that is, the type of living arrangement, not the specific place where you live. That is determined between you and your conservator. That could be anywhere from independent living (that is, living out on your own) all the way up to a closed, locked treatment facility or a state hospital level.
“I then must determine what rights may have to be restricted in your case — that is, whether or not you should have the right to possess a firearm, to vote, to contract, to make medical decisions that are related or unrelated to your mental disorder.
“You have certain important rights with respect to this morning’s hearing. You have the right to contest conservatorship, to say, ‘I don’t think I need this,’ and tell the court why. You have the right to the assistance of an attorney. If you cannot afford an attorney, then the public defender, who is very skilled in this area, will assist you. If you can afford an attorney and wish to bring in your own private attorney, you may do that as well. You also have the right to a jury trial. After this hearing is over, you may request a jury trial in this matter.
“It’s important to know that if the conservatorship is established, it will last for only one year and that it must terminate after that one year, unless it is reestablished by another court hearing.”
Wang’s case is called first.
(Although conservatorship hearings are open to the public and a matter of public record, all names of conservatees or potential conservatees have been changed, as have some details such as physical traits, to disguise identity.)
Gregg A. Michel, Ph.D., a member of County Mental Health’s forensic unit and a psychologist in private practice, is called to the stand to testify in behalf of the county.
Mr. Wang — stooped and somewhat wan, wearing dark trousers, white polo shirt, and beige cardigan — has waited outside in the hall. He is brought in by the bailiff and directed to the defense table, where he’s greeted by his attorney, Steve Binder, a member of the public defender’s mental health team. In front of Binder on the table are stacked pale blue case files in which clients’ records are kept.
Binder several weeks earlier visited the board-and-care in which Mr. Wang lives and talked with him about his reestablishment hearing. Mr. Wang had asked that Binder get him removed from conservatorship.
Like all judicial proceedings, these hearings follow a course. Testimony drawn out by county counsel, asking either for conservatorship or re-establishment of conservatorship currently in force, is designed to elucidate the person’s status as gravely disabled. The defender has the burden of proof. It is his job to show the person not gravely disabled.
County counsel opens by questioning the psychologist or psychiatrist who has evaluated the conservatee.
Seated in the witness box, Gregg Michel (pronounced “Mitchell”), a dark-haired, clean-shaven man in his 40s, is sworn in by the clerk.
County counsel begins, “Doctor, have you had an opportunity to examine Mr. Wang?”
Michel answers in clear, strong tones. “Yes, I did. I saw him here in the courthouse in the forensic evaluation unit....”
“Have you formed a diagnosis as to his mental condition?”
“Yes, his current diagnosis consists of what is called schizophrenic disorder. In the past, he’s been diagnosed as suffering from schizophrenia and later with ‘bipolar’ — what used to be called manic-depressive illness. His current treating physician feels that schizophrenic disorder is the most appropriate diagnosis, and I concurred with that assessment.”
“As a result of this mental disorder, is it your opinion that he’s unable to provide for his own food or clothing or shelter without assistance?”
“Yes, it is.”
“What about Mr. Wang’s functioning led you to believe that he is unable to provide for his basic needs?”
“The essential situation with this patient is that he tends to decompensate and require acute hospitalizations. When given appropriate medications, he then responds well and stabilizes. There has been a repeated cycle of this occurring.
“The current problems really have to do with his needing more insight into his own needs for treatment.... He evidenced some symptomatology that was relatively passive — illogical and psychotic thinking, difficulty in sequencing thoughts, some relatively mild depression.”
Mr. Wang, says Michel, is “ambivalent about taking medications and hopeful he may not need them in the future.” Further, says Michel, “He indicated that sometime in 1990 he had gone off medication because he didn’t like his previous board-and-care. He didn’t see judgment problems inherent in that.”
Michel notes that Mr. Wang is 38 years old, that he was first diagnosed at 19 as having a mental illness, that he has lived in a series of board-and-care facilities, and that in the past four years he has been hospitalized several times in an acute-care facility. Mr. Wang’s ceasing to take medication and subsequent decompensation was a pattern that, according to Michel, is not uncommon. “Patients stabilize and do relatively well and then begin thinking that they can do without medications. When they try to go off them, then you see the cycle continue.”
Then begins the litany of questions always asked by county counsel. “Is he capable of operating a motor vehicle?” “Of entering into a contract?” “Making medical decisions unrelated to his mental disorder?” “Completing of a voter registration form?” “Might he be a danger to others in possession of a firearm?”
Michel considers Mr. Wang capable only of making medical decisions unrelated to his mental disorder and filling out a voter registration form. Michel believes Mr. Wang would be a danger to others were he in possession of a firearm “because he does have a history of acting out, of being impulsive. That is a continuing problem, according to board-and-care staff.”
County counsel asks Michel, “In your opinion, at this time what is the least restrictive level of placement for him?”
“At present, my opinion is that a board-and-care facility is appropriate, because he still requires prompting to eat, to take medications, to go to treatment. I think, though, that the goal for him in the very near future should be independent living.” Public defender Binder begins questioning Michel. “You noted that he ceased medications in 1990 in order to get out of the board-and-care in which he was living?”
“Well, he said his reasons for ceasing medications there were because he didn’t like the board-and-care.”
“He did specifically state that it was dirty and he didn’t like being there?”
“Yes.”
“Have you been to that particular board-and-care?”
County counsel objects. Judge Hammes overrules the objection, directs Michel to answer. “No,” Michel states, “I haven’t.”
Binder queries Michel about Mr. Wang’s recent compliance with taking medication and attending day treatment. Michel notes that Mr. Wang has, with prompting, taken medication, attended treatment.
After more questions from Binder to Michel, questions intended to permit Mr. Wang to establish his ability to live without conservator’s supervision, Mr. Wang is sworn. Binder asks his client,
“You understand the doctor’s concern that off conservatorship you may cease to take your medications?”
“I would like to explain to the judge that this has occurred in the past, but my mind has stabilized to a point where I am more coherent within myself and in my surroundings. So I am willing to take medication at all costs.”
Judge Hammes asks, “What are the costs?”
“I don’t know the costs, but at all costs. I mean, it’s really destroying your life if you are not taking medication if needed.”
Judge Hammes asks, “What do the medications do for you?”
“I am not sure. I know my thinking is not as clear as it used to be, Your Honor. And it seems like maybe the doctor right now has doses a little bit high, but I will continue taking my medication, because life is very precious and, you know, I don’t have 35 years left on this earth. I want to get a job. I want to work. I have two years of college. There is a lot of free time when you are on disability and it’s no fun. I would rather be industrious and do what I have to do and contribute to life.”
“What happens,” the judge asks, “if you cease your medications?”
“Well, at present, I think it would be unfeasible. I think I have a good relationship with the doctor. I think he knows me better than myself at times. He’s a good doctor. I want to stick to him. But I don’t have enough time to talk to him. He’s a real fast-acting doctor. I tell him I want to tell him something, but everybody crowds around and starts talking and I can’t get through the right amount.” Mr. Wang goes on to say that he would like to request a new social worker “because this one doesn’t help me out, doesn’t even talk to me sometimes.”
Binder asks Mr. Wang, “Why did you cease taking medications?”
“Because I was scared. It’s bad — the neighborhood isn’t as good as it was — and it’s like a dungeon where I slept. The lady is okay, but the environment is dark all the time, and it scared me, you know.”
County counsel questions Mr. Wang, “Do you have many friends at the board-and-care or in your day treatment?”
“No,” Mr. Wang answers, expression hangdog. “That is the problem, how I couldn’t resolve the schizophrenia because I don’t want to fool around with those people. I mean, you know, it’s a bad influence. That is why I ran away from the other board-and-care, because it’s a bad influence. I am not comfortable. I run to the doctor. But they should have the board-and-care where I am now checked out because there is no hot water there, and I am scared, Your Honor.” County counsel has no further questions. The judge speaks, notes that based on Michel’s testimony, observing Mr. Wang, and reading the report, she believes conservatorship should be re-established. She adds that she thinks Mr. Wang has “legitimate concerns about medication,” that “without any question, there needs to be more dialogue about medication between Mr. Wang and his treating physician.”
Judge Hammes looks directly at Mr. Wang, whose mouth has turned petulant. “I understand what you are saying. I understand that you are saying, ‘I don’t like the side effects of these medications.’ At the same time, the history says that when you are taking medications, you don’t engage in behaviors that end up getting you picked up by police and brought back to the hospital. I think you know that too, so it’s a matter of getting it worked out. You have to live with some unpleasant side effects in order to stop those bad behaviors.
And apparently Dr. Michel thinks that you are very close to getting it worked out, and he thinks in a few more months of getting stabilized, you should be okay for independent living. So I think there is good hope for you.” Judge Hammes wishes Mr. Wang luck and turns then to county counsel, suggesting a note be made in Mr. Wang’s file that he would like to have further talk with the social worker.
This morning, some 20 uncontested I nonappearances are on calendar.
Judge Hammes wishes, before she proceeds with other cases, to run quickly through these. Jeff Elias, the tall, rangy, fast-talking attorney who heads the county’s public defender’s mental health law team, begins. “I saw Mr. Jones at Edgemoor. He was able to respond. Unfortunately, he rambled. He actually refused to discuss why I was there or what was being proposed. I am sure that he heard me. Either he was unwilling or unable to cooperate. When I asked if he wanted to attend court and contest or be involved in the procedure, he became very agitated and told me to leave.”
Judge Hammes glances up from papers spread open before her, asks, “You do not believe it would be in his interest to be in court?”
“No, Your Honor. He’s blind. He’s not ambulatory, very thin and frail, and I think he can become very agitated.”
Other uncontested nonappearance stories are similar. One person is “of limited intelligence” with “limited understanding” of her situation. Another “did not have capacity to understand what was being proposed and did not participate in the conversation.” Another made only “mumbling sounds.” A patient resident at Metropolitan State Hospital indicated he was happy to stay in conservatorship and “very much did not want to come to court.”
Uncontested non-appearances checked. Miss Preston, a tall, thin black woman, straightened hair pulled back into a stubby ponytail, comes to sit next to Public Defender Susan Daley.
The psychiatrist at Alpine, where Miss Preston is a patient, takes the stand. His diagnosis: paranoid schizophrenia. The story, as it emerges, is that Miss Preston, 35, some six weeks ago presented herself at Alvarado Parkway Institute’s emergency room. She was, says the psychiatrist, “conversing with astronauts” and “felt that astronauts were in her head and gnawing away at her stomach, that she had worms in her and that there were snot rags lying all around the place.” She was emaciated, “simply not eating and taking any liquid at all. She felt food was poisoned and beverages were poisoned.” Although Miss Preston claimed she had been staying in a hotel room, hospital staff insisted she was homeless.
Because Miss Preston wishes to be returned to her family in Arkansas, Alpine staff has attempted to locate her relatives there. Says the psychiatrist, “Those people who know her refused to take her in.”
While Miss Preston mutters, “No, no,” he goes on. He believes Miss Preston has no insight into her condition, and, were she discharged, she would refuse medication. However, shortly after her admission to Alpine, she did begin eating — or as the psychiatrist described, “She became compliant with food and fluid intake very rapidly.” And “she has been participating in the program at Alpine with good attendance.”
Daley leads her client through questions designed to show lack of grave disability. Asked where she is residing. Miss Preston says, “I was staying back in Arkansas. First I chose California because of surgery that I have, and I have been trying to find someone to help me with my surgery that I have so I can get my job.”
Asked how she would get to Arkansas, Miss Preston says, “On the Greyhound bus.” And how much, she’s asked, would it cost to ride the bus home to Arkansas? “A hundred eighty-one dollars. Special is $68.” Daley asks about the astronauts. “Did the astronauts ever tell you to do anything wrong or bad?”
“No. They are not bad astronauts.”
“They are good astronauts?”
“Yes.”
Daley argues against establishment of conservatorship. Miss Preston was not homeless — “has, in fact, never been on the street, she stayed in a hotel and with friends.” Miss Preston’s weight has stabilized, she now denies feeling food is poisoned, she recognizes she must take her medication.
Although Daley pleads her client’s case passionately, it seems clear that Miss Preston will not be released. And indeed she’s not. “Delusion in and of itself would not be dispositive of the court’s decision,” says Judge Hammes, “but the fact is that when she came into the hospital she was emaciated. While she’s on medication she seems to be doing all right....
“My problem is, I feel that I would be turning out a child without assistance if I were to say she’s okay to go out on her own. We feel she does need service of a public conservator. All disabilities imposed except the right to vote. A closed, locked facility is the least restrictive facility.”
Miss Preston, tears running down her cheeks, bolts out the courtroom door.
Before the door closes, she looks across the courtroom and up toward the bench, mutters, “I feel tricked.” The psych tech who brought her to court is right behind her.
Mr. Guston — late 20s, longish I blond hair, blond mustache, wrinkled cotton sports shirt, jeans — walks stiffly to the defense table, sits next to public defender Barbara Gerrard. She explains that Mr. Guston will not be contesting conservatorship reestablishment but that he does wish to request a change of placement.
County counsel introduces the medical declaration for re-establishment of conservatorship, which indicates that Mr. Guston suffers from schizophrenia, paranoid type. A closed, locked treatment facility is the least restrictive placement recommended. Counsel calls Dr. Bernard F. Hansen, the only full-time staff psychiatrist at the County Mental Health forensic unit, to testify.
Dr. Hansen — mid-60s, garbed in tie, sweater vest, tweed jacket, slacks — had earlier interviewed Mr. Guston and declares that he suffers “from a schizophrenia of a paranoid type, chronic in nature,” that he remains gravely disabled, that he should continue in a locked, closed facility.
Dr. Hansen lifts his eyebrows, adds, “Which of course he objects to very much.”
From the defense table, Mr. Guston leans forward, pins Dr. Hansen in a fierce gaze. Mr. Guston’s jaw rapidly twitches, and his hands are fists.
Dr. Hansen continues, “I questioned him about statements in the memoranda [prepared for the forensics unit by the conservator], and he claims that he is not angry, not violent. He claims that staff ‘shanked him in the ass’ and set up some sort of electrical shock thing to use on him.
“He claims his doctor is, I think,” Dr. Hansen pauses, studies an open file folder, “a torturer and a sadist because he changed him from Haldol to Thorazine. As well, he accused staff of using cocaine at the hospital. He said they were using ether-based cocaine, and he claimed that he could smell the ether.
“In his examination of mental status, he did not perform at all well. Certainly he has no insight. He feels at the age of 20 he may have been mentally ill, but not now. Testing for retention, he can retain and recall properly only three digits forward and three back, and his memory is impaired. His abstract thinking is way off. He’s disoriented. I asked the date. He said he couldn’t give it, and I said, ‘Well, start with the year. That makes it a little easier.’ He knew it was 1991. He was not able to tell me which month this is.” Dr. Hansen again studies his folder. “And he does believe in telekinesis — that is, he thinks he can pick up paranoid ideas from others, and he tries to talk to them about these ideas and they walk the other way.
“He denies any delusions and hallucinations. [At the facility where he’s resident], I think the major problem has been behavior.... He’s a very angry person.”
Indeed, jaw twitching, eyes narrowed, Mr. Guston appears angry. The bailiff, from his desk some five feet away, keeps his gaze turned steadily toward him.
County counsel asks if Dr. Hansen had looked at Mr. Guston’s placement history in less restrictive facilities, such as board-and-care homes. Hansen has. These placements were not successful. He has been at his present facility for one year, but in the two previous years, he had been in nine different placements, spending 20 percent of that time in hospitals in acute settings.
Guston’s defender, Barbara Gerrard, questions Dr. Hansen. What evidence, she asks, did Dr. Hansen have of attacks on others that her client has made? Hansen admits he has no evidence. She then asks what problems Hansen would foresee were her client placed in an unlocked facility.
“I would certainly feel that what they described as outbursts in the reports and descriptions of being agitated and impulsive, I think these would be a problem.”
“What does ‘outbursts’ mean?”
“Outbursts? I guess, anger. They say that he should remain in a locked, closed facility until his outbursts diminish to a safe level. He is very angry, and I felt uncomfortable talking to him, although he did not express any anger at me”
Gerrard continues. She asks if Dr. Hansen has any evidence of his having been aggressively hostile to hospital staff.
He responds, “All I can say is what they said. ‘Aggressive outbursts, labile in mood, agitated.’ ”
Gerrard pushes. “I guess aggressive outbursts is a bit vague, and I wonder what he might do, what you have any evidence of his having done.”
Dr. Hansen, seeming peeved, answers, “I would say that this would probably put staff and other patients under considerable pressure, at least.”
Gerrard lets it drop. Her client is sworn. Gerrard addresses his desire for a new placement. He wishes to be put in an unlocked facility in San Bernardino.
Gerrard asks, “Why do you not want to live in San Diego?”
“It’s too closed in. I do not appreciate the city anymore. I need the countryside. That is why I asked to move up north.”
County counsel questions Mr. Guston, who admits that his conservator had offered him a placement in an El Cajon board-and-care facility, but he turned that down. “I do not wish to live in San Diego anymore. I have had nothing but trouble from the people. The city is not my lifestyle.”
County counsel asks, “When you have been in board-and-care settings in the past, the doctor’s information was that you were unable to get along and were asked to leave. Do you recall...”
Mr. Guston’s tone takes on ferocity, “Well, in one board-and-care I was thrown on the ground and almost broke my collarbone by a 210-pound black man, not to tell you he was black but that he weighed 210 pounds. He ran the board-and-care. He threatened that he would hit me, and I pulled my arm away from him because he had ahold of me. He slammed my arm in the dresser. I got stabbed in the chin in another board-and-care where I was attacked by a man who was sent to CMH and returned to the same board-and-care, and I was kicked out. He drew blood from my finger, slammed it in the chair and cut it open, and I had to have stitches.”
“Do you think that in any of these circumstances that your behaviors were part of the problem?”
“No,” says Mr. Guston, “l am very low-keyed. ’ ’
“Do you know you have been described as having angry outbursts?”
Belligerent now, he answers, “I tell the truth, nothing but the truth, so help me God.”
“What kind of truth-telling is it that people would describe as an angry outburst? What kind of situation?”
“I don’t lie for no reason, for no one.” “Can you tell us what kind of situation occurred that you felt you had to be honest about that got you in trouble?”
“I had an upset stomach. I was sick, and I asked for a 7-Up, and I was denied a 7-Up, and I told her that she was taking my privileges as an American away from me as well as my civil rights, and she told me I could not go to the canteen furthermore, so I cursed at her, and she took my walk pass away, my other civil right. Now I don’t have a walk pass that everyone else does have....”
“So you did better for a while, then you had these setbacks?”
“No, I have done well all the way.”
Mr. Guston goes on to say that he participates in his group, that he showers and shaves daily.
After more questions from county counsel. Judge Hammes rules. “Based upon the evidence that I have heard, I believe the present closed, locked facility is the most appropriate.”
The judge pauses, gazing down at Mr. Guston, studying him. “As I can see, you are very angry, and it was evident even when you were getting sworn in by the clerk.”
Mr. Guston leans forward, jaw working faster, “You look with your eyes. It’s not with your spirit.”
Frown lines crease Judge Hammes’s forehead. She says, “Well, you looked very, very angry at the clerk, even when she was swearing you in, and I think you might scare people...”
Mr Guston’s mouth is tightly set, his jaw works furiously. When he speaks, he seems ready to spit. “The truth,” he says, standing up from his chair, ‘ ‘is very scary, I must admit, as one telling the truth.”
The bailiff rises, moves toward Mr. Guston, says, “That will be all, sir.
You can go.” Mr. Guston turns his eyes to the bailiff, seems ready to strike him, then pivots, strides out the courtroom door.
This morning, the matter of Dario Gonzalez, a rangy 15-year-old in red T-shirt and jeans, is also heard. Dario was named a ward of the court at the age of four. He has been in the mental health system since he was nine because of uncontrollable violent behavior. For the past two years, he has lived in the state mental hospital at Cabrillo, in a unit set aside for minors. He has asked to be returned to his home in San Diego, to live with his father, brother, and sister. He pleads with particular urgency to be allowed to leave the hospital and to go home. He notes that on his visits home there has been no trouble, he has done as he’s been told, has created no disturbances. Judge Hammes listens carefully, then asks that his case be carried over to give her time to talk with Dario’s family and doctors.
The young woman — Miss Anders — who had sniffed at her armpits continued to do so until she went to sit next to the public defender assigned her case. Questioning reveals that she has recently made another in a series of suicide attempts, that this was not her first hospitalization. Twenty-eight now, she has never held a job and, except for periods of hospitalization, has lived with her parents. Although anti-psychotic medications relieve her more severe symptoms and quiet the voices she hears, she remains depressed and anxious. She often “cheeks her meds” to avoid taking them, and when she goes off medication, she “cuts herself to the bone” on arms and legs. She wishes to be returned to her parents’ home, but they refuse to take her back; they want her placed under conservatorship and to remain hospitalized.
Called to testify. Miss Anders speaks in a tiny, clear voice. She promises, if returned home, she will take her medication, she will see her doctor. After further questioning, during which Miss Anders begins to ramble, Judge Hammes rules that she be placed in conservatorship, with a closed, locked facility as the least restrictive setting.
And there is the woman in her late 30s who wears the bulky muumuu and girlish bow — Miss Tarrington. She sits next to her defender, she hunches her shoulders, huddles in on herself as against some internal chill. County counsel asks the psychiatrist from the hospital in which the woman is resident, “Is it correct that at the time of her admittance there was some concern about her wandering in traffic and that she was saying she was on a journey?” “Yes,” he answers, his voice as matter-of-fact as if he were discussing an oil change for his car. “Originally when she came in, she was markedly disheveled, wandering the streets. When the police picked her up, she said she was Jesus going to Jerusalem.” Miss Tarrington is placed under conservatorship, with level of placement a closed, locked facility. “Good luck to you, Miss Tarrington,” the judge says.
It is almost noon. The spectator seats are empty. Judge Hammes turns to county counsel, asks, “Is that it?”
County counsel nods, says, “That does it.”
Jeff Elias stands from the defense table, begins gathering up the pale blue case files, smiles, says, “That’s a wrap.”
I went to see Jeff Elias, the public defender’s mental health team leader, at his llth-floor office in the City Centre building. His desk was stacked with the pale blue files that held patients’ records, with legal books. DSM-III-R, the Diagnostic and Statistical Manual of Mental Disorders, lay on one corner of his desk, and on the top shelf of a bookcase was a photograph of Elias’s son and daughter. It was early afternoon, and warm. Elias had tossed his jacket on a chair, loosened his tie.
He said he had come to this office three years ago, after serving as a public defender in L.A. for 11 years. “It’s something you have to like. Nobody does this kind of law unless they want to do it. It’s very specialized. It requires a strong advocate but a person who can be compassionate yet not so sensitive as to be crushed by what you hear day in and day out.
“Most of our clients are appreciative, as opposed to many criminal clients. We get cards and calls. Many of our clients need friends, and very often we are the only people they come into contact with who aren’t giving them a hard time. So you find yourself spending time with clients who just want to talk and talk.
“What makes it easier is we are not the treating doctors, not social workers, we are not there to try to dislodge a delusion, we are there to be an advocate for their legal rights, to counsel them to the extent they are willing to be counseled.”
I noted that many of his group’s clients will at first sound rational and then begin to speak near-gibberish. He agreed. “You will hear a person talk for a few minutes and they’ll sound fine, but as they talk longer, you will discover they are delusional, their thinking is not orderly.
“Usually, people who first enter into the hospital exhibit more acute symptoms than what you see once they are ready for a conservatorship hearing. If you went onto an emergency unit, you would see things you won’t see in court. Most people you see in court have been medicated.”
The medication, Elias said, often causes stiffness, shaking, dry mouth, restlessness.
“Many people will have trouble talking because of the medications. They know what they want to say, but they can’t say it. You have to get judges accustomed to these side effects of medication.”
I had heard that at the moment there were three conservatees with jury trials on calendar. Were there many jury trials? “No. We don’t get many. In part, most people don’t seem to be litigious enough to follow through or to fight what’s happening. Some can’t and others are intimidated by the system even though it is fairly informal. We try to comfort people, assure them there’s nothing to be fearftil of. But it’s embarrassing for many people. Imagine, coming to court and having people testify as to all these bizarre things about you. Most clients really don’t put up the fight to which they’re legally entitled.”
I’d seen psychiatrists and psychologists become testy under questioning by Elias’s team. One psychiatrist had told me that he felt Elias got some people off conservatorship who should have remained.
Responded Elias, “A lot of times doctors will accuse us of rabble-rousing among the patients, persuading them to fight and contest. But that’s far from what we do. There is some resistance on the part of many of the medical profession against our giving legal advice. They view LPS as interfering with their treatment. They resent having to justify this, to document that. There are some doctors who are even hostile to us.”
Because conservatorships must be reestablished annually, Elias and his staff see everyone on conservatorship at least once each year. Elias added, “Many of them we see more often than that. Many of them you receive calls from weekly, sometimes almost daily.” He went on to explain that he and his team spent afternoons visiting clients in local hospitals and in the board-and-care facilities. I asked about the latter facilities.
“There are hundreds of these. These are homes, licensed perhaps to house six people. Some are geared to geriatric patients, others to a younger clientele. The people are provided food, medications are dispensed. Staff isn’t necessarily trained to provide medical or psychiatric assistance, but staff members are there to notice if people are taking medications or if they are beginning to deteriorate in their conduct. If that happens, they can contact a conservator or doctor or they can take a person to a hospital.
“You will have people in board-and-care who go to day treatment programs. It fills their day. These programs, ideally, are providing lessons of insight, how to deal with mental illness, understand medication, develop living skills that can be applied to independent living. But the complaint we hear from our clients is that many of these programs are just busy work. Some people are happy with that and some aren’t.
“But it is a hard existence. There is not much to do around the board-and-care during the day. Some want you out after breakfast and not back before dinnertime. You don’t have much money. Most of the money you receive goes toward rent. If you smoke, what extra money you have to do anything is extremely limited. Most people get around $700; most board-and-care facilities get $500 or a little more. There’s no money to waste. It’s a real tight budget. A great deal of monotony is associated with that.”
Had Elias ever seen a case in which he believed a person who was not severely mentally ill was railroaded?
“No. I cannot even think of one case where we thought that or observed that. There are enough checks and balances in the system to keep that from happening.
“There are sick people who are cut loose much more readily in the system than are probably kept. You can honestly and accurately say that there are few people now who have been scooped up by the system who probably don’t deserve to be. Certain ones beat the system, get off conservatorships, and we never hear from them again. But many more come back into the system.”
The hope, he said, with LPS conservatorships was that the mentally ill would be taken from mental hospitals and brought back to the community and put into a setting where they could live a more normal life. “What happened was, yes, the liberties .and protections did, in fact, occur. The unfortunate thing is the community programs that were to be put in place never, in fact, were. It never got done in the community right; if it had been, there would be many people out there doing better than they are now.”
Almost every Tuesday and Thursday morning for four weeks, at about 8:30, I made my way through downtown streets, headed for the courthouse to attend conservatorship hearings. Always, before I arrived at the courthouse’s entrance on Broadway, I would pass men and women clothed in layers of garments, waking up from the broken-down cardboard boxes and ragged blankets on which they slept. Often they were deep in monologue, lips moving rapidly, hands fretting with dirty sleeves and rubbing dirt farther into creases of deeply tanned skin.
On Union Street, between Broadway and B Street, I would sometimes be greeted by a tall, spindly black male who pushed a shopping cart. Inevitably, he was wearing a woman’s blond wig set askew on his head, several dresses, a skirt. His feet would be pushed into women’s high-heeled shoes, from which several inches of his own bare brown heels protruded. He would lurch toward me, pushing his cart before him like a battering ram and demand that I give him money for breakfast.
Farther down the block, there’s a bus bench at Union and B streets, protected from weather by a second-story corridor that runs from courthouse to jail. Some mornings a middle-aged woman, tousle-haired, with large, sentimental eyes that she rubbed with knotted fists as if she were recently awakened from sleep, would be sitting on that bench, her filthy dress hiked well above her knees. She would be raving to herself in a staccato demi-English. As one after another person passed by her, she would halt her rant and ask for money.
Once inside the courthouse, waiting in the hall by the door into Department 14’s courtroom and then observing what went on in that courtroom on Tuesday and Thursday mornings, it was impossible not to see and hear likenesses between many people living on the streets and people appearing in mental health court.
Late one morning, a man in his early 20s had been brought from a hospital to the courthouse because he had requested a writ hearing to protest his hospitalization and demand his release. Four male attendants accompanied him. He was seated on one of the wooden benches in the hallway, an attendant on either side of him, two standing in front of him. He was slight in build, young, surely not more than 22, cleanly and even elegantly dressed in silky black turtleneck and beige trousers; he was dark-haired and handsome. Every few seconds he would lunge forward, teeth bared, and bite at his attendants. They would grab at him, hold him down. He would buck, growl, lunge. People walking by moved quickly and looked away.
I began to feel how difficult it is for those of us who have little contact with the mentally ill not to feel uneasy in their midst. Our own stability often feels so tenuous. Several mornings when I went to court, I’d not slept well, I was tired; the air was hot and muggy, and the streets around the courthouse seemed an obstacle course of need and craziness. I would begin to feel ill myself, shaky and strained. I’d feel my own often fragile psyche, my dubious hold on things, threatened simply by the presence around me of what felt to be an abnormal subjectivity or so many and such varied aberrant subjectivities.
And on those mornings, when I felt weary and plagued by a certain dis-ease, what seemed my usual point of view took on an odd slant, a queer bias. Then, the obviously mad people living on the streets and men and women babbling on benches outside Department 14 would feel to me to be carriers, not of physical illness, but of some virus that broke down the psyche’s linkages to a here-and-now in which two plus two always equaled four.
Tuesday and Thursday mornings, psychiatrists milled about in the hall, waiting to testily as to why patients incarcerated in their facilities should or should not be released. Most dressed conservatively, in well-tailored suits. There was one man, bear-like and gray-bearded, who eschewed suits and wore rumpled wash pants and sport shirts. He had been pointed out to me as a psychiatrist. His name, I was told, was Yaroslav Kushnir.
One morning, in the hall, I approached Dr. Kushnir. He spoke an accented English. He said that his practice was made up principally of acute and chronic patients, many of whom were on conservatorship. I asked if he thought the LPS conservatorship system was better than the old civil committal system. He said, about the LPS system, “It’s like communism. It works great on paper.”
I said it would seem that horrible things must have happened to some of these people when they were children. Kushnir nodded. “Some of them do have terrible histories, that’s true. But that’s not enough. Chronic schizophrenics, they often come from good homes. Schizophrenia,” he said gruffly, “it’s like a cancer of the mind, once you get it... ” And then his beeper went off, and he excused himself.
The morning on which Mr. Wang, Mr. Guston, Miss Preston, Miss Anders were in court was certainly a very average morning of conservancy hearings. As I sat through many more mornings of these hearings, I became increasingly impressed by how so many of these men and women, diagnosed as suffering mental disorder, courageously managed to keep themselves going. And I came quickly to understand a comment by Judge Hammes. So many cases she hears, she said, left her feeling emotionally drained.
There was the woman in her mid-30s, carefully dressed, blonde, her brightly rouged face oddly ageless, who had been a conservatee for ten years. She was in court because she wished to be taken off conservatorship. According to the report submitted by county counsel, she was kept on conservatorship because, from time to time, she ceased taking her medication and had to be hospitalized. But she was able to live independently in a studio in one of the downtown hotels and explained, proudly, that her studio had a refrigerator, a microwave, a television set. Her rent, she said, was $312 per month.
The public defender asked the series of questions designed to show that her client was not so gravely disabled as to be unable to care for food, clothing, and shelter. She asked, “Who pays the rent?”
“I pay it.”
“Do you get a check every month?”
“Yes.”
“And how much is that check?”
“Seven hundred and twelve dollars.”
“And out of that you have to pay your rent and handle all your other affairs?”
“Yes.”
“How do you handle your budgeting?”
“I budget until I have so much money for food, and I don’t overspend on anything.
And by the way, last month I saved $300.” All at once, the woman sped up, saying, “And I am not hungry and I am not starving and I have clean clothes and I have a nice clean room and by the way,” she stopped, looked about the courtroom, smiled, “I am really a sweet girl.”
I thought, at that juncture, “What a terrible moment for an attorney,” as the public defender continued, asking, “You were hospitalized in December of last year. Did you take yourself to the hospital for medication?”
“Yes.”
“You were suffering from depression?” But it was all over. The woman had begun what psychiatrists describe as decompensation. She had made the leap from the here-and-now into delusion. “Over my children. That was caused because I had a daughter. I was having trouble with the baby in my body, in other words, I was pregnant.” She added, with great innocence, “I can explain how it happened.” And then she went on to say, “I plan about three years more in this county because I want to get a degree. I am in college right now. I am studying international relations, dance, and chemical dependency.”
Many mornings in conservatorship, I would see and hear that decompensation. There was the woman in her early 40s, diagnosed as schizophrenic, who had been brought, completely naked, by the police into Harborview’s emergency room, where, according to Harborview staff, she behaved violently. Previously, she had been in the state hospital at Camarillo and currently was in a closed, locked ward of a local hospital.
She wept, telling the judge her husband had left her, then, when she became ill, she lost custody of her children. She said she had been in and out of hospitals but had continued to be able to visit with her children on holidays and in the summer. Her children were scheduled to visit her soon. She begged the judge not to institute the conservatorship. She said, “I have always conducted myself as a lady. I have always slept alone.” And then apologizing for being “so emotional,” she sobbed, “I am forced to take medicine not made for me.” Then she pulled at her aqua blouse, which barely buttoned across her broad bosom, said, “and these are state clothes.”
A stocky man with close-cropped hair standing stiffly across his broad skull had been brought from Patton State Hospital for a re-establishment hearing. The psychologist whom I sat next to that morning told me that this man had suffered brain damage from sniffing glue. The man’s head twitched frequently, and his dark eyes, when he turned them toward us, looked as if acetylene sparks could shoot from them. An odd smile regularly fluttered over his lips. “He’s hallucinating,” the psychologist told me, “hearing voices.” Questioned by county counsel, the man spoke not one understandable word but seemed rather to detonate a series of husky gutturals, dream cries, gleeful bursts, murmurs. Judge Hammes ruled that his conservatorship be re-established, with the state hospital to remain as the least restrictive setting.
Conservatorship hearings in which family members address the court can be particularly heartbreaking. Miss Adams, a stylishly dressed, heavyset woman in her 30s, sat in the second row, next to a woman whose 20 additional years and similar features made it obvious she was Miss Adams’s mother. When Miss Adams’s case was called, she went to sit next to Steve Binder. Miss Adams had several months earlier attempted suicide. It was not her first attempt. She had recently been transferred from the hospital to which she was taken after her suicide attempt to a second hospital, where she was being held on an open ward. She was asking the court that she not be placed under conservatorship and be permitted to live with her mother.
Miss Adams listened intently as the psychiatrist from the hospital to which she was first admitted testified as to her condition. She was diagnosed as suffering a major and recurring depression. “During her entire hospitalization with us, which was approximately 55 days, she expressed almost daily that she was feeling suicidal, feeling very hopeless and helpless. Frequently she mentioned that, if she had the opportunity, she would kill herself.”
Miss Adams was sworn. In a strong voice, she said, “I am not gravely disabled. I can take care of myself as I have in the past. I just need to get myself together. I lost my twins, and I just lost it.”
Judge Hammes leaned forward on the bench, asked, “When did you lose your twins?”
“At about five months. And after that was when I came to the hospital. I brought myself to the hospital this last time, so I am able to seek help. I do take my medication, I do believe I should take it.” Miss Adams, with Judge Hammes’s prompting, went on to explain that six months ago, when five months into a pregnancy in which she was carrying twins, she miscarried. The twins were born dead. It was after that she made her suicide attempts. She hoped now, she said, to return to her job as an aide in a nursing home and to live with her mother until she got herself together.
Miss Adams’s testimony completed, Judge Hammes said, “I think her mother would like to speak; I have a little note from the bailiff.” Mrs. Adams walked to the witness stand and was sworn.
Mrs. Adams stated that she was not willing at this time for her daughter — Dorothy — to live with her. “I really don’t think Dorothy is as well as she thinks she is. It hurts me to say that. She is safe at the hospital. There is not anything there to put stress in her life. She knows her job is destructive. She works at a convalescent home, and in that job she sees death and dying, depression. It depresses her.
“She is more than welcome at my home but not if it is simply going to be a turnaround and in three weeks she is depressed and at the point of death again. If you let her go now, she is going to be where she was three weeks ago. She wants out. But I want her healthy, and she is not going to be healthy if she comes home now. She is not over all that she has gone through. And as I sat here I knew I had to say something. I know to her it is a horrible thing, but I know it is the only thing I can say.”
Judge Hammes asked, “Is it hard to testify in this way?”
“No, because it’s something that I feel it’s right. I am worried for her safety. I am worried for her life from now on, not only her safety for three months, but for the rest of her life.”
Judge Hammes ruled that Miss Adams remain in a conservatorship in her present facility. Outside in the hallway, the mother and daughter came face to face. The psych tech accompanying the daughter moved aside to let them say their good-byes. The daughter sobbed. Tears rolled down her cheeks. The mother stood dry-eyed, arms at her sides. She opened her mouth as if to speak, then said nothing, turned and headed toward the elevator.
Mr. O’Toole, a broad-shouldered six-footer in his late 30s, looking uncannily like Burt Lancaster in his title role in Elmer Gantry, wore a navy-blue suit, pale-blue shirt, rep tie, Cuban-heeled black boots. He strode with great bustling confidence from his seat among spectators and took his place next to Steve Binder, the public defender representing him. Mr. O’Toole seemed more like a successful political candidate about to receive the homage of a grateful party than a petitioner come to court to plead for disestablishment of a mental health conservatorship. Psychologist Gregg Michel, who had interviewed Mr. O’Toole earlier that morning, was sworn.
Questioned by county counsel, Michel noted that Mr. O’Toole “suffers from what we used to call manic depression, now labeled as ‘bipolar disorder.’ ” Mr. O’Toole, Michel went on to say, had been diagnosed as “manic with psychotic features.”
“At this time, in your opinion,” county counsel asked, “does he continue to be gravely disabled?”
“Yes, in my opinion, he is gravely disabled. During the first 30 minutes that I spent with the patient today, he had some passive signs of his illness. He became pretty agitated. He was fairly intact, except for orientation. He believed that the year was 1981.”
Mr. O’Toole, starting to rise from his chair, shouted out, “I didn’t say that. I knew that it is 1991.”
Michel ignored the outburst, continued. “After approximately 20 to 30 minutes into the interview, he began having more and more difficulty focusing and had to be refocused constantly and became very concerned about the outcome of the exam to the point that it was difficult to conduct it. He has trouble with his attention, concentration. [At the hospital where he lives] he is a management problem. He wishes to sleep in. He looks better than he is. He is not accepting treatment. He doesn’t like it.
“In the summer of 1990, when he arrived in San Diego, he was extremely decompensated, disheveled, and quite psychotic and required acute hospitalization. He can seem to behave very appropriately, but the psychotic process does come out with this patient to a great degree.
“He shows a lack of insight. He was not aware of budgetary need. I could not get him to give me a rational plan as to how he would care for himself, except to say that he might live in cheap hotels, use his SSI, and whatever money he had left over, for food. And then he started talking about how he would enjoy eating in very nice, very expensive restaurants like Tony Roma’s.”
Mr. O’Toole stood to be sworn. When he raised his right hand, his suit jacket lifted, revealing that his black belt had not been threaded through the belt loops at the back of his trousers.
County counsel asked, “What do you suffer from?”
“Bipolar. But it really is not so much a matter of suffering, is it? It is this matter of always being treated.”
County counsel asked how Mr. O’Toole came to be hospitalized. He explained he had come to San Diego seeking work, run out of money, lived on the street, was picked up by police and taken to Harborview. “At Harborview, they asked me, did I want a conservatorship? And I said, ‘Why not, I’ve never tried one.’ ”
He went on to say that he was taking Prolixin, lithium, and “a little blue pill.”
He added, “I feel totally compliant about medication.” He assured the court he felt far more in control than in November. “I feel able to be a total member of society. I have bought clothes. I am able to dress nicely, I go to high-class singles’ events. At the place where I am staying, I have made friends. The ambience there,” he fluttered his hand in the air, shrugged, “is not that unbearable.”
County counsel asked where Mr. O’Toole would live were he permitted to leave the hospital.
“I have a degree in hotel management. I know the whole motel and hotel scene like the back of my hand. All this talk about shelter, I ask you,” Mr. O’Toole seemed exhilarated, “how many places can one person stay? Food and shelter in the past has not been for me a problem. By September of last year, because I had been living on the street, I had simply become unkempt. This,” Mr. O’Toole gestured contemptuously toward county counsel, toward Michel, “is just a little song and dance I do when I run out of money.” Binder pleaded, “Mr. O’Toole, however awkward, is able to use community resources. Whether for shelter or the need for a restaurant. He was able to get clothing and food for himself, able to commit himself.”
But it was no go for Mr. O’Toole. Judge Hammes, noting that Mr. O’Toole “does make a rather good presentation,” went on to refuse to end his conservatorship. Her refusal appeared to do little to thwart Mr. O’Toole’s elation. Psych tech right on his Cuban heels, Mr. O’Toole left the courtroom as would someone who had just received a standing ovation.
Outside Department 14, Mr. Jernigan had towered over the psych tech who accompanied him to his re-establishment hearing.
Mr. Jernigan was in his mid-50s, dangerously thin, and his skin had a blue pallor, the bloodless cast that skin will take on when someone sits in a darkened room watching a television on whose screen some black-and-white movie is showing. He moved restlessly up and down a small patch in the hall and pulled at the sleeves of his hooded sweatshirt. Once in the courtroom, seated next to his attorney, Patricia Rosenberg, Mr. Jernigan put his head down on the table while Dr. Kushnir testified.
“He has come up to staff with his fists and threatened to hit them. They believe he would have struck them if they hadn’t taken action. This is one of a dozen overall admissions for him. He is having a hard time. He was living at an intermediate nursing facility. I believe they are maintaining very well for him. But about a week before his hospitalization, he began to skip on his medicines with the result that his psychosis became aggravated, and he was running down the corridors of the nursing home, bumping into elderly patients, demanding cigarettes, going into other people’s rooms saying he was King Henry and everybody was his subject. He wasn’t sleeping and was very disruptive.” What Mr. Jernigan wanted. Dr. Kushnir said, was to be let out of a locked facility and allowed to live with his brother in North County. Dr. Kushnir said he could recommend only a closed, locked facility for this patient.
His long, scarecrow-thin arm stuck in the air, Mr. Jernigan was sworn. Asked then by Rosenberg about his medication,
Mr. Jernigan groaned, “Oooooh, it’s bad. God, it’s bad. Makes me sleep all the time.”
“But does it also help you?” Rosenberg asked, and Mr. Jernigan lifted his head, grinned idiotically, and nodded in the affirmative. Rosenberg went on, “Did you hear the doctor testify that the staff was frightened sometimes of you?”
Mr. Jernigan said he knew, then added, “They took away my clothes and my wallet.”
“So that made you mad.”
“They took away my social security card.” Mr. Jernigan’s face shifted through expressions from rapture to grief. He began, then, to weep — a moist, noisy sobbing. “My brother has died.” He moaned, then, without any apparent segue, brightened and began to explain that his name was Charles Jacob Tudor, that he was now and had been, he shouted, “the KING OF ENGLAND.” As swiftly as he had brightened, Mr. Jernigan dropped back into weeping. He looked toward the bench, tears streaming, said, “I love you, Judge.”
Judge Hammes, appearing momentarily disconcerted, said to the court reporter,
“Let the record show that Mr. Jernigan alternates between crying and laughter.” Rosenberg plunged on, asked Mr. Jernigan, “Did you hit anybody?” “No.”
“Even though you got mad, you didn’t actually hit anybody?”
“Oh, no.”
“Mr. Jernigan, if you were released from the hospital, where do you want to stay?”
“I want to stay with my brother. In Del Mar. It is so pretty in Del Mar.”
“Do you have social security and SSI?” Rosenberg asked.
Mr. Jernigan muttered a yes. Rosenberg asked, “Do you have someone to manage your money for you?”
Mr. Jernigan laughed happily, burbled, “My brother, my brother.”
Noting that she didn’t often have the king of England in her courtroom. Judge Hammes ordered that Mr. Jernigan’s conservatorship remain in place, with the least restrictive placement to be a closed, locked facility.
Jeff Elias had told me that he and his fellow public defenders had puzzled for months over a question Dr. Hansen put to interview subjects in his mental-status examinations. “How,” he asked, “is an apple like a horse?”
Watching and listening to Dr. Hansen testify in court, at first I’d not much liked him. He seemed, somehow, very stuffy. Then one morning, during questioning about a patient with a history of alcoholism, Dr. Hansen was asked by county counsel if he believed that in the locked facility in which the patient in question was resident, she had been, as reported, consuming “one or two beers a day.” Judge Hammes suddenly leaned forward on the bench, asking Dr. Hansen about the facility, “They don’t provide beer, do they?” And Hansen, smiling wanly, had shot back, “They don’t do that. They are not like the French.” I began, after that, to reassess my opinion.
The offices of the San Diego County Mental Health Service’s forensic unit are packed into a first-floor wing of the county courthouse, with large windows overlooking Union Street. I went one afternoon to Hansen’s office to chat. His office is nothing more than a small cubicle into which are crowded a small bookcase, file cabinet, and three chairs.
He told me that he came to the forensic unit 12 years ago and is the only psychiatrist who works full-time there. In addition to evaluations for re-establishment of conservatorship, he evaluates accused felons. His favorites, he smiled, were “the great malingerers,” accused criminals who pretended to have been insane at the time they committed a crime or who affected being too insane to assist in their defense.
Testifying, Dr. Hansen always noted that he had talked for 45 minutes to an hour to a conservatee before he made his evaluation of that person’s present condition. Before the interview, he will have studied a report prepared by the Department of Social Services’ conservators’ unit, a report that will include information from the conservatee’s residence and treating physician as to progress or lack of same. There will be a medical and psychiatric history. Perhaps educational, work, and family history.
“Most people we see are troubled — depressed, anxious, irritated, confused. That’s what we deal with most of the time. In many cases, their memories aren’t too good; patients don’t always remember their own histories or they don’t want to tell you sometimes.
“A lot of these people never functioned too well before they became ill. It may not have been too obvious. I talked to the family of a young woman on whom I was taking a history. They said, ‘She was doing fine, then suddenly one day she started screaming and walking down the street and taking off her clothes.’ But talking further with them I learned that several years before this incident the young woman had sat in her room for a week and wouldn’t come out and wouldn’t talk to anybody.
Then she passed through that and seemed okay. But then several years down the line, she had this real obvious break that they couldn’t ignore.”
I had heard, I said, many conservatees described as bipolars, manic-depressive.
Dr. Hansen agreed. “A lot of depressives go through that courtroom. One of the most common things, and the tendency seems to increase with age, many of the affective disorders get worse as you get older. And a lot of bipolars, as they get older, get the episodes more frequently and they last longer.
“The manics are interesting. When you deal with a manic, if, in your diagnosis, you rely on him for your history, you should be charged with malpractice. Because with a manic, they feel good!” Hansen clapped his hands, smiled, and then suddenly looked dour, “Unless they are getting into trouble — perhaps swimming in the nude in a public pool.”
I asked Dr. Hansen about a test I’d heard him mention in court. He had asked a patient to name 24 wild and domestic animals in one minute. I had tried this, had asked friends to do it. The best that I or anyone I knew could do was to name 18 animals in one minute. “You’re okay,” Hansen said. “The range is 12 to 24.”
He went on to mention a case on which I’d heard him testify — Mr. Moody. “He told me he just blanked out or spaced out when he tried to do this. He got six, and then he spaced out. It’s a test of memory. First you have to remember it, then you have to retrieve it, and then you have to be able to express it. And some of these people can’t retrieve worth a damn.”
Hansen looked thoughtful. “Some people may be preoccupied with a lot of internal stimuli I can’t see. Sometimes you can’t observe the stimuli. But you can see they won’t be listening to you, they are listening to something,” Dr. Hansen pointed to his head, on which, from the windows, afternoon sunlight fell on the wispy grey hairs and produced a halo effect, “that is coming from up there.”
How did he ask people if they were hearing voices?
“I don’t ask them about voices or hallucinations. That’s one of the last things you ask. You start off by asking about racing of thoughts. There are some people who go through a period of time when their thoughts are racing rapidly through their mind, they can’t keep up, they stop, they go slowly, but their thoughts seem to speed up, keep changing speed. The person can’t keep up, so he gets confused. His thoughts just seem to be doing their own thing.
“The second thing I usually ask is, ‘Have your thoughts ever been so strong you could hear them?’ Then I ask, ‘Have your thoughts ever been so strong that they sound like someone standing near you reading your thoughts aloud or speaking your thoughts?’
“Then I would go to things like thought insertion."
"Thought insertion?
“Yes, thoughts you don’t like, thoughts that feel as if they are not your own. I might ask, ‘Do you feel that these thoughts are being put into your mind from the outside?’
“Or there’s thought extraction. A person may lose his train of thought and start thinking that a thought has been pulled from him from outside. Then you can go on to other things like thought broadcasting. I would ask, ‘Do you believe that your thoughts are broadcast, that people around you, when you walk down the street, are thinking the same thing you are?’ Or, ‘Do you think that you can broadcast your thoughts?’
“Or I might ask, ‘Do thoughts escape from your head, go out in the air? Do you believe people blocks and miles away can pick up those thoughts and know what you are thinking about?’ These are pretty standard things.
“A lot of them will say they don’t hear voices, so I kind of beat around the bush. Then try to zero in.”
I reminded Dr. Hansen of a conservatee whom he had evaluated who told Judge Hammes that he believed voices ascended from the radiators in the dining room in the hospital where he was resident, and therefore he was afraid to go into the dining room. On several occasions, this man had rammed his head into the radiators. What was this about?
“People frequently have a source they believe these voices are coming from. Which is why some people will smash their head on, for instance, the radiators, because they believe the voices come from there.
“I may ask in such a case, ‘Who do you think is doing it? Why?’ They often will tell you that an individual is doing it or a group. If they are paranoid, they may tell you the CIA is doing something to them. Or they tell me it’s electronics.”
Have delusions changed over time?
“The ‘who’ and the method, yes. They do keep up to date. They don’t lag too far behind. In the old days they talked about telegraphs. Today they talk about electronics. They say they are controlled electronically. Or by computers. You will be told, ‘I have a computer in my head, put in there by the CIA.’ ” Hansen laughed, “The KGB is out of business. They do pick up the fears and suspicions of the time that are abroad in the culture.”
I had heard only one person in court claim to be royalty. Did Dr. Hansen hear this claim as often as he did, say, 10 years ago? Or 20? He thought not. People don’t know as much history, he said. “But a lot of these people, they are somebody or they are about to become somebody.”
And people believing they are Jesus?
“I guess he’s the most important fellow in our Christian background, and of course, he’s the Son of God. I think this is a symbol of power and protection. ‘No one can hurt me. I’m such-and-such.’ You look at each one of these persons and try to run it down why they say such a thing. As they get better, they realize it ain’t so.”
One of the rights given to conservatees is the right to make determinations about medical treatment apart from treatment for their mental disorder. What did Hansen ask to establish a person’s ability to make these decisions?
“I usually come up with some symptoms. Say, ‘You got up, you went to the bathroom, you were passing water, you saw some blood in your urine, what would you do?’ If their answer is ‘I don’t know what I would do’ or ‘I would go back to bed,’ such answers would go against them. I also ask about symptoms of botulism, which is a very serious illness — blurred vision, double vision, can’t swallow, paralysis of the nerves. If they don’t say, ‘I would go to the doctor,’ I would say they are not very competent.”
What is it, I asked, this taking off of clothes and going naked down streets that I heard about several times in court?
“Some street drugs like PCP make people very warm. People get a lot of odd somatic symptoms. They seem to seize upon them. They may feel warm, they may feel flushed, they may get overactive, and they’re sweating,” Dr. Hansen smiled, made motions as if he were tearing off his shirt, “and off go the clothes!”
I asked about the number of people I had heard described as scratching themselves, cutting themselves.
“Some of these people have what is called anhedonia. It comes from an old Greek word, anhedonic. These people will take things to give them some feeling, to get sensation. You get some of these people under distress, they may cut on themselves. Some people will say, ‘It felt good, so I did it.’
“So-called borderline personalities, one of the common things they do is cut themselves.” Hansen paused, thinking.
“Very labile, the borderlines. They overvalue you one day and decimate you the next day. Very angry sometimes. They have a hard time getting along in life. A Spanish psychiatrist called the borderline personality disorder ‘the ugly personality.’ Very descriptive, but we wouldn’t dare use it.”
How many people he sees on conservatorship have been drug users?
“It’s hard to guess. And they don’t always tell you. But drugs play a big part. I can remember when in a state hospital, if you saw a drug addict, the person was usually a heroin user. Some sniffed cocaine. Most of the time, people using cocaine didn’t get into too much difficulty. It was quite expensive.” He laughed. “Tallulah Bankhead said, ‘Cocaine addictive? Hell, no; I’ve used it thousands of times myself.’
“A lot of people now who use, use several drugs — speed to get high, barbiturates or heroin to calm down. You keep bouncing around. These are real problems.”
Hallucinogens, he added, are “considered to be bad for schizophrenics. Some people think it may predispose them to cracking up. Many of our schizophrenics are pretty precariously balanced, and it may not take too much to turn them over.”
I asked Dr. Hansen if he thought the LPS conservatorship was an improvement over the pre-1968 civil commitments.
“There were criticisms of the commitment process. Among them, mainly, some felt that the hearings were very short.
I worked at Agnews State Hospital near San Jose, and it wasn’t as the opponents said, but they often did have very short hearings. At Agnews, they used to have a court at the hospital, and the judge would be there. It was efficient. A lot of the attorneys would often handle cases on the morning we went to court and often wouldn’t know very much about the cases or spend much time with the patients. Now you have a group of public defenders whose reputation and livelihood depend on what they’re doing, which makes our work a little harder.” Dr. Hansen paused, pursed his lips, said, “Probably it’s more just.”
No conservatorship hearings' were without drama. But one morning was particularly epic. Judge Hammes, earlier in the month, had ordered that the Dario Gonzalez matter, in which 15-year-old Dario had asked to be allowed to leave Camarillo State Hospital and return home, be carried over until she had time to talk with Dario’s family and doctors. Today she was to announce her decision. Public Defender Patricia Rosenberg, Dario’s attorney, stood in the hall chatting with Dario, Dario’s father and younger brother.
Jeff Elias was there, blue case folders stacked in his arms. I told him I’d been to see Dr. Hansen and had asked the answer to “How is an apple like a horse?” Elias looked so hopeful that I hesitated before I said, apologetically, “They are both living things.” Elias groaned.
During the mornings I’d attended conservatorship hearings. I’d struck an acquaintance with a court-watcher. He directed my attention to a particularly chic and terribly thin woman in her mid-40s — Mrs. Raines. He said he knew this case and that checking the calendar posted next to Department 14’s door, he noted that Mrs. Raines had been brought from a hospital to court for a hearing on establishment of conservatorship.
Mrs. Raines sat on a bench outside Department 14, talking with a handsome, well-barbered, conservatively tailored man who appeared several years her junior. He was, my informant said, her husband. On Mrs. Raines’s other side sat her privately retained attorney. A young woman, whose small mouth, large blue eyes, and taffy-colored hair suggested she was Mrs. Raines’s daughter, stepped off the elevator and walked slowly toward Department 14. The young woman stopped for a moment, said hello to her mother, and went into the courtroom. I noticed that the daughter did not speak to Mr. Raines, that she, in fact, studiously avoided his glance.
Shortly before ten, Judge Hammes requested that county counsel, the Gonzalez family, Dario’s lawyer, and several doctors meet in her chambers. Minutes passed.
Mrs. Raines became increasingly nervous, restless. A psychiatrist from the hospital in which she lived was present, pacing the hall. Mr. Raines stood, went to him, introduced himself. They talked quietly.
My informant explained to me that this was the second time this spring Mrs. Raines had appeared in court. Several months before, she had been hospitalized as an involuntary patient and had sought a writ hearing. At that time, her daughter had testified she believed her mother able to care for herself, and Judge Hammes had ordered Mrs. Raines released. Recently, against her wishes, Mrs. Raines had again been hospitalized. Mr. Raines, I was told, was Mrs. Raines’s second husband and not the father of her two children. Further, I was told, the Raineses were separated. I suggested that they seemed quite friendly today, and my informant agreed. When Mr. Raines returned to sit by his wife, he pecked her cheek, patted her arm.
An hour had gone by when Judge Hammes’s bailiff called court back into session. At the defense table, Dario Gonzalez sat next to Patricia Rosenberg. Dario’s father and brother sat among spectators in the first row. Judge Hammes, with great solemnity, announced she had decided Dario could leave Camarillo to go home to live with his family. She added that she had given Dario and his father her phone number, at home and at the court, and urged them, should they have any problems or questions, to call her, day or night. She looked, for a long moment, into Dario’s eyes, then said, “Good luck.”
The Raines matter was called. The psychiatrist from the hospital in which Mrs. Raines was resident came to the stand and was sworn. County counsel asked, about Mrs. Raines, “Have you formed a diagnosis as to her mental condition?”
“Yes, I have. She has a bipolar mood disorder, manic phase.” The psychiatrist went on to say that, in his opinion, Mrs. Raines was so gravely disabled as to be unable to provide for her food, clothing, and shelter.
He continued, “After her release from the hospital after a writ hearing, my understanding is that after she returned home, she continued to manifest the severe symptoms of her psychiatric illness. I understand she resided or remained in her bathroom, a small bathroom in the home, for much of the time because she feared allergens in the air were affecting her. I understand she ate very poorly while at home.”
Questioned further, the psychiatrist testified he believed Mrs. Raines showed no insight into her illness, indeed she believed she had no psychiatric illness or disorder.
He said that although she had initially refused medications, she had recently agreed to take them, but only under duress. He was concerned that were she to be released, she would discontinue medications, and her symptoms “would again worsen or at least continue.”
Mrs. Raines’s attorney began his questioning of the doctor. The attorney explained that his client wished to be released to her husband. What was the doctor’s opinion about such an arrangement?
“She has a history of a very difficult relationship with her husband, and in fact, there is a divorce pending. They have been separated, I believe, at least for a year, if not a year and a half.
“Precipitant to one of her first admissions to the hospital was a belief that her husband was trying to harm her in some way or that he was releasing laser beams or laser beam holograms on a closet in which she was hiding. She has a history of being very fearful of him and that relationship. So I am concerned that would not be, at least at this point, a proper placement for her.”
Further, the doctor believed that were Mrs. Raines to be released to her husband that Mr. Raines would not be able to convince her to take medication.
Mrs. Raines was then sworn. Asked if she would take her medication, she spoke in a voice like that of a young girl and nodded obediently. “Yes, I definitely believe I need to take that medication.” She added that she thought the psychiatrist was under the impression that she and her husband were being divorced when, in fact, they were reconciled. “And,” she said, “we are going to stay married, and I would very much like to live with my husband.”
Mrs. Raines’s testimony ended. Judge Hammes noted that Mrs. Raines’s daughter Tiffany had asked to testify. The young woman, seeming entirely self-possessed, strode to the stand and was sworn.
As Tiffany spoke, no one in the courtroom moved, and all eyes, including those of Mrs. Raines, were on the young woman. Her story poured from her. She began at the point her mother had last been discharged from the hospital. “I took her home. I showed her a bill; we had a stack like that.” Tiffany held one hand up to indicate a stack perhaps a foot high. “I said, ‘Mom, what should we do?’ And she ignored it. Right away when she came home, she turned on her radio. Like, before she went into the hospital the first time, that was her big thing; all she would do was listen to the radio and dance around.
“The second day, she started locking herself in the bathroom. She did that for five days. From ten in the morning, and each day it got longer and longer. I’d get really worried. The bathroom is small; you can’t even lie down in it, there’s just a toilet, the window has a curtain on it, and there’s no light.
“The second day she got home, our car was supposed to be repossessed. When I told her about that, she didn’t care; she said, ‘Oh, well, we’ll have to do something.’ But she didn’t want to talk about it.... So I ended up hiding the car. I thought, ‘God, we have to have a car.’
“And then the food situation got really low. I purposely didn’t buy any because I wanted to see what she would do. I told her, ‘We still have the car. You can go get yourself some food.’ The last day she was there we had condiments, like, mustard and ketchup, and three cans of soup.
“The last day, she was in the bathroom from four in the afternoon until the next morning. I was so scared. She was so skinny she could die without more food. So I called the ambulance, and when they came she was still locked in the bathroom.”
“Your testimony,” Judge Hammes said, pleasantly, “is somewhat changed from before.”
Tiffany nodded, quick little up-and-down bobbings of her head. “That’s actually what I wanted to say. When I visited her at the hospital — because my stepdad had, like, actually physically and verbally abused her and because she was scared of him, physically.” Tiffany paused, looked into her lap, “and in the hospital, she said, ‘Tiffany, I am getting worse and worse.’
“So when I was here the last time, I didn’t really say what she was doing at home. I would like to say some of that stuff now.
“In January when I left for school after Christmas vacation, she was fine. We would talk on the phone, like, every night. And things she said started getting really weird.
“She said people were coming to our house in the middle of the night and during the day, and she didn’t know who they were. And she said my stepdad [Mark] was trying to kill her, and I guess she thought my sister was in on it with him too.
“She was sleeping in the closet then. She said my stepdad came to the door with a turban wrapped around his head and nails strapped to his fingers, and he was motioning like this,” Tiffany crooked her index finger, wriggled the finger beckoningly, “that he was going to hurt her, and she said she actually saw this, which really scared me.
“She said another time that she heard my stepdad, I guess having sex on her bed with my sister, and she told them to leave, and I guess they continued, and I said, ‘Well, Mom, did you see this?’ And she said yes.
“She said she got out of the closet and went and looked, and the two were hunched over the bed, and the girl had a gun. That freaked me out. So I called my sister; she was at school. She wasn’t at home.
“Another time, my mom said a helicopter landed in our back yard and the people came inside and were walking around.
“All along, though, she said she was being protected. I said, ‘Well, Mom, what are you talking about?’ And she said that her lawyer had contacted the FBI and that the FBI men were living in our house, and they were living in the attic and under our floor, and we don’t even have a basement, so I don’t know where they’d be living.
“She said they were waiting there until Mark came there and tried to kill her. She kept calling it a sting operation, that they had to witness him trying to kill her before they could arrest him. So she said that was what they were waiting for, and I said I was getting really scared, and she kept saying, ‘Trust me. Trust Randy.’ Randy’s her divorce lawyer.
“Then she said she started watching holograms in her closet, and Mark was good at computers and that he had put them there. She said they were movies, and she would sit there and watch them, and most of them were, like, her being tortured. One she said was my stepdad and my sister and they were, like, shoving animals up her, and she said she watched these for hours.
“I was getting really scared, I said, ‘Well, Mom, when you are watching these movies, are you eating?’ And she said, ‘Oh, sometimes the movies are really good so I don’t want to leave, and when I ask the movies to stop, they don’t, so sometimes I don’t end up eating.’ So that really scared me too.
“I called her one time and she started talking to people in the same room. I’d be crying and sobbing and saying, ‘Mommy, I don’t believe you,’ and she’d be laughing.
“All along it would be, like, the opposite of what it should be. All these months I never cried so much in all my life, and every time I cried, she kinda smiles, like, ‘Oh, life is great.’
“So I was talking to her on the telephone, and she started talking to other people in the same room. ‘Mom,’ I said, ‘who are you talking to?’ ” Tiffany lowered her voice, imitating her mother, “ ‘Oh, it’s Randy and the FBI men.’
“And I said, ‘Mom, will you please put one of them on the phone for me?’ And then she said, ‘Yeah, hold on.’ I could hear her go down the hallway and call, ‘Randy, Randy, will you please come here? Tiffany doesn’t believe that you’re here. Will you please come to the phone?’
“And then she came back, laughing. ‘Oh, it was bad timing, Tiffany, they just left!’ And I go, ‘Oh, my God.’
“So then I came home from school the next day. She was in the closet lying there. And I put my arm around her, and first she kind of responded, and then I let my arm go and she got really cold and, I don’t know, that night was probably the worst night in my life. She was just,” Tiffany narrowed her eyes, stared off into the courtroom as if remembering, “like, the whole time she, like, looked at me, and I will never forget how she looked, like she was possessed or something.
“She thought, I guess, that I was trying to kill her too. I said, ‘Mom, I was not trying to hurt you, you know. How could you think I was trying to hurt you?’ It was awful. During the night, she would say, ‘Do you hear that?’ and I would say, ‘No.’ And I told her I would stay up all night to make sure that no one comes here and hurts you.” Judge Hammes leaned toward Tiffany. “Can I interrupt you? You can’t help your mom right now. It’s beyond your help.” “Well, I don’t know. I’m afraid of my stepdad. If she goes to live with him, he could like ... I don’t know, I mean. I think in the hospital at least they give her medicine. I don’t know what to do. I don’t know.”
Judge Hammes again interrupted Tiffany, “I think that she needs medicine. I don’t know what else to do. Tiffany, thank you so much.”
The judge’s face was somber as she ordered that Mrs. Raines be placed under conservatorship and remain in her present hospital setting.
In the late afternoon I visited with Judge Hammes in her chambers. She had just returned from meeting with two psychiatrists about an 11-year-old boy in an LPS conservatorship. “Articulate, bright, looks you right in the eye, and then you read about his background, and you just have to cry. Too horrible to believe! Wandering around the streets at the age of seven because he hadn’t had anything to eat for three days. Didn’t know where his mother was. Scars all over his body. Placed in a foster home. Brother makes it, he doesn’t. He’s acting out.
“Of course, a child who reacts in a hostile fashion to abuse and abandonment and neglect can’t make it in a foster home, so what happens? The only way that they can get help sometimes is to get into a state mental hospital. It’s so sad it’s beyond words. It’s just awful.”
Judge Hammes said that she’d posed a hypothetical question to the psychiatrists. She’d asked, “What if a child came to you, and the evidence was he had a conduct disorder, and you said, ‘That’s not a mental disorder causing a grave disability.’ What could be done?
“They said that would be horrible, because then you wouldn’t have a place for this kid. He would run away from a foster home, destroy a foster home, he would end up on the street, end up as a prostitute somewhere because you didn’t bring them into the system where they can get help. “Well, those are our choices? Pathetic.” Before Judge Hammes took over the mental health court in January, did she have any idea the magnitude of problems that would come before her?
"No. I had talked to some of the judges who had done this, and they had let me know there would be a lot of stress in this department. I was not aware that juveniles would be involved. I thought it would be only adults. And it’s always the kids who get you. Adults, you figure, ‘Well, by this time there’s not much you can do.’ You feel bad, but it’s not like a child.
“You know what I’m shocked to find out? I worked in juvenile court for two years, early on in my career, and I did a lot of child-dependency and sexual-abuse cases. I worked back in the early ’70s, before the real tide had come in of a big concerted effort to combat child abuse and neglect. Back then, sexually abused children were basically treated as a non-victim. It was like, they’re so young, they’ll be fine.
“In these cases of sexually abused children, however, it’s not like you pulled out a gun and shot someone and you can see the blood. We can’t see it; and six months from now, they have a hard time describing it; ipso facto, there’s no victim. Well, that is simply not the fact.
“Now l am seeing it here, and I am shocked; I am reliving all this earlier stuff, because many of these reports coming across my desk show that these schizophrenic women were sexually abused as youngsters, and schizophrenia took hold shortly after that abuse, and now they are mental patients.”
Traditionally, in San Diego, the mental health court is a five-day-a-week, mornings-only court. In the afternoon, the judge who sits on the mental health bench handles criminal law and motion matters. Judge Hammes said that when she asked to be assigned to mental health court, she did so because she was interested in the criminal law and motion calendar. About the mental health half of her job, she said, “I really didn’t know what I was biting off. Had I known!”
The mental health calendar, she suggested, deserves more time. “Basically, these people are being detained in lockup facilities, and when you consider how many and how fast these decisions are being made, it’s really something else.”
And preparation is time consuming. “Making sure you get everything read! Every time I jump off the bench, I am back in my office, reading.”
Mental health court, she said, is much like small-claims court. “More informal. Lots of hearsay evidence comes in — not at all like the criminal field. And I like this. I think this is closer to pure justice. Actually, I’ve often thought that small claims is the real, pure justice, because both sides can talk. They are, of course, going to offer you some irrelevant material, but in this often spontaneous way, real important stuff gets told to you that might not get told when somebody’s trying to hone to rules. So in a much shorter time, you can get a clearer picture than you can when everyone travels these narrow lanes. It’s much easier, frankly, to get at the truth.
“It is hearsay. But it’s permitted by statute. I am so schooled in criminal law that I still look askance at hearsay, I still go at this hearsay with a little question mark in my brain, and I ask myself, ‘Did this really happen?’
“Things that are important to me are ‘How many hospitalizations?’ That’s usually a verifiable fact. And ‘Has this person a long history of hospitalizations?’ And ‘When they were brought into the hospital, were they brought in by a friend, or by police?’ And ‘Did the police report they were wandering in traffic?’ Because, usually, to get a police officer to pick you up, you have to be doing something pretty extraordinary. Those are the kind of hard facts that tend to be most impressive to me.
“ ‘What is a person’s right to be on the streets?’ is another issue that comes into these hearings. You see people who come in here and who want to live on the streets and do not want a conservator, and you are forcing them to live in a home where there’s a bed. People from liberal and conservative backgrounds cross in this area. And when I had to sit down and think about it, I came in my own mind to the feeling that I don’t personally think that a person should have either the right or the misfortune to be living on the street, full of lice, without health care, without proper nutrition. So that I don’t agree with the side that says if they choose that, they should have it. I don’t think that’s a human, rational choice. Even if they can sound pretty rational and tell you they would prefer that to some other thing, I don’t think they should have that right, if that’s what they want to call it.
“I consider all of it a misfortune. I suppose there are some cases where you might call it a choice, but I still have such a hard time dealing with that. I don’t think you should have it as a right, and if nothing else, from a cold perspective, I don’t think that you do have a right to make it so that when I walk down the street with my kid that I have to explain this horrible situation to my children. I don’t think they should see human beings living like that. I think it’s such a terrible thing that you just can’t do that. You have to find a way to help these people, and if they don’t want the help, then you make them. That’s what I think.”
Did she believe her months on the mental health bench would change her? “It certainly is an eye-opener. You see how vulnerable life makes you. Everybody, all of us. You feel empathy for the people on the other side of that bench, because they could be you or your family member. You feel a little less secure.”
So many cases she hears, she said, left her feeling emotionally drained. “You take them home. You can’t get them out of your head.”
Comments