 Facebook
Facebook
 X
X
 Instagram
Instagram
 TikTok
TikTok
 Youtube
Youtube
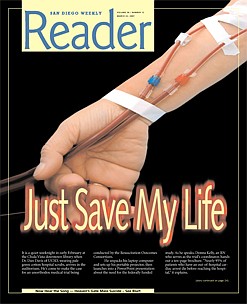
It is a quiet weeknight in early February at the Chula Vista downtown library when Dr. Dan Davis of UCSD, wearing pale green cotton hospital scrubs, arrives in the auditorium. He's come to make the case for an unorthodox medical trial being conducted by the Resuscitation Outcomes Consortium. He unpacks his laptop computer and sets up his portable projector, then launches into a PowerPoint presentation about the need for the federally funded study.
As he speaks, Donna Kelly, an RN who serves as the trial's coordinator, hands out a ten-page brochure. "Nearly 95% of patients who have an out-of-hospital cardiac arrest die before reaching the hospital," it explains cardiac arrest, unlike the odds on old TV shows such as Emergency, are daunting, Dr. Davis tells his Chula Vista audience. In the words of the brochure: "Someone must recognize the arrest, call 911 to summon the EMS providers, and perform CPR promptly (ideally before the EMS providers arrive). The EMS providers or trained lay rescuers must be able to provide defibrillation or other therapies if needed."
Surprising though it may seem to many, the state of emergency medical knowledge, according to Davis, is still pretty primitive. As the brochure says, "Many existing and proposed therapies have not received rigorous scientific evaluation in the prehospital setting."
Then Davis gets to the reason he has come. There are new, still experimental ways for paramedics to combine CPR and the use of defibrillators -- devices that check for a heartbeat and shock a stopped heart back to life -- that might improve those dismal survival rates. There's also a compact plastic device, a valve that attaches to the air tube or facemask of a patient with cardiac arrest. During CPR, the valve "creates a small vacuum inside the patient's chest, which increases the return flow of blood to the heart," according to a news release from the Resuscitation Outcomes Consortium -- ROC for short. But the doctors don't know for sure that the device improves the odds. Like all of the experimental procedures, it has yet to be fully tested on humans.
The cardiac trial is ROC's second study. The first, which began in San Diego County in mid-February, involves saline solution given trauma patients -- victims of traffic accidents, gunshot, or falls who have suffered massive blood loss, which can quickly lead to brain death.
Conducting a scientific test involves arbitrarily giving one kind of treatment to some patients and another kind to others, decided in a random manner, much like flipping a coin.
For instance, giving one cardiac patient a three-minute period of CPR between shocks and giving another only 30 seconds first. The "standard of care" for the past 15 years has been to go quickly to the defibrillator, but some doctors believe the longer period of CPR prior to defibrillation may be more effective.
Or, in the case of the saline study, giving one trauma patient the normal saline solution (.9 percent salt concentration) and giving another either a high-concentration (7.5 percent, referred to as hypertonic) saline solution or high-concentration saline with dextran, a circulation-enhancing substance.
The studies are "blinded," meaning that the paramedics who administer the treatment do not know the kind of saline solution they are using or whether the plastic airway device works or instead is a dummy model. With enough carefully recorded random attempts, a pattern might emerge that would validate one treatment over the other.
In most medical experiments, the subjects are well enough to decide if they want to participate. Trauma victims and people in cardiac arrest usually aren't; in fact, they are unconscious.
But someone has to be the guinea pig -- at least that's the idea behind the Resuscitation Outcomes Consortium. The Food and Drug Administration has exempted ROC from the usual requirement that experimental subjects furnish their "informed consent" prior to being enrolled in a study in which they may not receive the current standard of care.
In the ROC trials, paramedics in cities across the country have been given special training, equipped with hypertonic saline solution and the plastic airway devices, and provided with a way to randomize treatment on all of their runs.
Thus, every member of the general public, potentially, is fair game.
Initial funding for the Resuscitation Outcomes Consortium is $50 million. The consortium, which comprises 11 centers throughout the United States and Canada, including one in San Diego County, will eventually conduct multiple trials on various cardiac and trauma resuscitation techniques. The University of Washington in Seattle, ROC's Clinical Trial Center, is coordinating the consortium. For its part, UCSD is getting an initial $2.3 million from the project's principal sponsor, the government-run National Institutes of Health.
In exchange for the exemption from the informed-consent requirement, ROC and its participating medical schools and hospitals are required to minimize risk as much as possible.
They are also supposed to spread the word to the public that the experiments are taking place. According to the theory under which the Food and Drug Administration exemption was granted, once the citizenry is apprised of the "risk-benefit ratio" and given the option not to participate by wearing a wristband, the study has met its ethical obligations.
But turning that theory into practice is problematic. Dr. Davis's Chula Vista appearance, part of the university's so-called outreach effort, is a case in point: his audience is composed of just three people. Two are journalists; the third is a friend of one of the writers. One reporter leaves halfway through the talk.
Looking around the virtually empty auditorium to which he has been speaking for almost 90 minutes, Davis says that the study doesn't have enough money for lots of TV spots and other expensive ways of reaching people; despite that hurdle, he insists, the university is trying to get the word out.
But the story is more complicated than that. Though Davis mentions it only fleetingly, the city of San Diego, which was expected to provide many of the subjects for the trials, is not taking part. It quietly opted out last fall after Mayor Jerry Sanders and his staff vetoed a previous agreement to participate.
A vigorous, behind-the-scenes debate between the mayor's office and UCSD then ensued about the merits and risks of the trial -- a discussion that, had it been conducted in public rather than behind closed doors, would doubtless have been of interest to San Diegans.
E-mails obtained under the state Public Records Act show that from the very beginning of the university's attempt to gain the mayor's favor, researchers were shadowed by controversy from another UCSD trial involving an experimental blood substitute called PolyHeme.
As with the ROC study, the rules of the PolyHeme trial did not require that its subjects -- trauma victims who were comatose -- give their consent to the procedure, the infusion of PolyHeme, a concoction of synthetic hemoglobin and other ingredients that its proponents maintained would be better than saline solution at saving lives in the minutes before patients reached the hospital and received regular blood.
In the PolyHeme trial, which began in San Diego in May 2004, small plastic bags of the blood substitute developed by the trial's sponsor, Northfield Laboratories of Evanston, Illinois, were deployed in three of the city of San Diego's poorest neighborhoods on paramedic trucks: Oak Park's Medic 26, San Ysidro's Medic 29, and Nestor's Medic 62, as well as at the downtown fire station. Other paramedic units in the county and an air medical transportation service were also enrolled in the study.
The reason for restricting the initial deployment in the city of San Diego to the three low-income neighborhoods was that Northfield had provided UCSD with only limited supplies of the substance, according to a May 2003 e-mail by study coordinator Beth Romeril.
But neither UCSD nor San Diego officials ever made public the specific locations of PolyHeme deployment within the city. Instead, the university issued a press release, took out small newspaper advertisements to announce the trial, and held a public briefing in August 2003 at University Hospital in Hillcrest. It also provided plastic bracelets to be worn by people who did not wish to be given the blood substitute.
The trial received brief mentions on several TV news broadcasts and a March 23, 2004 story in the Union-Tribune headlined "A new hope for saving of lives," in which Dr. David Hoyt, then trauma director at UCSD Medical Center and principal investigator for the San Diego part of the study, touted the substance's potential and downplayed its risks.
But for those seeking to know how the trial was proceeding, the university was tight-lipped. It refused to provide information regarding the well-being of the subjects participating, arguing that doing so would violate a trade secret agreement it had signed with Northfield, the project's sponsor.
One example of the information gap was a heavily redacted letter dated August 26, 2004, from Daniel Masys, MD, then director of UCSD's Human Research Protections Program, to Hoyt concerning an "adverse event" -- a serious complication or death -- encountered by one of the study subjects and reported to the university's Institutional Review Board, a group set up under federal law to review the ethics and integrity of the university's medical research.
"Your July 22, 2004 adverse event report for Project 030443 has been reviewed and accepted by the IRB Committee at the August 2004 meeting. This report concerns the following subject: 1)."
The description that followed, describing the cause of the incident and what happened to the patient, was blacked out by the university. Hundreds of other documents requested by a reporter under the state's Public Records Act were similarly censored on the grounds that making them public would violate patient privacy or reveal Northfield's trade secrets.
And though UCSD repeatedly insisted that it wanted the public to be fully aware of the PolyHeme study and the ethical issues it raised, a June 21, 2005 e-mail showed that Romeril and Kelly, the coordinator of the upcoming ROC trials, were wary of fielding pointed media inquiries.
"Could you send me the name of the reporter that has been asking about PolyHeme and now ROC," wrote Kelly to Romeril. "I saw [Dr.] Danny Davis today and wanted him to know that this person was out there asking questions about ROC and PolyHeme with a history of stirring up trouble. He wanted more information i.e. what newspaper, what has he written in the past, 'have you googled him' etc.
"I just wanted Dan to be aware that if someone does start asking questions that he be sure that the intent was sincere and not malicious. Dan was more of the impression that reporting to the media was not necessarily a bad thing. I agree but would prefer it be in a good light with positive spin rather than someone just looking for dirt to stir up."
Romeril replied the same day: "The reporter is Matt Potter, an 'investigative reporter' for the Reader here in town. You can look at the Reader web site to see stories he has had printed in the past -- they tend to be long, wandering exposé types about possible corruption in city government....
"He is not a science or medical reporter and he is definitely not looking for good news to share. Also be aware that there are legally binding confidentiality agreements in place with Northfield regarding this study, and rest assured we will be sued (by Northfield) if we breach that contract, so check with them before saying anything to a reporter!"
Concluded Romeril: "In general, media attention is not a bad thing; in fact Channel 10 is planning a follow-up piece for some time in July. Dr. Hoyt will be interviewed for that again. The problem with Mr. Potter is that he seems to be on a fishing expedition and just wants carte blanche access to all sorts of study files etc. without giving any kind of reason or explanation as to what it is he is looking for...does not inspire confidence in his motives!"
A month later, in a brief July 2005 interview, Hoyt defended the PolyHeme trial, saying that it was safe for its subjects and fully compliant with federal regulations that cover drug trials involving lack of informed consent. He also minimized the adverse event report, but he would not describe what had happened to the patient.
Hoyt acknowledged that alerting residents of the low-income and minority neighborhoods where PolyHeme was deployed within the city of San Diego "wasn't something we specifically considered" in complying with the government's requirement for public notice. The limited deployment was the university's way of dealing with a "cost containment problem," he explained, and poor people or minorities were not deliberately targeted.
UCSD abruptly ended its role in the PolyHeme trial in the spring of last year, saying that it needed to clear the decks for the Resuscitation Outcomes Consortium program. "As previously planned, due to preparation for the ROC trials, UC San Diego Medical Center and Scripps Mercy Hospital will no longer be able to enroll PolyHeme study participants as of Friday April 21st 2006," Hoyt wrote in an April 18 e-mail.
"The PolyHeme will be collected up over the next few days and there will be no more available to the medics as of Thursday afternoon. The study itself will continue for another month by other sites. We would like to thank everyone who has helped to get this trial done as it was not easy and we appreciate all the efforts it took to do it." On June 30, Hoyt left UCSD to become chairman of surgery at UC Irvine's medical school, handing the reins of ROC to his colleague, Dr. Dan Davis.
Six months later, Northfield Laboratories announced the first results of its PolyHeme study, and the news was not good. "Blood substitute 'a disaster' in trial," said a December 20, 2006 headline in the Chicago Tribune. Of the trauma subjects who received PolyHeme, 13.2 percent died, versus 9.6 percent of those who received the standard saline solution. No details about where or when the deaths had occurred were provided.
"If you look at the absolute number of deaths, it kills more patients than saline does," observed Martin Shkreli, a hedge-fund manager at New York-based Elea Capital who was following the ups and downs of Northfield stock.
Steven Gould, Northfield's chief executive officer, blamed protocol errors made by researchers in the various trials around the country and said that further number-crunching would show that PolyHeme benefited patients. He said the company still planned to submit the product for federal approval sometime this year.
Critics, however, have been pounding the company and the federal government for allowing the trials to occur in the first place. The most formidable opponent is Charles E. Grassley, the powerful Republican senator from Iowa.
In a letter last March to the Food and Drug Administration, Grassley wrote, "I am personally troubled that, for all intents and purposes, the FDA allowed a clinical trial to proceed, which makes the inhabitants of 32 communities in 18 states...potential 'guinea pigs,' without their consent." He demanded that Food and Drug Administration policies be changed to forbid such trials in the future.
Grassley's criticism came at an inopportune time for UCSD. The university was attempting to persuade the City of San Diego and its new mayor, Jerry Sanders, that the ROC studies should be conducted using city paramedic rigs. Two years before, during the administration of Mayor Dick Murphy, the City had agreed to participate, but the new mayor's people had questions.
The university had a formidable point man in Dr. James Dunford, a popular faculty member of the UCSD medical school who is also employed as the medical director of the city's Emergency Medical Services.
In an April 25, 2006 e-mail to his UCSD colleagues, Dunford outlined a plan to go public about ROC's first study, the saline trial, and to deal up front with its exemption from the Food and Drug Administration's requirement of informed consent. He would arrange to "meet with Jill Olin, the new Deputy COO, Public Safety and Homeland Security -- Jill will need to give the idea her ok and then take it to Mayor Sanders before it can go to the Council's PSNS [Public Safety and Neighborhood Services] Committee."
The same day, after a morning meeting, ROC administrator Donna Kelly sent an e-mail to Dunford and others. "PSNS will need an initial notification that we are planning to do a county wide community notification and consultation for the [hypertonic saline] trial," she said.
"Jim is going to be in touch with Brian Mineshine (sp.) [San Diego city councilman Brian Maienschein] to determine how to proceed with the PSNS for the initial intro that we are going to be doing this followed by a more formal presentation after the IRB [Institutional Review Board] approves it."
But the council hearing didn't happen. Instead, Dunford became mired in a series of meetings with Sanders and his staff. At his first session with Olen on May 24, he seemed to appreciate the lingering credibility problems that the controversies enveloping the PolyHeme study had created for the university.
"I underscored the lessons learned from PolyHeme and a commitment to adapt and improve our processes of community outreach," Dunford wrote in a May 24, 2006 e-mail to his UCSD colleagues.
"I did inform her of the concerns that Senator Grassley has expressed with the FDA regarding (in particular) the inpatient aspects of the PolyHeme trial," Dunford added. "While it was agreed that ROC might bring prestige to the City this was felt to be distinctly less important than tangible benefits (or risks).
"As I have previously mentioned, it is clear that the City is not in the same position it was when it originally enthusiastically endorsed our ROC application several years ago. Cost and risk:benefit are major concerns confronting city leaders every day, and ROC will be similarly assessed."
A month later, Dunford was beginning to sound impatient. "I am waiting to hear back from the Mayor's office regarding ROC, having submitted a letter of explanation 10 [days] ago that I believe was compelling as to why they should support ROC," he said in a June 22 e-mail to Kelly. "I will be following up next week if I do not hear back before then....
"Lastly, remember it is not the City Council that 1st determines the worthiness of this or any big issue in the City -- it is the Mayor's office," Dunford added. "Now that the city has adopted a 'strong mayor' form of government, the City Council only becomes involved if the Mayor's policy advisors recommend something...this is a big change since January. I am quite optimistic we will be all right."
"I will have to get used to the new mayor's office business process," replied Kelly. "Glad to hear you have a new SD Fire Chief and that she will be a supporter of our efforts."
Throughout the summer, UCSD anxiously awaited a final decision. On July 6, according to a July 20 message from Dunford to San Diego Fire Chief Tracy Jarman, Dunford had talked to Olen again, and "Jill informed me the issue was still under review."
In July 2006, UCSD received the results of an $18,000 public opinion survey it had commissioned earlier that year. The study, conducted for the university by Bellevue, Washington-based Herbert Research, polled 502 San Diego County residents over the telephone. Before they began asking questions, the pollsters told respondents that the current state of the art for emergency medical treatment was bleak and that the experimental treatments prescribed by the study were largely risk-free.
"Currently, very few cardiac arrest victims survive to be discharged from the hospital, and many patients with serious traumatic injuries die in the field or hospital," respondents were told. "All of the experimental ways of treating cardiac arrest and trauma victims that are being considered have appeared safe in animal and small human studies," the pollsters added.
Respondents were then asked a series of questions, including whether they would want to be included in the hypertonic saline study "without providing consent if there was a one in three chance of dying with standard treatment." To that, 74.3 percent said yes, 19.7 percent said no, and 6 percent responded, "Don't know/Refused."
Regarding the second trial of experimental treatment for cardiac arrest, respondents were asked whether they would want to participate without their prior consent "if there was less than a 10 percent chance of surviving with standard treatment." Given those slim odds, 84.3 percent said yes, 13.5 percent said no, and 2.2 percent responded, "Don't know/Refused."
In the words of one person interviewed by the pollsters: "The options are pretty grim, so why not try! Try anything as long as it's not black magic!" The study's sponsors soon began thinking of ways to use the poll to lobby the Sanders team. "How should we approach the Mayor's office with this overwhelming mandate?" Davis wrote Dunford on July 14. The poll was not released to the public.
In late July, Sara Steinhoffer, UCSD's manager of Public Affairs and Community Relations, e-mailed Dr. Dan Davis and UCSD Institutional Review Board administrator Michael Caligiuri. "And just so we are all on the same page, on Friday I left the press release with the aide to San Diego City Councilmember Donna Frye and asked him to call if she had any questions. She had initially raised concerns with the PolyHeme trial."
But Sanders's participation seemed to be growing more uncertain. "I have been in a bunch of meetings and press conferences this summer with the mayor and he is a great guy with vision," Dunford wrote Dr. David Hoyt, by then chairman of UC Irvine medical school's Department of Surgery but still cochair for trauma on the ROC steering committee.
"The issue is that his leadership team is almost exclusively focused on the $1.5 billion pension problem & its enormous implications. I'm concerned they might decide we're not essential to the immediate needs no matter how good the idea."
Later in the same message, dated August 27, Dunford voiced other worries. "Even if the mayor gives his endorsement, we may still have to take it to [city council] committees like public safety where it would be debated, so the process could take longer yet."
Dunford then complained that few local government officials were willing to go public with their backing of the potentially controversial experiments, even if they privately backed the idea.
"What's frustrating is the county EMS folks can't give a formal endorsement to ROC. I think that would be the single biggest assist we could have right now. But when I spoke with [county EMS director] Bruce Haynes about it he said they wouldn't be able to give much assistance officially, even though he has said openly that he supports ROC. It's another example of the county [Health and Human Services Agency] attempting to smother strong medical direction, in my opinion."
(Haynes responded to Dunford's criticism last week, saying by phone, "I'm not sure of the context of that e-mail, but it may have had to do with wanting the county to go to the city as an advocate for [ROC], and I'm not sure that that was our role." He added, "I know Jim has strong feelings about good medical [direction] and everything, but it's not been my experience with regard to the ROC or anything else that the county is trying to squelch or impair medical [direction]. It's not been my experience at all."
(Haynes said that the county EMS office's decision to approve the ROC deployment had never been brought to the board of supervisors at a full public hearing, though aides of individual supervisors had been briefed privately. "I don't think there was any request that the board formally act on it -- it just didn't seem like something they needed to do.")
On the afternoon of September 5, 2006, after Dunford had lobbied the city for months, the ceiling fell in. Maurice Luque, public information officer for the San Diego Fire-Rescue Department, e-mailed Dunford. The subject: "no go for ROC." "Jim: I don't know if you've heard about this officially or not," wrote Luque, "but unofficially ROC is a no go. Call me and I can fill you in."
Based on their subsequent reaction, Dunford and his UCSD colleagues were caught by surprise. They appeared unable to believe that Mayor Sanders's decision was final and began a behind-the-scenes campaign to pressure him into changing his mind.
On September 11, Dunford fired off an e-mail to mayoral aide Cynthia Lewis. "I would appreciate an opportunity to speak with Mayor Sanders regarding a recent decision that would prevent our City from participating in the National Institutes of Health's prestigious Resuscitation Outcomes Consortium (ROC). As the City's EMS Medical Director, I believe this federally-sponsored program would enhance the health of our citizens for years to come."
One message illustrated the secretive nature of the university's efforts to overturn the mayor's verdict. "I have been working with Melanie in Assemblymember Saldana's office on the hearing and mentioned your contact," wrote Sara Steinhoffer, UCSD's manager of Public Affairs and Community Relations, to UCSD's Dr. Dan Davis in a September 13 e-mail.
"I shared with her that we have not received official word from the Mayor/City that their position on ROC participation has changed and that therefore it would be premature for that office to make inquiries. I thanked them for their interest and told them I would keep them apprised.
"This is a delicate matter on several fronts, so let's stay consistent and internal to the greatest extent possible."
The mayor wasn't the only source of worry. On September 15, 2006, Institutional Review Board administrator Michael Caligiuri dispatched an e-mail to Dan Davis and his associates saying that the office of University of California president Robert Dynes "has recently expressed concern over potential third party liability associated with" the saline trial. "The [hypertonic saline] trial is unique in that there are no subcontracts between UCSD and the participating hospitals that would normally spell out conditions of indemnification of the parties involved," wrote Caligiuri.
"A solution is needed that: 1) protects the study participant from costs associated with research-related injury and that this is clearly disclosed in the consent form; 2) clarifies the responsibilities of UCSD and the participating non-UCSD entities, including hospitals, EMT personnel, etc. throughout the study period; and 3) satisfies 1 and 2 above in an efficient manner without further delay in study approval."
Dunford made a personal pitch to Sanders on Tuesday morning, September 19. Two days later, on the morning of September 21, Dunford sent an e-mail to Olen. "The person about whom I referred Tuesday AM in our meeting with Mayor Sanders as the prime military 'mover' for ROC is Colonel John Holcolm, MD, FACS. John is the Commander and Director of the U.S. Army Institute for Surgical Research, Fort Sam Houston, TX. I've met John previously and he is a terrific individual."
Dunford went on to list other doctors who he said would vouch for the trials and their safety. "I would be glad to arrange for any of these folks to speak with our City leaders to provide assurance of safety and allay concerns about risk."
But despite intense university lobbying, Sanders did not change his mind. That afternoon, Dunford e-mailed Olen asking for an audience with her. "I called Ronne Froman's office to see if I might be able to help sort through the ROC issue. Ronne informed me that a decision had been made this morning and that you would be the person with whom I should speak....
"After 8 years in this position, I thought I had a pretty good handle on what would be best to improve cardiac arrest and trauma care for San Diego," said Dunford. "I need to regroup now, and would like to know where the leadership team wants me to direct my energy since ROC will no longer be on the radar screen."
On September 24, an e-mail from Dr. Dan Davis appealed to Sanders and Olen. "While I was aware that some specific issues had been identified that would need to be addressed, I had no idea that the non-participation of San Diego Fire Department was being considered," said Davis in his e-mail to the pair. "The withdrawal of San Diego from the ROC project will threaten our site's ability to fulfill our commitment to the NIH, Department of Defense, and American Heart Association."
On September 26, Dunford sent an e-mail to a colleague, relaying the bad news. "I spoke with Mayor Sanders 1 week ago, providing my recommendation that the City maintain its commitment to participate in ROC," Dunford related. "As you might imagine, the University is concerned about the potential impact of the City's decision on this landmark NIH grant and the future of funding to the region."
A week later, Davis was still trying. "Please let me know if you'd like to meet at some point to go over some details regarding ROC and how it might affect the city," Davis wrote in an October 8 e-mail to Jill Olen. "You might conclude that it would be less disruptive to participate than to withdraw, given the amount of preparation and infrastructure development."
He presented a list of training services and equipment that he said the study would provide the city for free, then added, "And that's not to mention the disaster training opportunities and high quality education provided by me as study PI principal investigator."
Olen replied the next day: "Dan -- the decision not to participate in ROC at this time has been made. No further discussion needs to be held."
On December 8, Dunford e-mailed Karen Wentworth of the American Heart Association, a cosponsor of the project. "The NIH was understandably upset by this development and has told UCSD it should do whatever it can to grow the site (over 1/2 the expected patient recruitment was to have come from the City)...to that end Dr. Dan Davis has been communicating with Orange County's acting EMSA Medical Director to expand up there ASAP."
(UCSD medical school spokeswoman Leslie Franz said that Davis would not respond to questions unless university officials vetted them first. Even then, she made clear, there was no assurance Davis would be allowed by the university to be questioned by a reporter. Read portions of the documents over the phone last week, Franz said she would call back to further discuss the matter but did not. Davis did not respond to repeated messages left with his office and on his voice mail line. Dunford also did not return repeated phone calls.)
(At city hall, Fred Sainz, the mayor's press secretary, did not return phone calls. Olen's secretary said she was traveling outside the country and was not available for comment.)
Meanwhile, things weren't going all that smoothly for the saline portion of the study, which was preparing for launch in Chula Vista, National City, and other parts of the county outside the city of San Diego.
On October 26, local investigators got word that the Food and Drug Administration had halted the study. "The FDA has just informed the CTC [Clinical Trial Center] that the HS [hypertonic saline] trial is on clinical hold," said an e-mail from Berit Bardarson, a trauma nurse consultant working for the study at the University of Washington in Seattle. "ALL ENROLLMENT INTO THE HS TRIAL MUST BE SUSPENDED IMMEDIATELY."
From Portland, Oregon, Jerris Hedges e-mailed the same day: "Portland is pulling the investigational fluid off the EMS units. We hope to have this complete by this weekend."
ROC spokeswoman Judy Powell, reached by phone last week at her office in Seattle, explained that the Food and Drug Administration temporarily called a halt to the trial because it wanted "more intensive monitoring." Specifically, the agency concluded that follow-up blood tests of patients enrolled in the experiment were not being conducted uniformly at all trial sites. "The initial schedule was whatever the doctor at each location ordered," Powell said. "The FDA wanted a standard of three blood draws within each 24-hour period, and that has now been implemented."
Regarding other details of the study, Powell is more reticent. "There have been expected adverse events," she acknowledges, but as to the number and character of such incidents, "I can't tell you that right now." None of the events, which have been reviewed by the Food and Drug Administration and ROC's data safety management committee, has been directly related to the study, she said. Members of the public interested in knowing more will have to wait until the publication of scientific papers about the trial's outcome, not expected for several years.

It is a quiet weeknight in early February at the Chula Vista downtown library when Dr. Dan Davis of UCSD, wearing pale green cotton hospital scrubs, arrives in the auditorium. He's come to make the case for an unorthodox medical trial being conducted by the Resuscitation Outcomes Consortium. He unpacks his laptop computer and sets up his portable projector, then launches into a PowerPoint presentation about the need for the federally funded study.
As he speaks, Donna Kelly, an RN who serves as the trial's coordinator, hands out a ten-page brochure. "Nearly 95% of patients who have an out-of-hospital cardiac arrest die before reaching the hospital," it explains cardiac arrest, unlike the odds on old TV shows such as Emergency, are daunting, Dr. Davis tells his Chula Vista audience. In the words of the brochure: "Someone must recognize the arrest, call 911 to summon the EMS providers, and perform CPR promptly (ideally before the EMS providers arrive). The EMS providers or trained lay rescuers must be able to provide defibrillation or other therapies if needed."
Surprising though it may seem to many, the state of emergency medical knowledge, according to Davis, is still pretty primitive. As the brochure says, "Many existing and proposed therapies have not received rigorous scientific evaluation in the prehospital setting."
Then Davis gets to the reason he has come. There are new, still experimental ways for paramedics to combine CPR and the use of defibrillators -- devices that check for a heartbeat and shock a stopped heart back to life -- that might improve those dismal survival rates. There's also a compact plastic device, a valve that attaches to the air tube or facemask of a patient with cardiac arrest. During CPR, the valve "creates a small vacuum inside the patient's chest, which increases the return flow of blood to the heart," according to a news release from the Resuscitation Outcomes Consortium -- ROC for short. But the doctors don't know for sure that the device improves the odds. Like all of the experimental procedures, it has yet to be fully tested on humans.
The cardiac trial is ROC's second study. The first, which began in San Diego County in mid-February, involves saline solution given trauma patients -- victims of traffic accidents, gunshot, or falls who have suffered massive blood loss, which can quickly lead to brain death.
Conducting a scientific test involves arbitrarily giving one kind of treatment to some patients and another kind to others, decided in a random manner, much like flipping a coin.
For instance, giving one cardiac patient a three-minute period of CPR between shocks and giving another only 30 seconds first. The "standard of care" for the past 15 years has been to go quickly to the defibrillator, but some doctors believe the longer period of CPR prior to defibrillation may be more effective.
Or, in the case of the saline study, giving one trauma patient the normal saline solution (.9 percent salt concentration) and giving another either a high-concentration (7.5 percent, referred to as hypertonic) saline solution or high-concentration saline with dextran, a circulation-enhancing substance.
The studies are "blinded," meaning that the paramedics who administer the treatment do not know the kind of saline solution they are using or whether the plastic airway device works or instead is a dummy model. With enough carefully recorded random attempts, a pattern might emerge that would validate one treatment over the other.
In most medical experiments, the subjects are well enough to decide if they want to participate. Trauma victims and people in cardiac arrest usually aren't; in fact, they are unconscious.
But someone has to be the guinea pig -- at least that's the idea behind the Resuscitation Outcomes Consortium. The Food and Drug Administration has exempted ROC from the usual requirement that experimental subjects furnish their "informed consent" prior to being enrolled in a study in which they may not receive the current standard of care.
In the ROC trials, paramedics in cities across the country have been given special training, equipped with hypertonic saline solution and the plastic airway devices, and provided with a way to randomize treatment on all of their runs.
Thus, every member of the general public, potentially, is fair game.
Initial funding for the Resuscitation Outcomes Consortium is $50 million. The consortium, which comprises 11 centers throughout the United States and Canada, including one in San Diego County, will eventually conduct multiple trials on various cardiac and trauma resuscitation techniques. The University of Washington in Seattle, ROC's Clinical Trial Center, is coordinating the consortium. For its part, UCSD is getting an initial $2.3 million from the project's principal sponsor, the government-run National Institutes of Health.
In exchange for the exemption from the informed-consent requirement, ROC and its participating medical schools and hospitals are required to minimize risk as much as possible.
They are also supposed to spread the word to the public that the experiments are taking place. According to the theory under which the Food and Drug Administration exemption was granted, once the citizenry is apprised of the "risk-benefit ratio" and given the option not to participate by wearing a wristband, the study has met its ethical obligations.
But turning that theory into practice is problematic. Dr. Davis's Chula Vista appearance, part of the university's so-called outreach effort, is a case in point: his audience is composed of just three people. Two are journalists; the third is a friend of one of the writers. One reporter leaves halfway through the talk.
Looking around the virtually empty auditorium to which he has been speaking for almost 90 minutes, Davis says that the study doesn't have enough money for lots of TV spots and other expensive ways of reaching people; despite that hurdle, he insists, the university is trying to get the word out.
But the story is more complicated than that. Though Davis mentions it only fleetingly, the city of San Diego, which was expected to provide many of the subjects for the trials, is not taking part. It quietly opted out last fall after Mayor Jerry Sanders and his staff vetoed a previous agreement to participate.
A vigorous, behind-the-scenes debate between the mayor's office and UCSD then ensued about the merits and risks of the trial -- a discussion that, had it been conducted in public rather than behind closed doors, would doubtless have been of interest to San Diegans.
E-mails obtained under the state Public Records Act show that from the very beginning of the university's attempt to gain the mayor's favor, researchers were shadowed by controversy from another UCSD trial involving an experimental blood substitute called PolyHeme.
As with the ROC study, the rules of the PolyHeme trial did not require that its subjects -- trauma victims who were comatose -- give their consent to the procedure, the infusion of PolyHeme, a concoction of synthetic hemoglobin and other ingredients that its proponents maintained would be better than saline solution at saving lives in the minutes before patients reached the hospital and received regular blood.
In the PolyHeme trial, which began in San Diego in May 2004, small plastic bags of the blood substitute developed by the trial's sponsor, Northfield Laboratories of Evanston, Illinois, were deployed in three of the city of San Diego's poorest neighborhoods on paramedic trucks: Oak Park's Medic 26, San Ysidro's Medic 29, and Nestor's Medic 62, as well as at the downtown fire station. Other paramedic units in the county and an air medical transportation service were also enrolled in the study.
The reason for restricting the initial deployment in the city of San Diego to the three low-income neighborhoods was that Northfield had provided UCSD with only limited supplies of the substance, according to a May 2003 e-mail by study coordinator Beth Romeril.
But neither UCSD nor San Diego officials ever made public the specific locations of PolyHeme deployment within the city. Instead, the university issued a press release, took out small newspaper advertisements to announce the trial, and held a public briefing in August 2003 at University Hospital in Hillcrest. It also provided plastic bracelets to be worn by people who did not wish to be given the blood substitute.
The trial received brief mentions on several TV news broadcasts and a March 23, 2004 story in the Union-Tribune headlined "A new hope for saving of lives," in which Dr. David Hoyt, then trauma director at UCSD Medical Center and principal investigator for the San Diego part of the study, touted the substance's potential and downplayed its risks.
But for those seeking to know how the trial was proceeding, the university was tight-lipped. It refused to provide information regarding the well-being of the subjects participating, arguing that doing so would violate a trade secret agreement it had signed with Northfield, the project's sponsor.
One example of the information gap was a heavily redacted letter dated August 26, 2004, from Daniel Masys, MD, then director of UCSD's Human Research Protections Program, to Hoyt concerning an "adverse event" -- a serious complication or death -- encountered by one of the study subjects and reported to the university's Institutional Review Board, a group set up under federal law to review the ethics and integrity of the university's medical research.
"Your July 22, 2004 adverse event report for Project 030443 has been reviewed and accepted by the IRB Committee at the August 2004 meeting. This report concerns the following subject: 1)."
The description that followed, describing the cause of the incident and what happened to the patient, was blacked out by the university. Hundreds of other documents requested by a reporter under the state's Public Records Act were similarly censored on the grounds that making them public would violate patient privacy or reveal Northfield's trade secrets.
And though UCSD repeatedly insisted that it wanted the public to be fully aware of the PolyHeme study and the ethical issues it raised, a June 21, 2005 e-mail showed that Romeril and Kelly, the coordinator of the upcoming ROC trials, were wary of fielding pointed media inquiries.
"Could you send me the name of the reporter that has been asking about PolyHeme and now ROC," wrote Kelly to Romeril. "I saw [Dr.] Danny Davis today and wanted him to know that this person was out there asking questions about ROC and PolyHeme with a history of stirring up trouble. He wanted more information i.e. what newspaper, what has he written in the past, 'have you googled him' etc.
"I just wanted Dan to be aware that if someone does start asking questions that he be sure that the intent was sincere and not malicious. Dan was more of the impression that reporting to the media was not necessarily a bad thing. I agree but would prefer it be in a good light with positive spin rather than someone just looking for dirt to stir up."
Romeril replied the same day: "The reporter is Matt Potter, an 'investigative reporter' for the Reader here in town. You can look at the Reader web site to see stories he has had printed in the past -- they tend to be long, wandering exposé types about possible corruption in city government....
"He is not a science or medical reporter and he is definitely not looking for good news to share. Also be aware that there are legally binding confidentiality agreements in place with Northfield regarding this study, and rest assured we will be sued (by Northfield) if we breach that contract, so check with them before saying anything to a reporter!"
Concluded Romeril: "In general, media attention is not a bad thing; in fact Channel 10 is planning a follow-up piece for some time in July. Dr. Hoyt will be interviewed for that again. The problem with Mr. Potter is that he seems to be on a fishing expedition and just wants carte blanche access to all sorts of study files etc. without giving any kind of reason or explanation as to what it is he is looking for...does not inspire confidence in his motives!"
A month later, in a brief July 2005 interview, Hoyt defended the PolyHeme trial, saying that it was safe for its subjects and fully compliant with federal regulations that cover drug trials involving lack of informed consent. He also minimized the adverse event report, but he would not describe what had happened to the patient.
Hoyt acknowledged that alerting residents of the low-income and minority neighborhoods where PolyHeme was deployed within the city of San Diego "wasn't something we specifically considered" in complying with the government's requirement for public notice. The limited deployment was the university's way of dealing with a "cost containment problem," he explained, and poor people or minorities were not deliberately targeted.
UCSD abruptly ended its role in the PolyHeme trial in the spring of last year, saying that it needed to clear the decks for the Resuscitation Outcomes Consortium program. "As previously planned, due to preparation for the ROC trials, UC San Diego Medical Center and Scripps Mercy Hospital will no longer be able to enroll PolyHeme study participants as of Friday April 21st 2006," Hoyt wrote in an April 18 e-mail.
"The PolyHeme will be collected up over the next few days and there will be no more available to the medics as of Thursday afternoon. The study itself will continue for another month by other sites. We would like to thank everyone who has helped to get this trial done as it was not easy and we appreciate all the efforts it took to do it." On June 30, Hoyt left UCSD to become chairman of surgery at UC Irvine's medical school, handing the reins of ROC to his colleague, Dr. Dan Davis.
Six months later, Northfield Laboratories announced the first results of its PolyHeme study, and the news was not good. "Blood substitute 'a disaster' in trial," said a December 20, 2006 headline in the Chicago Tribune. Of the trauma subjects who received PolyHeme, 13.2 percent died, versus 9.6 percent of those who received the standard saline solution. No details about where or when the deaths had occurred were provided.
"If you look at the absolute number of deaths, it kills more patients than saline does," observed Martin Shkreli, a hedge-fund manager at New York-based Elea Capital who was following the ups and downs of Northfield stock.
Steven Gould, Northfield's chief executive officer, blamed protocol errors made by researchers in the various trials around the country and said that further number-crunching would show that PolyHeme benefited patients. He said the company still planned to submit the product for federal approval sometime this year.
Critics, however, have been pounding the company and the federal government for allowing the trials to occur in the first place. The most formidable opponent is Charles E. Grassley, the powerful Republican senator from Iowa.
In a letter last March to the Food and Drug Administration, Grassley wrote, "I am personally troubled that, for all intents and purposes, the FDA allowed a clinical trial to proceed, which makes the inhabitants of 32 communities in 18 states...potential 'guinea pigs,' without their consent." He demanded that Food and Drug Administration policies be changed to forbid such trials in the future.
Grassley's criticism came at an inopportune time for UCSD. The university was attempting to persuade the City of San Diego and its new mayor, Jerry Sanders, that the ROC studies should be conducted using city paramedic rigs. Two years before, during the administration of Mayor Dick Murphy, the City had agreed to participate, but the new mayor's people had questions.
The university had a formidable point man in Dr. James Dunford, a popular faculty member of the UCSD medical school who is also employed as the medical director of the city's Emergency Medical Services.
In an April 25, 2006 e-mail to his UCSD colleagues, Dunford outlined a plan to go public about ROC's first study, the saline trial, and to deal up front with its exemption from the Food and Drug Administration's requirement of informed consent. He would arrange to "meet with Jill Olin, the new Deputy COO, Public Safety and Homeland Security -- Jill will need to give the idea her ok and then take it to Mayor Sanders before it can go to the Council's PSNS [Public Safety and Neighborhood Services] Committee."
The same day, after a morning meeting, ROC administrator Donna Kelly sent an e-mail to Dunford and others. "PSNS will need an initial notification that we are planning to do a county wide community notification and consultation for the [hypertonic saline] trial," she said.
"Jim is going to be in touch with Brian Mineshine (sp.) [San Diego city councilman Brian Maienschein] to determine how to proceed with the PSNS for the initial intro that we are going to be doing this followed by a more formal presentation after the IRB [Institutional Review Board] approves it."
But the council hearing didn't happen. Instead, Dunford became mired in a series of meetings with Sanders and his staff. At his first session with Olen on May 24, he seemed to appreciate the lingering credibility problems that the controversies enveloping the PolyHeme study had created for the university.
"I underscored the lessons learned from PolyHeme and a commitment to adapt and improve our processes of community outreach," Dunford wrote in a May 24, 2006 e-mail to his UCSD colleagues.
"I did inform her of the concerns that Senator Grassley has expressed with the FDA regarding (in particular) the inpatient aspects of the PolyHeme trial," Dunford added. "While it was agreed that ROC might bring prestige to the City this was felt to be distinctly less important than tangible benefits (or risks).
"As I have previously mentioned, it is clear that the City is not in the same position it was when it originally enthusiastically endorsed our ROC application several years ago. Cost and risk:benefit are major concerns confronting city leaders every day, and ROC will be similarly assessed."
A month later, Dunford was beginning to sound impatient. "I am waiting to hear back from the Mayor's office regarding ROC, having submitted a letter of explanation 10 [days] ago that I believe was compelling as to why they should support ROC," he said in a June 22 e-mail to Kelly. "I will be following up next week if I do not hear back before then....
"Lastly, remember it is not the City Council that 1st determines the worthiness of this or any big issue in the City -- it is the Mayor's office," Dunford added. "Now that the city has adopted a 'strong mayor' form of government, the City Council only becomes involved if the Mayor's policy advisors recommend something...this is a big change since January. I am quite optimistic we will be all right."
"I will have to get used to the new mayor's office business process," replied Kelly. "Glad to hear you have a new SD Fire Chief and that she will be a supporter of our efforts."
Throughout the summer, UCSD anxiously awaited a final decision. On July 6, according to a July 20 message from Dunford to San Diego Fire Chief Tracy Jarman, Dunford had talked to Olen again, and "Jill informed me the issue was still under review."
In July 2006, UCSD received the results of an $18,000 public opinion survey it had commissioned earlier that year. The study, conducted for the university by Bellevue, Washington-based Herbert Research, polled 502 San Diego County residents over the telephone. Before they began asking questions, the pollsters told respondents that the current state of the art for emergency medical treatment was bleak and that the experimental treatments prescribed by the study were largely risk-free.
"Currently, very few cardiac arrest victims survive to be discharged from the hospital, and many patients with serious traumatic injuries die in the field or hospital," respondents were told. "All of the experimental ways of treating cardiac arrest and trauma victims that are being considered have appeared safe in animal and small human studies," the pollsters added.
Respondents were then asked a series of questions, including whether they would want to be included in the hypertonic saline study "without providing consent if there was a one in three chance of dying with standard treatment." To that, 74.3 percent said yes, 19.7 percent said no, and 6 percent responded, "Don't know/Refused."
Regarding the second trial of experimental treatment for cardiac arrest, respondents were asked whether they would want to participate without their prior consent "if there was less than a 10 percent chance of surviving with standard treatment." Given those slim odds, 84.3 percent said yes, 13.5 percent said no, and 2.2 percent responded, "Don't know/Refused."
In the words of one person interviewed by the pollsters: "The options are pretty grim, so why not try! Try anything as long as it's not black magic!" The study's sponsors soon began thinking of ways to use the poll to lobby the Sanders team. "How should we approach the Mayor's office with this overwhelming mandate?" Davis wrote Dunford on July 14. The poll was not released to the public.
In late July, Sara Steinhoffer, UCSD's manager of Public Affairs and Community Relations, e-mailed Dr. Dan Davis and UCSD Institutional Review Board administrator Michael Caligiuri. "And just so we are all on the same page, on Friday I left the press release with the aide to San Diego City Councilmember Donna Frye and asked him to call if she had any questions. She had initially raised concerns with the PolyHeme trial."
But Sanders's participation seemed to be growing more uncertain. "I have been in a bunch of meetings and press conferences this summer with the mayor and he is a great guy with vision," Dunford wrote Dr. David Hoyt, by then chairman of UC Irvine medical school's Department of Surgery but still cochair for trauma on the ROC steering committee.
"The issue is that his leadership team is almost exclusively focused on the $1.5 billion pension problem & its enormous implications. I'm concerned they might decide we're not essential to the immediate needs no matter how good the idea."
Later in the same message, dated August 27, Dunford voiced other worries. "Even if the mayor gives his endorsement, we may still have to take it to [city council] committees like public safety where it would be debated, so the process could take longer yet."
Dunford then complained that few local government officials were willing to go public with their backing of the potentially controversial experiments, even if they privately backed the idea.
"What's frustrating is the county EMS folks can't give a formal endorsement to ROC. I think that would be the single biggest assist we could have right now. But when I spoke with [county EMS director] Bruce Haynes about it he said they wouldn't be able to give much assistance officially, even though he has said openly that he supports ROC. It's another example of the county [Health and Human Services Agency] attempting to smother strong medical direction, in my opinion."
(Haynes responded to Dunford's criticism last week, saying by phone, "I'm not sure of the context of that e-mail, but it may have had to do with wanting the county to go to the city as an advocate for [ROC], and I'm not sure that that was our role." He added, "I know Jim has strong feelings about good medical [direction] and everything, but it's not been my experience with regard to the ROC or anything else that the county is trying to squelch or impair medical [direction]. It's not been my experience at all."
(Haynes said that the county EMS office's decision to approve the ROC deployment had never been brought to the board of supervisors at a full public hearing, though aides of individual supervisors had been briefed privately. "I don't think there was any request that the board formally act on it -- it just didn't seem like something they needed to do.")
On the afternoon of September 5, 2006, after Dunford had lobbied the city for months, the ceiling fell in. Maurice Luque, public information officer for the San Diego Fire-Rescue Department, e-mailed Dunford. The subject: "no go for ROC." "Jim: I don't know if you've heard about this officially or not," wrote Luque, "but unofficially ROC is a no go. Call me and I can fill you in."
Based on their subsequent reaction, Dunford and his UCSD colleagues were caught by surprise. They appeared unable to believe that Mayor Sanders's decision was final and began a behind-the-scenes campaign to pressure him into changing his mind.
On September 11, Dunford fired off an e-mail to mayoral aide Cynthia Lewis. "I would appreciate an opportunity to speak with Mayor Sanders regarding a recent decision that would prevent our City from participating in the National Institutes of Health's prestigious Resuscitation Outcomes Consortium (ROC). As the City's EMS Medical Director, I believe this federally-sponsored program would enhance the health of our citizens for years to come."
One message illustrated the secretive nature of the university's efforts to overturn the mayor's verdict. "I have been working with Melanie in Assemblymember Saldana's office on the hearing and mentioned your contact," wrote Sara Steinhoffer, UCSD's manager of Public Affairs and Community Relations, to UCSD's Dr. Dan Davis in a September 13 e-mail.
"I shared with her that we have not received official word from the Mayor/City that their position on ROC participation has changed and that therefore it would be premature for that office to make inquiries. I thanked them for their interest and told them I would keep them apprised.
"This is a delicate matter on several fronts, so let's stay consistent and internal to the greatest extent possible."
The mayor wasn't the only source of worry. On September 15, 2006, Institutional Review Board administrator Michael Caligiuri dispatched an e-mail to Dan Davis and his associates saying that the office of University of California president Robert Dynes "has recently expressed concern over potential third party liability associated with" the saline trial. "The [hypertonic saline] trial is unique in that there are no subcontracts between UCSD and the participating hospitals that would normally spell out conditions of indemnification of the parties involved," wrote Caligiuri.
"A solution is needed that: 1) protects the study participant from costs associated with research-related injury and that this is clearly disclosed in the consent form; 2) clarifies the responsibilities of UCSD and the participating non-UCSD entities, including hospitals, EMT personnel, etc. throughout the study period; and 3) satisfies 1 and 2 above in an efficient manner without further delay in study approval."
Dunford made a personal pitch to Sanders on Tuesday morning, September 19. Two days later, on the morning of September 21, Dunford sent an e-mail to Olen. "The person about whom I referred Tuesday AM in our meeting with Mayor Sanders as the prime military 'mover' for ROC is Colonel John Holcolm, MD, FACS. John is the Commander and Director of the U.S. Army Institute for Surgical Research, Fort Sam Houston, TX. I've met John previously and he is a terrific individual."
Dunford went on to list other doctors who he said would vouch for the trials and their safety. "I would be glad to arrange for any of these folks to speak with our City leaders to provide assurance of safety and allay concerns about risk."
But despite intense university lobbying, Sanders did not change his mind. That afternoon, Dunford e-mailed Olen asking for an audience with her. "I called Ronne Froman's office to see if I might be able to help sort through the ROC issue. Ronne informed me that a decision had been made this morning and that you would be the person with whom I should speak....
"After 8 years in this position, I thought I had a pretty good handle on what would be best to improve cardiac arrest and trauma care for San Diego," said Dunford. "I need to regroup now, and would like to know where the leadership team wants me to direct my energy since ROC will no longer be on the radar screen."
On September 24, an e-mail from Dr. Dan Davis appealed to Sanders and Olen. "While I was aware that some specific issues had been identified that would need to be addressed, I had no idea that the non-participation of San Diego Fire Department was being considered," said Davis in his e-mail to the pair. "The withdrawal of San Diego from the ROC project will threaten our site's ability to fulfill our commitment to the NIH, Department of Defense, and American Heart Association."
On September 26, Dunford sent an e-mail to a colleague, relaying the bad news. "I spoke with Mayor Sanders 1 week ago, providing my recommendation that the City maintain its commitment to participate in ROC," Dunford related. "As you might imagine, the University is concerned about the potential impact of the City's decision on this landmark NIH grant and the future of funding to the region."
A week later, Davis was still trying. "Please let me know if you'd like to meet at some point to go over some details regarding ROC and how it might affect the city," Davis wrote in an October 8 e-mail to Jill Olen. "You might conclude that it would be less disruptive to participate than to withdraw, given the amount of preparation and infrastructure development."
He presented a list of training services and equipment that he said the study would provide the city for free, then added, "And that's not to mention the disaster training opportunities and high quality education provided by me as study PI principal investigator."
Olen replied the next day: "Dan -- the decision not to participate in ROC at this time has been made. No further discussion needs to be held."
On December 8, Dunford e-mailed Karen Wentworth of the American Heart Association, a cosponsor of the project. "The NIH was understandably upset by this development and has told UCSD it should do whatever it can to grow the site (over 1/2 the expected patient recruitment was to have come from the City)...to that end Dr. Dan Davis has been communicating with Orange County's acting EMSA Medical Director to expand up there ASAP."
(UCSD medical school spokeswoman Leslie Franz said that Davis would not respond to questions unless university officials vetted them first. Even then, she made clear, there was no assurance Davis would be allowed by the university to be questioned by a reporter. Read portions of the documents over the phone last week, Franz said she would call back to further discuss the matter but did not. Davis did not respond to repeated messages left with his office and on his voice mail line. Dunford also did not return repeated phone calls.)
(At city hall, Fred Sainz, the mayor's press secretary, did not return phone calls. Olen's secretary said she was traveling outside the country and was not available for comment.)
Meanwhile, things weren't going all that smoothly for the saline portion of the study, which was preparing for launch in Chula Vista, National City, and other parts of the county outside the city of San Diego.
On October 26, local investigators got word that the Food and Drug Administration had halted the study. "The FDA has just informed the CTC [Clinical Trial Center] that the HS [hypertonic saline] trial is on clinical hold," said an e-mail from Berit Bardarson, a trauma nurse consultant working for the study at the University of Washington in Seattle. "ALL ENROLLMENT INTO THE HS TRIAL MUST BE SUSPENDED IMMEDIATELY."
From Portland, Oregon, Jerris Hedges e-mailed the same day: "Portland is pulling the investigational fluid off the EMS units. We hope to have this complete by this weekend."
ROC spokeswoman Judy Powell, reached by phone last week at her office in Seattle, explained that the Food and Drug Administration temporarily called a halt to the trial because it wanted "more intensive monitoring." Specifically, the agency concluded that follow-up blood tests of patients enrolled in the experiment were not being conducted uniformly at all trial sites. "The initial schedule was whatever the doctor at each location ordered," Powell said. "The FDA wanted a standard of three blood draws within each 24-hour period, and that has now been implemented."
Regarding other details of the study, Powell is more reticent. "There have been expected adverse events," she acknowledges, but as to the number and character of such incidents, "I can't tell you that right now." None of the events, which have been reviewed by the Food and Drug Administration and ROC's data safety management committee, has been directly related to the study, she said. Members of the public interested in knowing more will have to wait until the publication of scientific papers about the trial's outcome, not expected for several years.
Comments