 Facebook
Facebook
 X
X
 Instagram
Instagram
 TikTok
TikTok
 Youtube
Youtube
One day this past January I walked into Children’s Hospital to see my infant son, born three months prematurely. Within the intensive care unit, he was in a small room that accommodated four babies, and all four were sleeping when I arrived. The two nurses charged with their care were talking quietly; they seemed to forget me as I slipped into a side alcove to pump some breast milk. It took me a moment to realize they were airing their feelings about premature babies One nurse, blonde, delicate, groomed meticulously, was saying if she ever were pregnant and she started to go into labor early — very early — she would simply stay home. She didn’t spell it out, but her implication was clear: she would choose almost certain death for her baby rather than bringing it to the hospital, to the ministrations of people like herself.

Like all things you’re not supposed to hear, her sentiments fascinated me. I couldn't help comparing her words with my actions, couldn't stop marveling at how sophisticated her thinking was compared with what mine had been. Now, in hindsight, I know what she knew: that when a baby is about to be born long before its time, the only certain way tor its parents to retain control over their lives is to hide within their home. In contrast, when things started to go wrong for me and my husband and our unborn child last November, we were total innocents, and so of course we passively delivered ourselves to the experts.
Patricia and Sam Frustaci had months in which to prepare themselves for the recent premature birth of their septuplets in Orange County. My husband and I had about fifty-four hours. This is not enough time, not when a pregnancy brings as much joy and excitement as ours brought us. In our marriage, years had passed in which a child would have intruded, unwanted. But slowly our feelings had changed. When we first began trying to conceive, I still felt ambivalent. But every barren month that passed, my disappointment intensified. We consulted fertility specialists, had tests. I was scheduled to undergo surgery that we hoped would help us, when we learned that I was pregnant, after two years of trying.
So the greatest pleasure of this pregnancy was our absolute certainty that we wanted it. We had lived through a vision of childlessness and found it bleak. Another pleasure was my seeming good health; morning sickness never bothered me. Toward the end of my sixth month, I was writing in my journal about how good I felt, how thrilling labor seemed, three months away. “I’m not close enough to it to worry too much or be physically uncomfortable,” I recorded. “I feel intensely in love with Steve. . . . Every night, settling down to sleep, with the warmth of him next to me and the baby inside, brings me unrecountable pleasure, and waking up to snuggle for a few moments in the morning is the coziest, sweetest time I’ve ever known."
Thirteen days after I wrote that, a warm fluid began to seep out from deep within me. I happened to be out on the campus of San Diego State and I rushed to the nearest bathroom. The liquid was clear and sweet-smelling, and I knew it was amniotic fluid (the liquid in which the baby is suspended). Later that afternoon, when I finally reached my gynecologist on the phone, he tried to calm my fears, suggesting that maybe it was mucus or urine. He told me to stay in bed, as still as possible, and to come to his office the next morning.
Throughout the night, the liquid continued to leak out, a few tablespoons at a time, and my horror pooled, and grew. My gynecologist’s confirmation the next morning that it was indeed amniotic fluid was unnecessary; I knew that my baby’s safe harbor was draining out of me, and I felt wild with despair, with incredulity. My doctor, David Priver, took samples of the fluid to be sent for laboratory analysis; a test would tell us something about how far developed the baby’s lungs were after only six months of gestation, a crucial question, since once out of the womb, a baby must breathe to live; underdevelopment of the lungs is the biggest killer of premature babies. Priver also conducted a sonogram, and from the ghostly images on the screen he guessed that the baby weighed about two pounds. Finally, a sample of my blood was drawn to see whether I showed signs of some infection, the most common culprit behind this "premature rupture of the membranes.”
Priver sat behind his desk and gave us his blunt prediction: I would probably go into labor within twenty-four hours. The same question seemed to arise from both Steve and me simultaneously. If the baby survived the birth, what would be its chances of a normal, healthy life? Priver looked grim and said he would be frank with us, that with a child born that small and that early, there was significant risk it would suffer some impairment. But he hastened to add that before the birth — if there were to be one — we would speak with one of the neonatologists from Children’s Hospital who could explain to us in detail what we faced. A neonatologist would be with us in the delivery room, and would be prepared to make a split-second evaluation of whether the baby’s life was truly viable. “I’ve talked to all those guys and I know where they’re coming from philosophically,” Priver said. We wouldn’t have to suffer through the ordeal of a Baby Doc-type situation, in which the parents had met with resistance to their desire to avoid heroic interventions to save their grossly handicapped infant.
Priver’s words comforted us both, but somehow they seemed to grow more and more distant the next day, after our arrival at Sharp Hospital. I had spent the night at home, in bed, trying to remain immobile, trying to will the placenta inside my body to heal, but by late the next morning my pulse and temperature had begun to climb, as had the baby’s heartbeat (we had borrowed an electronic stethoscope from a midwife friend). At the hospital, a fetal monitor confirmed that labor had begun, but after an hour or so, Priver saw that my cervix had barely dilated. The baby’s skull was probably too fragile to protect adequately against brain damage during a long and arduous vaginal delivery, so the doctors would take the baby by Caesarean section, as soon as possible.
The appearance of neonatologist Larry Johnsgard moments before I went into the delivery room seemed to me almost an afterthought on his part. In addition, he made no mention of any split-second delivery-room decisions; instead, all he seemed to talk about was how little he could tell us about what would happen either to us or to our baby. One thing we could count on, he said, was for things not to go smoothly; tiny premature babies almost always experienced precipitous ups and downs. We should brace ourselves for the baby to remain in the hospital until about the time of its due date, three months hence.
We asked about the baby’s chances of survival and, even more urgently, what chance it would have of a normal life, and to each such question the neonatologist seemed to shrug his shoulders; indeed, to me it seemed as if he were offended by our hunger for such numbers. “I really don’t like to talk statistics,’’ he demurred. “I just don’t think it’s fair to you or your baby.” Resentment and hostility flared up within me; the doctor seemed cavalier, patronizing, almost impatient with the delays caused by our questions. I finally blurted out what had been gnawing at me: didn’t my husband and I have some decisions to make in the midst of this crisis? Not really, the neonatologist told us.
The hour that followed, the Caesarean section, was a vortex of fear and pain. At some point I had begun to wish, secretly, that my baby would be a boy, and I remember a brief stab of elation at the news of his sex. I remember the shock of hearing a tiny voice pierce the delivery room, crying. Later, right before they rushed him away, voices urged me to look at my son. I was shaking violently, and the drugs they had given me made it hard to focus my eyes. I know I looked where they directed, but today I have no memory of what I saw.
Later I learned that my husband, Steve, had accompanied the baby on the long journey through the corridors that connect Sharp Hospital’s maternity ward with Children’s Hospital’s Newborn Intensive Care Unit (NICU). The baby, already connected to a half-dozen wires and tubes, rode within a portable incubator that blinked and beeped like a robot of science fiction. When Steve finally reported back to me in the recovery room, I was surprised to hear a note of ebullience in his report of how the baby had shaken his clenched fists and kicked his tiny legs. “He was bright red, and he was angry!" When Steve saw this, he said, he felt that the baby wasn’t about to die.
That evening Steve also was introduced to the procedures in Children’s Hospital’s NICU, where our son had been placed. I wasn’t able to tolerate the fifteen-minute trek there until early the next afternoon, and when Steve finally wheeled me over and explained where to check in with the receptionist, where to obtain a surgical gown, where to wash my hands, I felt like a novitiate in some frantic, underground society.
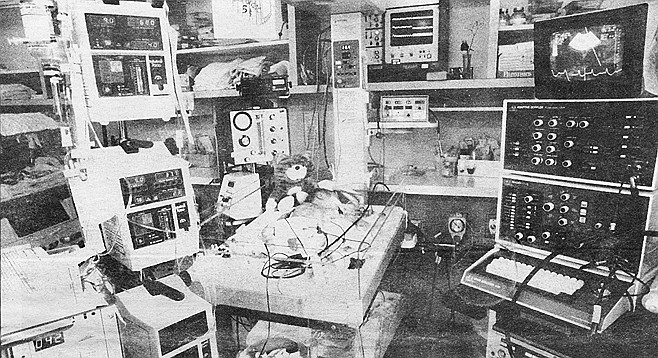
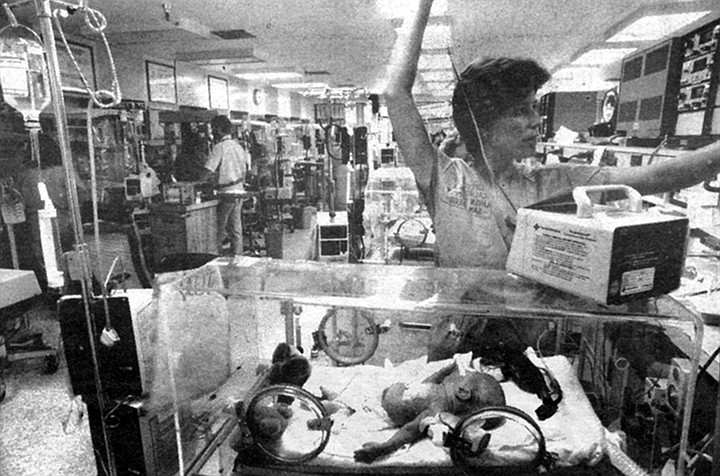
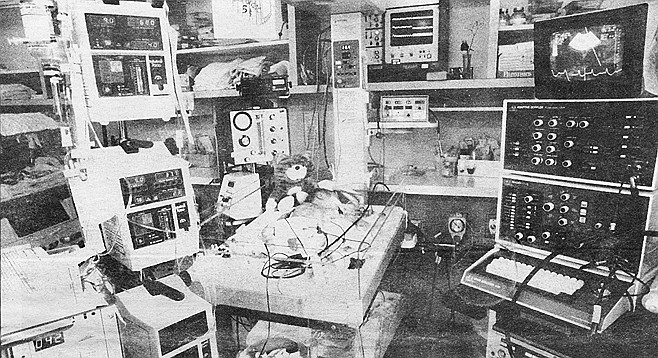
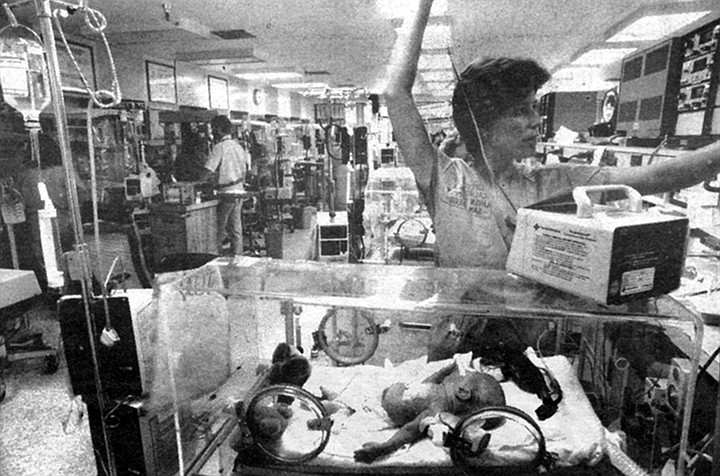
This was a place of intense, concentrated activity, one of those places too densely crammed with sights and sounds for the newcomer to be able to perceive all of that with which he is being bombarded. It is a place bustling with people in hospital gowns, up to a dozen and a half nurses and ten doctors at a time, plus technicians and receptionists and custodians and visitors. Alarms sound routinely here, every minute or two, announcing that this baby’s heart rate is dropping, that that one has stopped breathing, that one of the dozens of intravenous lines has ceased to flow. Rock music churns in the background, syncopated by the buzz of phones. This is a page out of Brave New World, not a nursery.
Through this turmoil, Steve led me to our baby, a tiny red figure lying flat on his back, arms and legs splayed wide. “What a nice face he has,” I thought. Thick white tape obscured part of it, tape that was holding some of the tubes in place. His eyes were closed. But his features looked delicate and well formed, his eyes large and deep-set, his head covered with a fuzzy haze of red-gold hair. His face sustained me.
I could look at it and imagine what a strong and handsome face it might become, and somehow that allowed me not to see him coldly, objectively, as a three-month-premature baby, which is good, because that sight is one of the most pathetic, most heart-breaking in the world. Newborn premature babies look a lot like the babies starving in Africa, with their outsized heads and visible rib cages — except a very premature baby is so stunningly tiny. My son was one inch longer than a schoolkid’s ruler, and he weighed two pounds, five ounces.
He looked, on the one hand, astonishingly human, with tiny, perfect hands and toes, tiny, perfect fingernails and toenails. On the other hand, the machinery made him look like an alien creature. The tape on his face held in place a tube that ran into his mouth and down into his lungs, aiding with his breathing. Another tube, entering his nose, was used to suction secretions in his lungs. Five separate electronic probes,- some wider than his hand-span, were glued to his body, sensing his heartbeat, respiration, body temperature, and blood-oxygen levels. An intravenous line had been sewed into a blood vessel in his navel to act as a high-tech umbilical cord; blood samples would come out through this line while nutrients and fresh blood would enter him through it. Most pathetic of all were the cloth restraints that pinned his wrists to the bed, preventing him from grasping at the equipment which invaded him.
Somehow all the machinery seemed to siphon attention away from the baby. The machinery was lively, flashing numbers and emitting noises; the baby, on the other hand, lay as still as something washed up from the sea, half drowned. Steve and the baby’s nurse eagerly explained to me each machine’s function, and not long after they had finished, it seemed time to return to my hospital room at Sharp. Adrenaline buoyed us; I felt amazed that both the baby and I were alive. I also felt warmed every time a friend would call and congratulate us (instead of offering condolences). Although Steve and I had not expected to pick a name for another two months, we quickly settled upon “Michael.” It sounded strong and normal.
The next morning was a Monday. Steve had to work, so an aide wheeled me over to the NICU alone. This time at Michael’s bedside I found even more machinery and a cluster of people; someone explained that a cardiologist was using an ultrasound machine to examine the baby’s heart. As big as a small forklift, the machine squealed and panted like some demon, while complex waves pulsed on various screens. Only the cardiologist and her assistant were paying any attention to the testing — I know that now — but at that moment it seemed as if a crowd of strangers was gaping at my baby’s innermost essence. No one ever should have seen this part of him, not even me, and I felt depthless sorrow.
Eventually the doctor and the ultra-sound machine completed their tasks, and finally I could pull up a stool and sit next to the baby. He lay on a mattress on a metal platform underneath electric coils that radiated heat. Sheets of clear plastic surrounded the platform to contain the warmth, but I could lift the plastic to touch him gently and talk to him. I tried this, said hello to him and asked him how he was doing, and suddenly I felt as if everyone in the room was watching me, witnessing my crude, blundering attempts to act like a mother. Every time I said something to Michael, waves of something like shame flooded me and I found myself compulsively sneaking glances all around me, to see who was looking. I wanted to hide, to take my baby and hide with him, and hold him, and instead it felt as if we both were naked and on display.
Gradually these feelings subsided. Within a day or two I began to learn how the doctors and nurses were talking about my baby, through the medium of the machines. Children’s Hospital's NICU has a policy whereby every parent of a child in intensive care may visit or telephone the unit at any time of the day or night, and as I began visiting and calling, the machines surrounding Michael gradually stopped being a shiny jumble of garbage and started taking on some individuality, like characters in a play. There were, for example, the “bili lights,” banks of blue-white light aimed at Michael, so bright that he had to be blindfolded. I learned that the bili lights were there because Michael had jaundice; that is, his immature liver was failing to break down a toxic substance in his blood called bilirubin. The lights were supposed to help his body break this down. We could tell how well this was working from daily tests of the bilirubin levels in his blood.
So when we called or visited, one of the questions we could ask was, “How is his bilirubin level today?” They could answer this question. They would say, “It was thirteen,” or, “It was eleven,” or, “It stayed the same — still nine.” We learned that when it reached seven or eight, the noxious bili lights would be taken away.
I learned about the respirator that was inserted down into Michael’s lungs within moments of his birth. Many premature babies need such assistance because their immature lungs lack surfactant, a fluid coating that keeps them from collapsing when they exhale; every breath then becomes a terrible struggle. Michael’s major respiratory problem, however, was a tendency to forget to breathe. This condition, called apnea, also is extremely common in premature babies; the centers in their brains that control breathing are simply immature. As explained to me, the respirator was giving Michael enough of a boost to insure that his body was getting enough oxygen.
I learned that the respirator had two important components. First, the nurses could adjust the percentage of oxygen that the machine was puffing into his lungs. Normal air is composed of twenty-one percent oxygen, but for many premature babies that isn’t enough. They need to breathe in a higher percentage of oxygen in order to wind up with enough in their blood. Some need as much as a hundred percent oxygen (a very bad situation, since too much oxygen is poisonous to humans; one common complication of breathing this much oxygen is eye damage, even blindness). Michael never needed much more than about thirty-five percent oxygen, and from hour to hour the nurses would try to decrease that amount (checking the oxygen levels in his blood to see if he was tolerating the weaning process).
The other variable of the respirator was the number of breaths per minute it could give to the baby — anywhere from 150 down to four. The constant goal was also to reduce this number, to wean the baby off the respirator entirely. So we could also always ask, “What percentage of oxygen is he getting?” and “How many breaths a minute?” These questions they could answer, with ease. But it didn’t take me long to figure out that there were some questions it would do no good to ask, not then. Will he be blind? Deaf? (We couldn’t even begin to test his sight and hearing for several weeks.) Will he be mentally retarded? Physically incapacitated? (It would be months if not years before we could make these predictions.) What emotional scars does it leave upon someone to come into the world three months early, to have one's first experiences of the world be those of prolonged suffering and pain?
Those questions haunted me, but if they had no answers, the answers we did receive the first two weeks were encouraging. Although the heart sonogram showed that one of the little blood vessels outside Michael's heart failed to close properly, treatment with a drug seemed to correct the problem within a few days. Better still, head scans revealed no signs that the trauma of birth had caused bleeding in his brain, a major cause of cerebral palsy. Five days after he was born, he somehow yanked the respirator tubes out of his lungs, and he did well without the breathing assistance. Eight days after his birth, one of the nurses let me wash him (with moistened cotton balls), and for the first time since his birth I heard him cry — miniature, high-pitched squeaks. The same nurse let me hold him inside the warmer, cradling in my arms his whole assembly of heaters and wires and gauges. Steve held the oxygen tube near his face, and Michael looked at me, his eyes as large and blue as those of the fetus in 2001. He grasped my finger with his tiny hand, and as I talked to him, he seemed calmer.
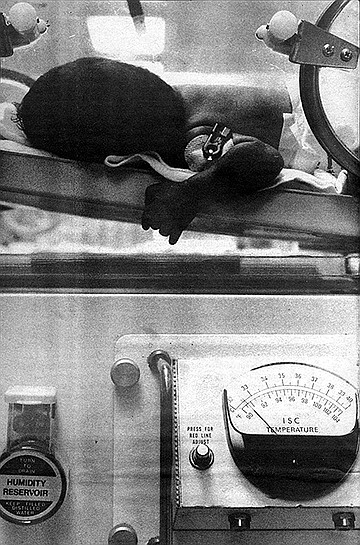
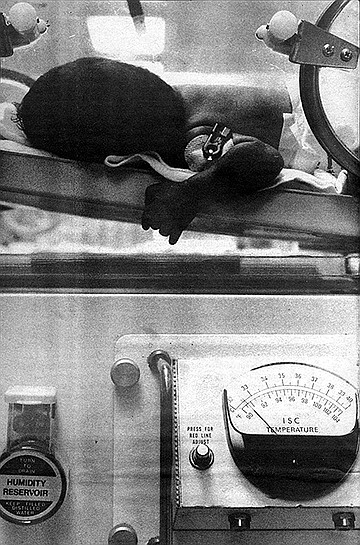
Within days he moved from the open warmer into an incubator (nowadays they call them isolettes). The nurses routinely began inserting a tube down into his stomach and giving him tiny amounts of the breast milk I was pumping — starting with a sixth of an ounce every three hours, and ever so gradually increasing the quantity. Two weeks after Michael’s birth, Dr. Johnsgard told us he thought Michael was doing “superbly.” We tried to tell ourselves not to relax, not to start to feel confident. But at night, after a couple of glasses of wine, we also started to talk about how a gentle birth probably wasn’t all that important, and how — if he survived the hospital unscathed — he might even be better off for having gotten this head start on the real world.
Things fell apart seventeen days after he was born. Once again he was forgetting to breathe. Often. Ten times, twelve times during an eight-hour shift.
This is what it was like when it happened. If you were standing by his side, and you knew what you were looking for, you would see a subtle change in his coloring. Instead of looking pink, he would start to appear pale, with a grayish cast around his mouth, his eyes, his fingernails. About this time, the electronic monitor next to him, which gave a constant read-out of his heartbeat and respirations, would begin to change, the heartbeat numbers dropping from 150 or so beats a minute to 120, 100, 90. An alarm would begin to shriek, and a nurse would walk over and open the portholes of his isolette. She would gently rub her fingers over his back, or pat his bottom, or if that weren't sufficient, she would snap her finger against the bottom of his feet. Invariably, this worked. You could see him take a deep breath and the pink glow would return.
In the NICU slang, these spells were “A’s and B’s,” for apnea (the failure to breathe), and bradycardia (the slowing of the heartbeat that usually accompanied the apnea). And so the pattern of our daily questions changed. “How many A’s and B’s did he have?” became the first thing out of our mouths. Some eight-hour shifts would pass with one or two, then he'd have six, seven, nine. We’d been warned that this might happen, warned that time and time again a tiny preemie would do splendidly for a week or two, then would seem to tire out and would once again need the machine to help him breathe. Warnings cannot adequately prepare one for such a setback, and depression engulfed both of us. I wept daily. But after a week of watching Michael’s struggle, of watching him turn dusky over and over again. I felt almost relieved when on December 11, twenty-four days after he was born, he went back on the respirator once again.
The next day he looked visibly pinker and more rested. The day after that he looked awful, with a 102-degree fever, his stomach distended. The staff began to fear he might have contracted some hospital-bred infection and so they began a grueling series of tests: of his blood, his urine, his spinal fluid. The next five days he steadily improved, then at 7:30 one morning we received a call from the neonatologist on duty in the NICU. He told us that during the night Michael’s heartbeat had begun dropping — and the nurse couldn’t rouse him. until finally the team had taken out the respirator tube and replaced it with another one. Perhaps the first tube had gotten clogged with mucus (completely cutting off Michael’s air supply) or perhaps some other problem was developing. We would have to wait and see. With that incident, Michael went from needing six ventilations per minute of room air to twenty breaths per minute of air containing fifty-five percent oxygen.
Slowly, painstakingly, the weaning process began again. Steve and I spent Christmas Eve and part of Christmas Day in the NICU. Our best present came the day after Christmas, when the staff judged that once again Michael was ready to try breathing unassisted. He weighed three pounds, two and a half ounces. Steve and I had been told that someday, before he could come home, he would probably move over to the less-intense “special care nursery” at Sharp Hospital. But the day Michael came off the respirator for the second time, we couldn’t imagine his ever leaving the NICU.
I often marvel at how quickly human beings adjust to their environments. In a few weeks, the NICU had become as familiar as home, which is strange, considering that it has to rank as one of the most unnatural places in the world. Here people, in effect, are growing babies in artificial wombs. Here there is no day or night. The bright lights shine ceaselessly, and when we question whether that’s good for the babies, the staff responds that they need to see whether the babies are changing color, a much better indication of distress than any machine. The noise of the telephones and the alarms combines with radio station B-100. I wondered if classical music might not be better for the babies, but I held my tongue; aggressive, hard-driving rock seemed so appropriate for the NICU nurses.
Over the weeks, I met dozens upon dozens of these young women (and all were women, and most were young, just as all five of Children’s staff neonatologists are middle-age men). Michael seemed to have three new nurses (one for each shift) every day. Some were chatty and some were impassive. Some were aloof, though a much higher percentage were so maternal and sympathetic that their warmth would bring tears to my eyes. Far more striking than their differences, however, were the things they had in common. Like air traffic controllers, they thrived on having three things to do at any given moment, in an atmosphere of imminent crisis. Because they have to make minute-by-minute decisions, the NICU nurses work more independently of doctors than nurses in other areas of medicine. They are far more important in the lives of their tiny charges than are the babies’ own parents, and I think the nurses know this, and like it.
If the nurses are the front-line troops of the NICU, hopped up and elbow-deep in the mundanities of caring for very tiny, very sick babies, the neonatologists are the generals. Once a day they and various other key medical personnel would float from one isolette to the next, pondering each baby’s case, making strategic decisions in a manner that looked calm and measured and judicious (parents were required to retreat to some distance during these “rounds”). The vast majority of the time I talked not with the neonatologists but with one of the three nurse-clinicians, Donna Brandon. Brandon was more like a diplomat than a soldier. She knew what the neonatologists were planning, and she could work shoulder-to-shoulder with the nurses, but she also was our main source of information about Michael’s overall status. Almost every day I besieged her with dozens of questions, and she answered them patiently. Slowly, day by day, I began to get an insight into the frontiers of medicine, of how imprecise it is, how dependent upon trial and error — of how, even when something “works,” how many questions never get answered.
One day I had another insight into modern American medicine. It suddenly struck me that this experience in the NICU was the only time in my life I’d ever been in a place where everyone acted as if the cost of things were irrelevant. Almost everything, no matter how shiny and sturdy-looking, was used once and thrown away, or so it seemed. No one ever so much as mentioned the price of anything — be it alcohol wipes or brain scans — because price was never a consideration in whether to do something. Not that I wanted to know what Michael’s care was costing us. Steve’s private insurance covered everything except the first $1500, but it still terrified me utterly to hear what those expenses were; the hospital bill alone — not including doctors’ fees — for just the first nine days was more than $25,000. Other babies who lacked private insurance were substantially covered by state and federal funds. Steve commented that the NICU was the most democratic place he’d ever known; here you could find a Mexican farmworker’s baby next to a La Jolla lawyer’s baby, both receiving the most sophisticated medical care on earth, administered by people to whom money seemed to be no object.
We guessed that some of the other parents were farmworkers, though we never knew for sure. Throughout all the weeks, we never really got to know any of the other parents. I yearned to talk to some of them; it seemed as though no one could really understand what I was experiencing except for someone in the same position. But we never made the connections; we weren't there at the same times or were too shy to step up and introduce ourselves. But even though the other parents were shadowy figures, flitting in and out of the background, their babies were always there, and Steve and I talked about them daily, and came to care about them. The nurses and the doctors all knew what was wrong with each baby, but they didn’t share the daily news with us; some unspoken code seemed to proscribe this. Still, Steve and I could read the posted names of the babies located near Michael, and by eavesdropping on the nurses, we got a vague idea of which were seriously ill, which were thriving.
All the books about premature babies I was reading warned me not to compare Michael with the other babies, but the comparisons were inevitable. For weeks upon weeks it seemed as if he were the tiniest baby in sight; baby after baby moved in, stayed for a few days, then moved out, while we remained. Then one day in early January I came in to find a new baby occupying the open warmer next to Michael’s isolette. He was a boy twenty-six or twenty-seven weeks (gestational age), and he weighed two and a half pounds — very close to what Michael had been. Seven and a half weeks had passed since Michael’s birth — and already it was hard for me to believe that Michael had ever looked so raw, so horribly fragile, like a broken baby bird. That day, weighing four pounds and two ounces, my son looked plump, even robust, and I knew that soon we would be leaving the NICU.
It actually took two more weeks, time in which Michael began learning to drink my breast milk from a bottle (instead of having the nurses pour it into his stomach through a tube). Laboriously he would suck half an ounce and fall asleep. He would choke, turn blue, set off the heart alarms. It took nine days to get him to consume his full quota: one and one-third ounces. Four days later we got permission for him to feed at my breast for the first time; and later that day Michael once again rode in a “transport incubator” through the corridors that connect Children’s with Sharp Hospital, where he checked into the special care nursery.
I hated the Sharp nursery that first day. I didn’t recognize any of the nurses, didn’t know to whom I could turn for information. The place seemed sterile and tomblike. Being there reminded me of what had happened when we were there two months earlier. I was forced to relive the trauma of Michael’s birth.
But it took only a day or two for me to see that I had grown addicted to the maelstrom of the NICU, that the Sharp nursery — clean, quiet, orderly — was a much better place for babies. Here, if all went well, Michael only would need to practice drinking his meals orally to grow a little plumper.
All didn’t go well. Five days after entering the Sharp nursery, Michael’s skin suddenly began looking as if it had been washed with a yellow stain. Tests showed that his blood contained a very high level of bilirubin. Once again he had jaundice. But unlike the jaundice that had afflicted him immediately after birth, this jaundice was frightening. Michael’s liver wasn't working properly, and this time the doctors didn’t know why. Once again the neonatologists were demanding blood, urine. Once again they ordered ultrasound tests, and then they called in more doctors, specialists in baby gastrointestinal systems. The experts ordered yet more exotic tests; technicians injected radioactive particles into one of Michael’s veins and watched a screen to see that the particles passed through the liver and out into his bile tracts.
The doctors finally concluded that Michael’s liver probably had been irritated by some of the intravenous fluids he had been given in the NICU. This happened fairly often, about fifteen percent of the time, and Michael’s jaundice would probably just go away, they guessed. Since his bottle feedings were improving, suddenly everyone was talking about when to discharge him. We picked him up from the hospital February 16, two days short of his due date. He was five pounds, four ounces, and three months old.
It took twenty minutes to drive from Children’s Hospital to our home, but it took months to leave the hospital behind. Weeks passed before I could bring myself to stop keeping hourly records, like a nurse, of everything from Michael’s temperature to his bowel movements. It took me even longer to stop worrying obsessively about every single milliliter of milk he failed to consume; not until we finally switched over to complete breast-feeding was I able to begin to relax, as Michael steadily gained weight. We Came home from the hospital with a rented machine that monitored his heartbeats and respirations. Every night we connected Michael to it with a soft rubber belt which we fastened around his chest with Velcro tabs. When three and a half months passed with no significant apnea spells, we finally returned the monitor. Recently Michael went back to the hospital for day surgery on a hernia, another ailment that commonly plagues preemies. The scar from that is fast fading.
Other signs of his experience will take longer to recede. X-rays of his lungs still show some mild damage, but unlike adults, babies can grow new lung tissue, and we expect that Michael’s should heal by the time he’s two years old. Another legacy of Michael’s prematurity visible to sharp observers is the shape and size of his head, large in comparison to the rest of his body and flattened on the sides (by the pressure of lying on the sides for three months, instead of being supported uniformly in the womb). Michael also still is very small, though our pediatrician thinks he will catch up to the normal size range by the end of this year. He cried and fretted throughout most of his first months at home; preemies are notable for their early irritability.
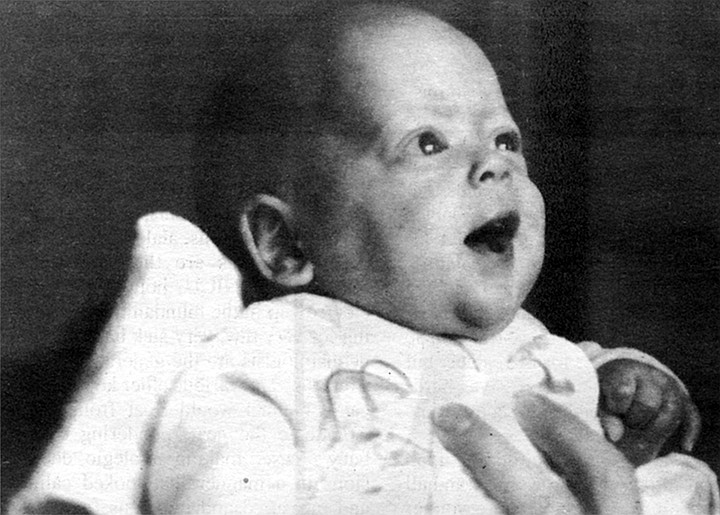
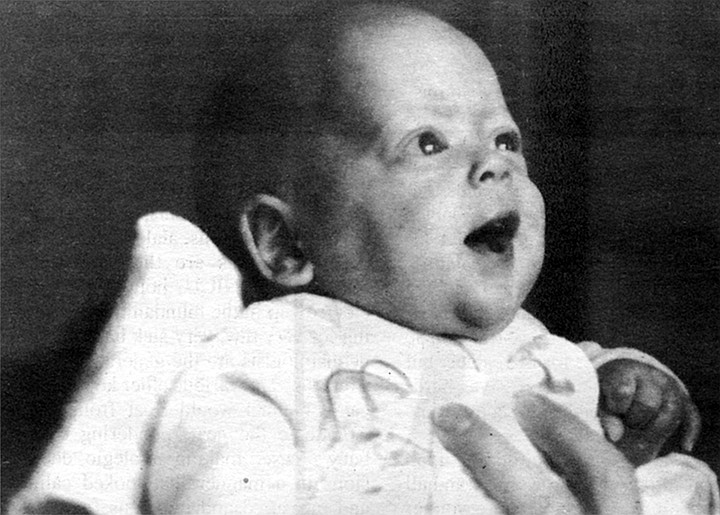
At the same time, we’ve been so lucky. His eyesight and hearing seem to be fine, and he’s been very healthy. The jaundice has disappeared. He’s an alert, bright-eyed baby who smiles readily, huge delighted grins that brighten up the whole room. He’s active and vigorous and he’s doing most of the things done by babies his age (minus three months): reaching for and gumming things, creeping and rolling over, babbling.
It will be years before we can definitively answer whether Michael’s prematurity has hurt his development. The scientific studies that exist aren’t much help in making predictions. For one thing, there aren’t a whole lot of them; just ten years ago, most babies born three months early simply died. One of the major studies that have been done indicates that only about five percent of very early, very small preemies suffer severe developmental handicaps — but many (an additional thirty-five percent) develop milder problems such as learning and behavioral disorders, lack of physical coordination, or hyperactivity. To complicate things still further, a host of factors appear to influence the odds, including everything from the parents’ socioeconomic levels to whether or not the baby was on a respirator.
I never asked that one nurse in the NICU why she would let her (hypothetical) premature baby die, but I assume she had to be thinking of all the things that can (and do) go wrong. I know she was aware of how nightmarishly, horribly wrong things become once in a while, as they had for one of the NICU’s little patients. Born only two months prematurely, he had progressed quite well until he had developed an infection that put him back on the respirator, whereupon his lung disease failed to improve. For a year and a half. At eighteen months, he had spent his entire life in the NICU, and was still on a respirator. When Michael was there, this baby’s family members were preparing themselves for the homecoming of the little boy — and all his medical equipment, including the breathing machine.
Another nurse, whose mother was a social worker specializing in the mentally retarded, told me that her mother had never forgiven her for choosing to work with the tiny preemies. “She says, ‘Your patients today are my clients in the future,’ “ the nurse said. When Michael was still in the hospital and I didn’t know if he would be mentally retarded, when I didn’t know if he too would develop some infection that would lead to chronic lung disease, I seethed at the circumstances that had trapped Steve and me into facing such terrifying prospects.
But what would I have done differently, even if someone had been brutally honest with me, had said, “Once you enter that hospital, they’re going to cut you open and take your baby away from you for a very long time, and when they finally give him back there’s at least a forty percent chance he’ll be damaged”? Even if I had known that, I don’t see how I could have stayed home and delivered Michael alone, to die. And once I was in the hospital, how could the doctors have acted differently? Not knowing precisely what the consequences of their interventions might be, how could they do other than to employ their skills and hope for the best? I’ve been thinking about this ever since Michael was born, and I don’t have any other answers. Technology has forced us to play these games with these babies’ lives,yet at every turn we have only one move.
Since Michael’s birth, several friends and acquaintances have called him a “miracle baby.” Every time I hear the phrase, I squirm. Miracles are supposed to be instantaneous and inexplicable and free. What we lived through cost more than a quarter of a million dollars and involved three months of round-the-clock care by dozens of people who were among the most skilled, dedicated, and hard-working I’ve ever known. There are other times, too, however, when I’m holding Michael close to me and he looks at me with his big blue eyes and his face lights up and I am overcome with love. Then I think maybe I don’t know the meaning of the word miracle.

One day this past January I walked into Children’s Hospital to see my infant son, born three months prematurely. Within the intensive care unit, he was in a small room that accommodated four babies, and all four were sleeping when I arrived. The two nurses charged with their care were talking quietly; they seemed to forget me as I slipped into a side alcove to pump some breast milk. It took me a moment to realize they were airing their feelings about premature babies One nurse, blonde, delicate, groomed meticulously, was saying if she ever were pregnant and she started to go into labor early — very early — she would simply stay home. She didn’t spell it out, but her implication was clear: she would choose almost certain death for her baby rather than bringing it to the hospital, to the ministrations of people like herself.

Like all things you’re not supposed to hear, her sentiments fascinated me. I couldn't help comparing her words with my actions, couldn't stop marveling at how sophisticated her thinking was compared with what mine had been. Now, in hindsight, I know what she knew: that when a baby is about to be born long before its time, the only certain way tor its parents to retain control over their lives is to hide within their home. In contrast, when things started to go wrong for me and my husband and our unborn child last November, we were total innocents, and so of course we passively delivered ourselves to the experts.
Patricia and Sam Frustaci had months in which to prepare themselves for the recent premature birth of their septuplets in Orange County. My husband and I had about fifty-four hours. This is not enough time, not when a pregnancy brings as much joy and excitement as ours brought us. In our marriage, years had passed in which a child would have intruded, unwanted. But slowly our feelings had changed. When we first began trying to conceive, I still felt ambivalent. But every barren month that passed, my disappointment intensified. We consulted fertility specialists, had tests. I was scheduled to undergo surgery that we hoped would help us, when we learned that I was pregnant, after two years of trying.
So the greatest pleasure of this pregnancy was our absolute certainty that we wanted it. We had lived through a vision of childlessness and found it bleak. Another pleasure was my seeming good health; morning sickness never bothered me. Toward the end of my sixth month, I was writing in my journal about how good I felt, how thrilling labor seemed, three months away. “I’m not close enough to it to worry too much or be physically uncomfortable,” I recorded. “I feel intensely in love with Steve. . . . Every night, settling down to sleep, with the warmth of him next to me and the baby inside, brings me unrecountable pleasure, and waking up to snuggle for a few moments in the morning is the coziest, sweetest time I’ve ever known."
Thirteen days after I wrote that, a warm fluid began to seep out from deep within me. I happened to be out on the campus of San Diego State and I rushed to the nearest bathroom. The liquid was clear and sweet-smelling, and I knew it was amniotic fluid (the liquid in which the baby is suspended). Later that afternoon, when I finally reached my gynecologist on the phone, he tried to calm my fears, suggesting that maybe it was mucus or urine. He told me to stay in bed, as still as possible, and to come to his office the next morning.
Throughout the night, the liquid continued to leak out, a few tablespoons at a time, and my horror pooled, and grew. My gynecologist’s confirmation the next morning that it was indeed amniotic fluid was unnecessary; I knew that my baby’s safe harbor was draining out of me, and I felt wild with despair, with incredulity. My doctor, David Priver, took samples of the fluid to be sent for laboratory analysis; a test would tell us something about how far developed the baby’s lungs were after only six months of gestation, a crucial question, since once out of the womb, a baby must breathe to live; underdevelopment of the lungs is the biggest killer of premature babies. Priver also conducted a sonogram, and from the ghostly images on the screen he guessed that the baby weighed about two pounds. Finally, a sample of my blood was drawn to see whether I showed signs of some infection, the most common culprit behind this "premature rupture of the membranes.”
Priver sat behind his desk and gave us his blunt prediction: I would probably go into labor within twenty-four hours. The same question seemed to arise from both Steve and me simultaneously. If the baby survived the birth, what would be its chances of a normal, healthy life? Priver looked grim and said he would be frank with us, that with a child born that small and that early, there was significant risk it would suffer some impairment. But he hastened to add that before the birth — if there were to be one — we would speak with one of the neonatologists from Children’s Hospital who could explain to us in detail what we faced. A neonatologist would be with us in the delivery room, and would be prepared to make a split-second evaluation of whether the baby’s life was truly viable. “I’ve talked to all those guys and I know where they’re coming from philosophically,” Priver said. We wouldn’t have to suffer through the ordeal of a Baby Doc-type situation, in which the parents had met with resistance to their desire to avoid heroic interventions to save their grossly handicapped infant.
Priver’s words comforted us both, but somehow they seemed to grow more and more distant the next day, after our arrival at Sharp Hospital. I had spent the night at home, in bed, trying to remain immobile, trying to will the placenta inside my body to heal, but by late the next morning my pulse and temperature had begun to climb, as had the baby’s heartbeat (we had borrowed an electronic stethoscope from a midwife friend). At the hospital, a fetal monitor confirmed that labor had begun, but after an hour or so, Priver saw that my cervix had barely dilated. The baby’s skull was probably too fragile to protect adequately against brain damage during a long and arduous vaginal delivery, so the doctors would take the baby by Caesarean section, as soon as possible.
The appearance of neonatologist Larry Johnsgard moments before I went into the delivery room seemed to me almost an afterthought on his part. In addition, he made no mention of any split-second delivery-room decisions; instead, all he seemed to talk about was how little he could tell us about what would happen either to us or to our baby. One thing we could count on, he said, was for things not to go smoothly; tiny premature babies almost always experienced precipitous ups and downs. We should brace ourselves for the baby to remain in the hospital until about the time of its due date, three months hence.
We asked about the baby’s chances of survival and, even more urgently, what chance it would have of a normal life, and to each such question the neonatologist seemed to shrug his shoulders; indeed, to me it seemed as if he were offended by our hunger for such numbers. “I really don’t like to talk statistics,’’ he demurred. “I just don’t think it’s fair to you or your baby.” Resentment and hostility flared up within me; the doctor seemed cavalier, patronizing, almost impatient with the delays caused by our questions. I finally blurted out what had been gnawing at me: didn’t my husband and I have some decisions to make in the midst of this crisis? Not really, the neonatologist told us.
The hour that followed, the Caesarean section, was a vortex of fear and pain. At some point I had begun to wish, secretly, that my baby would be a boy, and I remember a brief stab of elation at the news of his sex. I remember the shock of hearing a tiny voice pierce the delivery room, crying. Later, right before they rushed him away, voices urged me to look at my son. I was shaking violently, and the drugs they had given me made it hard to focus my eyes. I know I looked where they directed, but today I have no memory of what I saw.
Later I learned that my husband, Steve, had accompanied the baby on the long journey through the corridors that connect Sharp Hospital’s maternity ward with Children’s Hospital’s Newborn Intensive Care Unit (NICU). The baby, already connected to a half-dozen wires and tubes, rode within a portable incubator that blinked and beeped like a robot of science fiction. When Steve finally reported back to me in the recovery room, I was surprised to hear a note of ebullience in his report of how the baby had shaken his clenched fists and kicked his tiny legs. “He was bright red, and he was angry!" When Steve saw this, he said, he felt that the baby wasn’t about to die.
That evening Steve also was introduced to the procedures in Children’s Hospital’s NICU, where our son had been placed. I wasn’t able to tolerate the fifteen-minute trek there until early the next afternoon, and when Steve finally wheeled me over and explained where to check in with the receptionist, where to obtain a surgical gown, where to wash my hands, I felt like a novitiate in some frantic, underground society.
This was a place of intense, concentrated activity, one of those places too densely crammed with sights and sounds for the newcomer to be able to perceive all of that with which he is being bombarded. It is a place bustling with people in hospital gowns, up to a dozen and a half nurses and ten doctors at a time, plus technicians and receptionists and custodians and visitors. Alarms sound routinely here, every minute or two, announcing that this baby’s heart rate is dropping, that that one has stopped breathing, that one of the dozens of intravenous lines has ceased to flow. Rock music churns in the background, syncopated by the buzz of phones. This is a page out of Brave New World, not a nursery.
Through this turmoil, Steve led me to our baby, a tiny red figure lying flat on his back, arms and legs splayed wide. “What a nice face he has,” I thought. Thick white tape obscured part of it, tape that was holding some of the tubes in place. His eyes were closed. But his features looked delicate and well formed, his eyes large and deep-set, his head covered with a fuzzy haze of red-gold hair. His face sustained me.
I could look at it and imagine what a strong and handsome face it might become, and somehow that allowed me not to see him coldly, objectively, as a three-month-premature baby, which is good, because that sight is one of the most pathetic, most heart-breaking in the world. Newborn premature babies look a lot like the babies starving in Africa, with their outsized heads and visible rib cages — except a very premature baby is so stunningly tiny. My son was one inch longer than a schoolkid’s ruler, and he weighed two pounds, five ounces.
He looked, on the one hand, astonishingly human, with tiny, perfect hands and toes, tiny, perfect fingernails and toenails. On the other hand, the machinery made him look like an alien creature. The tape on his face held in place a tube that ran into his mouth and down into his lungs, aiding with his breathing. Another tube, entering his nose, was used to suction secretions in his lungs. Five separate electronic probes,- some wider than his hand-span, were glued to his body, sensing his heartbeat, respiration, body temperature, and blood-oxygen levels. An intravenous line had been sewed into a blood vessel in his navel to act as a high-tech umbilical cord; blood samples would come out through this line while nutrients and fresh blood would enter him through it. Most pathetic of all were the cloth restraints that pinned his wrists to the bed, preventing him from grasping at the equipment which invaded him.
Somehow all the machinery seemed to siphon attention away from the baby. The machinery was lively, flashing numbers and emitting noises; the baby, on the other hand, lay as still as something washed up from the sea, half drowned. Steve and the baby’s nurse eagerly explained to me each machine’s function, and not long after they had finished, it seemed time to return to my hospital room at Sharp. Adrenaline buoyed us; I felt amazed that both the baby and I were alive. I also felt warmed every time a friend would call and congratulate us (instead of offering condolences). Although Steve and I had not expected to pick a name for another two months, we quickly settled upon “Michael.” It sounded strong and normal.
The next morning was a Monday. Steve had to work, so an aide wheeled me over to the NICU alone. This time at Michael’s bedside I found even more machinery and a cluster of people; someone explained that a cardiologist was using an ultrasound machine to examine the baby’s heart. As big as a small forklift, the machine squealed and panted like some demon, while complex waves pulsed on various screens. Only the cardiologist and her assistant were paying any attention to the testing — I know that now — but at that moment it seemed as if a crowd of strangers was gaping at my baby’s innermost essence. No one ever should have seen this part of him, not even me, and I felt depthless sorrow.
Eventually the doctor and the ultra-sound machine completed their tasks, and finally I could pull up a stool and sit next to the baby. He lay on a mattress on a metal platform underneath electric coils that radiated heat. Sheets of clear plastic surrounded the platform to contain the warmth, but I could lift the plastic to touch him gently and talk to him. I tried this, said hello to him and asked him how he was doing, and suddenly I felt as if everyone in the room was watching me, witnessing my crude, blundering attempts to act like a mother. Every time I said something to Michael, waves of something like shame flooded me and I found myself compulsively sneaking glances all around me, to see who was looking. I wanted to hide, to take my baby and hide with him, and hold him, and instead it felt as if we both were naked and on display.
Gradually these feelings subsided. Within a day or two I began to learn how the doctors and nurses were talking about my baby, through the medium of the machines. Children’s Hospital's NICU has a policy whereby every parent of a child in intensive care may visit or telephone the unit at any time of the day or night, and as I began visiting and calling, the machines surrounding Michael gradually stopped being a shiny jumble of garbage and started taking on some individuality, like characters in a play. There were, for example, the “bili lights,” banks of blue-white light aimed at Michael, so bright that he had to be blindfolded. I learned that the bili lights were there because Michael had jaundice; that is, his immature liver was failing to break down a toxic substance in his blood called bilirubin. The lights were supposed to help his body break this down. We could tell how well this was working from daily tests of the bilirubin levels in his blood.
So when we called or visited, one of the questions we could ask was, “How is his bilirubin level today?” They could answer this question. They would say, “It was thirteen,” or, “It was eleven,” or, “It stayed the same — still nine.” We learned that when it reached seven or eight, the noxious bili lights would be taken away.
I learned about the respirator that was inserted down into Michael’s lungs within moments of his birth. Many premature babies need such assistance because their immature lungs lack surfactant, a fluid coating that keeps them from collapsing when they exhale; every breath then becomes a terrible struggle. Michael’s major respiratory problem, however, was a tendency to forget to breathe. This condition, called apnea, also is extremely common in premature babies; the centers in their brains that control breathing are simply immature. As explained to me, the respirator was giving Michael enough of a boost to insure that his body was getting enough oxygen.
I learned that the respirator had two important components. First, the nurses could adjust the percentage of oxygen that the machine was puffing into his lungs. Normal air is composed of twenty-one percent oxygen, but for many premature babies that isn’t enough. They need to breathe in a higher percentage of oxygen in order to wind up with enough in their blood. Some need as much as a hundred percent oxygen (a very bad situation, since too much oxygen is poisonous to humans; one common complication of breathing this much oxygen is eye damage, even blindness). Michael never needed much more than about thirty-five percent oxygen, and from hour to hour the nurses would try to decrease that amount (checking the oxygen levels in his blood to see if he was tolerating the weaning process).
The other variable of the respirator was the number of breaths per minute it could give to the baby — anywhere from 150 down to four. The constant goal was also to reduce this number, to wean the baby off the respirator entirely. So we could also always ask, “What percentage of oxygen is he getting?” and “How many breaths a minute?” These questions they could answer, with ease. But it didn’t take me long to figure out that there were some questions it would do no good to ask, not then. Will he be blind? Deaf? (We couldn’t even begin to test his sight and hearing for several weeks.) Will he be mentally retarded? Physically incapacitated? (It would be months if not years before we could make these predictions.) What emotional scars does it leave upon someone to come into the world three months early, to have one's first experiences of the world be those of prolonged suffering and pain?
Those questions haunted me, but if they had no answers, the answers we did receive the first two weeks were encouraging. Although the heart sonogram showed that one of the little blood vessels outside Michael's heart failed to close properly, treatment with a drug seemed to correct the problem within a few days. Better still, head scans revealed no signs that the trauma of birth had caused bleeding in his brain, a major cause of cerebral palsy. Five days after he was born, he somehow yanked the respirator tubes out of his lungs, and he did well without the breathing assistance. Eight days after his birth, one of the nurses let me wash him (with moistened cotton balls), and for the first time since his birth I heard him cry — miniature, high-pitched squeaks. The same nurse let me hold him inside the warmer, cradling in my arms his whole assembly of heaters and wires and gauges. Steve held the oxygen tube near his face, and Michael looked at me, his eyes as large and blue as those of the fetus in 2001. He grasped my finger with his tiny hand, and as I talked to him, he seemed calmer.
Within days he moved from the open warmer into an incubator (nowadays they call them isolettes). The nurses routinely began inserting a tube down into his stomach and giving him tiny amounts of the breast milk I was pumping — starting with a sixth of an ounce every three hours, and ever so gradually increasing the quantity. Two weeks after Michael’s birth, Dr. Johnsgard told us he thought Michael was doing “superbly.” We tried to tell ourselves not to relax, not to start to feel confident. But at night, after a couple of glasses of wine, we also started to talk about how a gentle birth probably wasn’t all that important, and how — if he survived the hospital unscathed — he might even be better off for having gotten this head start on the real world.
Things fell apart seventeen days after he was born. Once again he was forgetting to breathe. Often. Ten times, twelve times during an eight-hour shift.
This is what it was like when it happened. If you were standing by his side, and you knew what you were looking for, you would see a subtle change in his coloring. Instead of looking pink, he would start to appear pale, with a grayish cast around his mouth, his eyes, his fingernails. About this time, the electronic monitor next to him, which gave a constant read-out of his heartbeat and respirations, would begin to change, the heartbeat numbers dropping from 150 or so beats a minute to 120, 100, 90. An alarm would begin to shriek, and a nurse would walk over and open the portholes of his isolette. She would gently rub her fingers over his back, or pat his bottom, or if that weren't sufficient, she would snap her finger against the bottom of his feet. Invariably, this worked. You could see him take a deep breath and the pink glow would return.
In the NICU slang, these spells were “A’s and B’s,” for apnea (the failure to breathe), and bradycardia (the slowing of the heartbeat that usually accompanied the apnea). And so the pattern of our daily questions changed. “How many A’s and B’s did he have?” became the first thing out of our mouths. Some eight-hour shifts would pass with one or two, then he'd have six, seven, nine. We’d been warned that this might happen, warned that time and time again a tiny preemie would do splendidly for a week or two, then would seem to tire out and would once again need the machine to help him breathe. Warnings cannot adequately prepare one for such a setback, and depression engulfed both of us. I wept daily. But after a week of watching Michael’s struggle, of watching him turn dusky over and over again. I felt almost relieved when on December 11, twenty-four days after he was born, he went back on the respirator once again.
The next day he looked visibly pinker and more rested. The day after that he looked awful, with a 102-degree fever, his stomach distended. The staff began to fear he might have contracted some hospital-bred infection and so they began a grueling series of tests: of his blood, his urine, his spinal fluid. The next five days he steadily improved, then at 7:30 one morning we received a call from the neonatologist on duty in the NICU. He told us that during the night Michael’s heartbeat had begun dropping — and the nurse couldn’t rouse him. until finally the team had taken out the respirator tube and replaced it with another one. Perhaps the first tube had gotten clogged with mucus (completely cutting off Michael’s air supply) or perhaps some other problem was developing. We would have to wait and see. With that incident, Michael went from needing six ventilations per minute of room air to twenty breaths per minute of air containing fifty-five percent oxygen.
Slowly, painstakingly, the weaning process began again. Steve and I spent Christmas Eve and part of Christmas Day in the NICU. Our best present came the day after Christmas, when the staff judged that once again Michael was ready to try breathing unassisted. He weighed three pounds, two and a half ounces. Steve and I had been told that someday, before he could come home, he would probably move over to the less-intense “special care nursery” at Sharp Hospital. But the day Michael came off the respirator for the second time, we couldn’t imagine his ever leaving the NICU.
I often marvel at how quickly human beings adjust to their environments. In a few weeks, the NICU had become as familiar as home, which is strange, considering that it has to rank as one of the most unnatural places in the world. Here people, in effect, are growing babies in artificial wombs. Here there is no day or night. The bright lights shine ceaselessly, and when we question whether that’s good for the babies, the staff responds that they need to see whether the babies are changing color, a much better indication of distress than any machine. The noise of the telephones and the alarms combines with radio station B-100. I wondered if classical music might not be better for the babies, but I held my tongue; aggressive, hard-driving rock seemed so appropriate for the NICU nurses.
Over the weeks, I met dozens upon dozens of these young women (and all were women, and most were young, just as all five of Children’s staff neonatologists are middle-age men). Michael seemed to have three new nurses (one for each shift) every day. Some were chatty and some were impassive. Some were aloof, though a much higher percentage were so maternal and sympathetic that their warmth would bring tears to my eyes. Far more striking than their differences, however, were the things they had in common. Like air traffic controllers, they thrived on having three things to do at any given moment, in an atmosphere of imminent crisis. Because they have to make minute-by-minute decisions, the NICU nurses work more independently of doctors than nurses in other areas of medicine. They are far more important in the lives of their tiny charges than are the babies’ own parents, and I think the nurses know this, and like it.
If the nurses are the front-line troops of the NICU, hopped up and elbow-deep in the mundanities of caring for very tiny, very sick babies, the neonatologists are the generals. Once a day they and various other key medical personnel would float from one isolette to the next, pondering each baby’s case, making strategic decisions in a manner that looked calm and measured and judicious (parents were required to retreat to some distance during these “rounds”). The vast majority of the time I talked not with the neonatologists but with one of the three nurse-clinicians, Donna Brandon. Brandon was more like a diplomat than a soldier. She knew what the neonatologists were planning, and she could work shoulder-to-shoulder with the nurses, but she also was our main source of information about Michael’s overall status. Almost every day I besieged her with dozens of questions, and she answered them patiently. Slowly, day by day, I began to get an insight into the frontiers of medicine, of how imprecise it is, how dependent upon trial and error — of how, even when something “works,” how many questions never get answered.
One day I had another insight into modern American medicine. It suddenly struck me that this experience in the NICU was the only time in my life I’d ever been in a place where everyone acted as if the cost of things were irrelevant. Almost everything, no matter how shiny and sturdy-looking, was used once and thrown away, or so it seemed. No one ever so much as mentioned the price of anything — be it alcohol wipes or brain scans — because price was never a consideration in whether to do something. Not that I wanted to know what Michael’s care was costing us. Steve’s private insurance covered everything except the first $1500, but it still terrified me utterly to hear what those expenses were; the hospital bill alone — not including doctors’ fees — for just the first nine days was more than $25,000. Other babies who lacked private insurance were substantially covered by state and federal funds. Steve commented that the NICU was the most democratic place he’d ever known; here you could find a Mexican farmworker’s baby next to a La Jolla lawyer’s baby, both receiving the most sophisticated medical care on earth, administered by people to whom money seemed to be no object.
We guessed that some of the other parents were farmworkers, though we never knew for sure. Throughout all the weeks, we never really got to know any of the other parents. I yearned to talk to some of them; it seemed as though no one could really understand what I was experiencing except for someone in the same position. But we never made the connections; we weren't there at the same times or were too shy to step up and introduce ourselves. But even though the other parents were shadowy figures, flitting in and out of the background, their babies were always there, and Steve and I talked about them daily, and came to care about them. The nurses and the doctors all knew what was wrong with each baby, but they didn’t share the daily news with us; some unspoken code seemed to proscribe this. Still, Steve and I could read the posted names of the babies located near Michael, and by eavesdropping on the nurses, we got a vague idea of which were seriously ill, which were thriving.
All the books about premature babies I was reading warned me not to compare Michael with the other babies, but the comparisons were inevitable. For weeks upon weeks it seemed as if he were the tiniest baby in sight; baby after baby moved in, stayed for a few days, then moved out, while we remained. Then one day in early January I came in to find a new baby occupying the open warmer next to Michael’s isolette. He was a boy twenty-six or twenty-seven weeks (gestational age), and he weighed two and a half pounds — very close to what Michael had been. Seven and a half weeks had passed since Michael’s birth — and already it was hard for me to believe that Michael had ever looked so raw, so horribly fragile, like a broken baby bird. That day, weighing four pounds and two ounces, my son looked plump, even robust, and I knew that soon we would be leaving the NICU.
It actually took two more weeks, time in which Michael began learning to drink my breast milk from a bottle (instead of having the nurses pour it into his stomach through a tube). Laboriously he would suck half an ounce and fall asleep. He would choke, turn blue, set off the heart alarms. It took nine days to get him to consume his full quota: one and one-third ounces. Four days later we got permission for him to feed at my breast for the first time; and later that day Michael once again rode in a “transport incubator” through the corridors that connect Children’s with Sharp Hospital, where he checked into the special care nursery.
I hated the Sharp nursery that first day. I didn’t recognize any of the nurses, didn’t know to whom I could turn for information. The place seemed sterile and tomblike. Being there reminded me of what had happened when we were there two months earlier. I was forced to relive the trauma of Michael’s birth.
But it took only a day or two for me to see that I had grown addicted to the maelstrom of the NICU, that the Sharp nursery — clean, quiet, orderly — was a much better place for babies. Here, if all went well, Michael only would need to practice drinking his meals orally to grow a little plumper.
All didn’t go well. Five days after entering the Sharp nursery, Michael’s skin suddenly began looking as if it had been washed with a yellow stain. Tests showed that his blood contained a very high level of bilirubin. Once again he had jaundice. But unlike the jaundice that had afflicted him immediately after birth, this jaundice was frightening. Michael’s liver wasn't working properly, and this time the doctors didn’t know why. Once again the neonatologists were demanding blood, urine. Once again they ordered ultrasound tests, and then they called in more doctors, specialists in baby gastrointestinal systems. The experts ordered yet more exotic tests; technicians injected radioactive particles into one of Michael’s veins and watched a screen to see that the particles passed through the liver and out into his bile tracts.
The doctors finally concluded that Michael’s liver probably had been irritated by some of the intravenous fluids he had been given in the NICU. This happened fairly often, about fifteen percent of the time, and Michael’s jaundice would probably just go away, they guessed. Since his bottle feedings were improving, suddenly everyone was talking about when to discharge him. We picked him up from the hospital February 16, two days short of his due date. He was five pounds, four ounces, and three months old.
It took twenty minutes to drive from Children’s Hospital to our home, but it took months to leave the hospital behind. Weeks passed before I could bring myself to stop keeping hourly records, like a nurse, of everything from Michael’s temperature to his bowel movements. It took me even longer to stop worrying obsessively about every single milliliter of milk he failed to consume; not until we finally switched over to complete breast-feeding was I able to begin to relax, as Michael steadily gained weight. We Came home from the hospital with a rented machine that monitored his heartbeats and respirations. Every night we connected Michael to it with a soft rubber belt which we fastened around his chest with Velcro tabs. When three and a half months passed with no significant apnea spells, we finally returned the monitor. Recently Michael went back to the hospital for day surgery on a hernia, another ailment that commonly plagues preemies. The scar from that is fast fading.
Other signs of his experience will take longer to recede. X-rays of his lungs still show some mild damage, but unlike adults, babies can grow new lung tissue, and we expect that Michael’s should heal by the time he’s two years old. Another legacy of Michael’s prematurity visible to sharp observers is the shape and size of his head, large in comparison to the rest of his body and flattened on the sides (by the pressure of lying on the sides for three months, instead of being supported uniformly in the womb). Michael also still is very small, though our pediatrician thinks he will catch up to the normal size range by the end of this year. He cried and fretted throughout most of his first months at home; preemies are notable for their early irritability.
At the same time, we’ve been so lucky. His eyesight and hearing seem to be fine, and he’s been very healthy. The jaundice has disappeared. He’s an alert, bright-eyed baby who smiles readily, huge delighted grins that brighten up the whole room. He’s active and vigorous and he’s doing most of the things done by babies his age (minus three months): reaching for and gumming things, creeping and rolling over, babbling.
It will be years before we can definitively answer whether Michael’s prematurity has hurt his development. The scientific studies that exist aren’t much help in making predictions. For one thing, there aren’t a whole lot of them; just ten years ago, most babies born three months early simply died. One of the major studies that have been done indicates that only about five percent of very early, very small preemies suffer severe developmental handicaps — but many (an additional thirty-five percent) develop milder problems such as learning and behavioral disorders, lack of physical coordination, or hyperactivity. To complicate things still further, a host of factors appear to influence the odds, including everything from the parents’ socioeconomic levels to whether or not the baby was on a respirator.
I never asked that one nurse in the NICU why she would let her (hypothetical) premature baby die, but I assume she had to be thinking of all the things that can (and do) go wrong. I know she was aware of how nightmarishly, horribly wrong things become once in a while, as they had for one of the NICU’s little patients. Born only two months prematurely, he had progressed quite well until he had developed an infection that put him back on the respirator, whereupon his lung disease failed to improve. For a year and a half. At eighteen months, he had spent his entire life in the NICU, and was still on a respirator. When Michael was there, this baby’s family members were preparing themselves for the homecoming of the little boy — and all his medical equipment, including the breathing machine.
Another nurse, whose mother was a social worker specializing in the mentally retarded, told me that her mother had never forgiven her for choosing to work with the tiny preemies. “She says, ‘Your patients today are my clients in the future,’ “ the nurse said. When Michael was still in the hospital and I didn’t know if he would be mentally retarded, when I didn’t know if he too would develop some infection that would lead to chronic lung disease, I seethed at the circumstances that had trapped Steve and me into facing such terrifying prospects.
But what would I have done differently, even if someone had been brutally honest with me, had said, “Once you enter that hospital, they’re going to cut you open and take your baby away from you for a very long time, and when they finally give him back there’s at least a forty percent chance he’ll be damaged”? Even if I had known that, I don’t see how I could have stayed home and delivered Michael alone, to die. And once I was in the hospital, how could the doctors have acted differently? Not knowing precisely what the consequences of their interventions might be, how could they do other than to employ their skills and hope for the best? I’ve been thinking about this ever since Michael was born, and I don’t have any other answers. Technology has forced us to play these games with these babies’ lives,yet at every turn we have only one move.
Since Michael’s birth, several friends and acquaintances have called him a “miracle baby.” Every time I hear the phrase, I squirm. Miracles are supposed to be instantaneous and inexplicable and free. What we lived through cost more than a quarter of a million dollars and involved three months of round-the-clock care by dozens of people who were among the most skilled, dedicated, and hard-working I’ve ever known. There are other times, too, however, when I’m holding Michael close to me and he looks at me with his big blue eyes and his face lights up and I am overcome with love. Then I think maybe I don’t know the meaning of the word miracle.
Comments